Journal of Addiction & Prevention
Download PDF
Maladaptive schemas and cognitions, such as inaccurate assessments of the impacts of alcohol use, may also play a significant role in treatment outcomes such as abstinence after completion of treatment [53]. Many inpatient and outpatient programs provide psycho-education to counter cognitions influencing alcohol use, and one study focused on beliefs about alcohol as a predictor of abstinence post-treatment [47]. Although positive alcohol beliefs are consistently associated with alcohol use, 53 male clients at a 10-day inpatient program who had positive alcohol expectancies did not consume more alcohol at the 1-month follow up. At the 3-month follow up, however, negative alcohol expectancies influenced a reduction in alcohol consumption, possibly indicating the importance of modifying cognitions associated with substance use in treatment programs. This study did not examine longer-term abstinence and so it is uncertain if this theoretical approach is more widely applicable.
Mini Review
*Address for Correspondence: Peter Silverstone, MB. BS, MD, FRCPC, ICD.D, Professor, Department of Psychiatry, University of Alberta, 1E7.17 Mackenzie Centre 8114 -112 Street, Edmonton, Alberta, Canada, Tel: +1-780-407-6576; Fax +1-780-407-6672; E-mail: peter.silverstone@ualberta.ca
Citation: Hamza DM, Silverstone PH. In the Treatment of Alcohol Abuse there are No Clear Differences in Outcomes between Inpatient Treatment and Outpatient Programs. J Addiction Prevention. 2015;3(1): 9.
Copyright © 2015 Hamza DM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 3, Issue: 1
Submission: 16 December, 2014 | Accepted: 07 February, 2015 | Published: 11 February, 2015
Some inpatient programs utilize directed learning and structured daily routine or provide a holistic program known as the therapeutic community (TC), in addition to care as usual [22]. Most inpatient facilities include education specific to substance use, such as relapse management, for shorter periods of care (between 1-3 months), while inpatient TC approach incorporates psycho education in other social dimensions, such as assertiveness training, for longer-term care (ranging from 3–12 months) [22,23]. This longer period of inpatient care allows clients to participate in the management and operation of the facility encouraging collaboration and mutual support skills within a prosocial environment.
In the Treatment of Alcohol Abuse there are No Clear Differences in Outcomes between Inpatient Treatment and Outpatient Programs
Deena M. Hamza and Peter H. Silverstone*
- Department of Psychiatry, University of Alberta, Edmonton, Canada
*Address for Correspondence: Peter Silverstone, MB. BS, MD, FRCPC, ICD.D, Professor, Department of Psychiatry, University of Alberta, 1E7.17 Mackenzie Centre 8114 -112 Street, Edmonton, Alberta, Canada, Tel: +1-780-407-6576; Fax +1-780-407-6672; E-mail: peter.silverstone@ualberta.ca
Citation: Hamza DM, Silverstone PH. In the Treatment of Alcohol Abuse there are No Clear Differences in Outcomes between Inpatient Treatment and Outpatient Programs. J Addiction Prevention. 2015;3(1): 9.
Copyright © 2015 Hamza DM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 3, Issue: 1
Submission: 16 December, 2014 | Accepted: 07 February, 2015 | Published: 11 February, 2015
Abstract
Alcohol use disorder has serious implications including increased risk of violence, motor vehicle collisions, and criminal activity. Treatment can be given in an inpatient/residential setting or in an outpatient/day-treatment setting. Given the significantly lower costs of the latter approach it is important to determine if there are differences in outcomes between these. However, one of the issues is that treatment programs vary greatly in many areas including duration, care setting, goal intensity, and amount of psycho-education. It is perhaps unsurprising, therefore, that research into differences between inpatient/residential and outpatient/day-treatment programs have produced conflicting results. Previous reviews have not determined a clear beneficial outcome for either approach, but have noted significant methodological issues which have limited the ability to potentially identify clear differences. Since there are significant cost differences between these approaches, and there has been a marked switch away from inpatient/residential programs for this reason, it is important to examine the recent literature to determine if these conclusions have changed. The primary finding from the current analysis is that there remains a marked lack of good outcome studies in this area. Issues include lack of details on many potential aspects that my affect outcome, such as the roles of age, gender, severity and nature of abuse, presence of co morbidity, and program details. From the limited literature available the only consistent finding is that, in general, longer-term programs are more successful than shorter-term programs for both inpatient/residential and outpatient/day-treatment settings. Future research is still needed to determine which program factors, such as goal intensity, care structure, psycho-education, therapeutic alliance, social and human capital, and the inclusion of an education program, actually affect outcomes. The rather dispiriting conclusion is that despite the huge impact of these conditions, the large sums being spent to address them, and recommendations for many years for the need for improved research regarding this issue, our knowledge regarding the most effective types of treatment for Alcohol use disorder remains limited. Perhaps the only conclusion possible at this time is that longer programs are likely to be more effective.Keywords
Alcohol abuse; Residential; Inpatient; Outpatient; Location; TherapyIntroduction
Substance use disorders, including alcohol use, significantly affect personal health and compromise public safety [1,2]. Population surveys indicate that between 39% and 50% of adults engage in hazardous alcohol use, contributing to a number of social issues (such as violence, crime, motor vehicle collisions and toxicity) and an estimated 3.3 million deaths annually [3,4]. Despite the magnitude of the problem, most do not receive treatment. Thus, of the estimated 20 million identified cases of alcohol use disorders in the Unites States, less than 20% receive treatment in any year, and treatment is thought to be inadequate in many cases [5]. Further, treatment programs for alcohol use disorders in the United States are estimated to cost over $7 billion annually [6]. Similar costs occur in Europe [7]. Research has attempted to identify those characteristics of treatment programs that best predict long-term recovery, and outcome measures have included engagement, affiliation, retention in treatment, compliance to treatment, and evidence of sustained remission and/or abstinence [8-12].Treatment for alcohol use disorders occurs in two settings: inpatient/residential and outpatient/day-treatment situations. In large part because of the significant additional costs of inpatient/residential programs there has been a marked switch in service provision towards outpatient/day treatment programs. For example, in the United States the proportion of programs offering residential treatment over a 12-year period (1990–2002) decreased from 55% of care to 10% [13]. Previous comprehensive literature reviews have supported this since they did not find differences between approaches [14,16], particularly on the most appropriate outcome measure, namely the probability of abstinence at 12-months post-treatment [17,18].
Since the provision of the most effective type of care has important clinical and policy implications for the treatment of individuals with alcohol use disorders, it is important to continue to determine what the current research evidence shows in terms of what are the key elements in current approaches, duration of care, goal intensity, care structure, psycho education, social alliance, therapeutic and human capital, and the 12-step approach. In particular, it is important to examine these factors in the context of inpatient/residential approaches versus outpatient/day-treatment approaches. While the terms are often used interchangeably [19], in the present article the term “inpatient” will be used to refer to alcohol use treatment programs in which the individual is removed from their primary environment and required to reside in the care facility. Therefore, outpatient care encompasses programs offering treatment with individuals returning to their primary environment each evening, or upon completion of the session and includes day-treatment programs.
However, when reviewing these aspects of treatment it needs to be clarified that, overall, the quality of the literature is quite limited. There remain multiple methodological issues which have been repeatedly pointed out in previous reviews [5,14,16]. These include a lack of detail regarding such items as effects of age and sex, the details of the alcohol-use and its severity and chronicity, and if there are other comorbid conditions. These qualifications regarding the overall quality of the data should be recognized when considering the findings that are available.
Methods
Multiple databases were searched for appropriate publications, including: PsycINFO; Pub Med; Health Sciences: JSTOR: Journals@Ovid Full Text; and SAGE Journals Online and Psychology. Additionally, a manual search of publications that had the words “Alcohol” or “Addictions” in the titles was carried out. Keywords searched for were outpatient, inpatient, substance use, day hospital, inpatient care, 12-step, treatment, remission, abstinence, alcohol use disorder, Alcoholics Anonymous, and recovery. The search was then limited to articles published from 1992 to December 2013 focusing on alcohol use disorders. Additionally, internet-based searches were performed to identify potentially relevant publications that were not published in the peer-reviewed manner.Comparison between inpatient care with outpatient care
Key elements of inpatient and outpatient care: Inpatient programs are heterogeneous and care facilities may differ on theoretical underpinnings, duration of treatment, intensity, care setting and level of commitment. The universal feature of specialized long-term inpatient care programs for alcohol uses the removal from the primary environment, to restructure social and physical surroundings which will support successful recovery [20,21]. Inpatient care may be provided within a hospital or clinical setting, or inpatient care facility (Figure 1). Care in hospital settings may include medically assisted detoxification and management of withdrawal symptoms [21]. Inpatient hospital-based care is best suited for individuals who are at high risk of developing life-threatening withdrawal symptoms, have severe psychiatric conditions or are in need of 24-hour medical supervision [20]. For individuals without these conditions, inpatient treatment in non-hospital settings provides structure and intense programming without an emphasis on medical stabilization. Unlike hospital-based care, inpatient facilities may require a period of abstinence before acceptance into the program. It has been suggested that inpatient programs are best suited for individuals who experience chronic relapses, are dependent, or do not have good social environmental support [20,22]. There is also considerable evidence that those with severe alcohol use disorders benefit the most from intense monitoring [6,16,20,23].
Figure 1: Inpatient care settings. This shows the inpatient care programs and how they may link to residential care, as well as the differences in concept in most cases. While not the case in all studies, in general there are significant differences between approaches in an inpatient setting compared to a residential setting.
However, it needs to be recognized that the year following treatment requires considerable life changes as the individual shifts from inpatient care that provides a safe and secure environment to independence in the “real-world” with potential alcohol use triggers. Relapse rates are often noted to be more prevalent within this 12-month transition period with nearly 60-80% of individuals relapsing within 3-4 months after leaving an inpatient program, indicating the importance of long-term care including aftercare programming. A potential barrier influencing relapse rates in aftercare programming may be caused by internal or structural obstacles preventing commitment and active participation [24]. The transition from inpatient care to less structured aftercare approaches requires individuals, who may be in the process of developing human capital (i.e. abstinence self-efficacy, or the belief in internal resources to maintain sobriety, and coping skills), to relearn the structure of a new setting and cultivate trust and alliance with new support staff and peers. Mechanisms enabling successful SUD treatment outcomes are thought to be related directly to client-provider relationship, linkage services (i.e. transportation, childcare) and matched treatment programs so entering a different program outside of previous treatment may not be encouraging [5,19].
As with inpatient programs, outpatient care is heterogeneous and may differ in duration, intensity and care settings (Figure 2). Outpatient programs are more versatile in that they may be standalone treatment, or can be supplementary aftercare following inpatient treatment. These programs may target individuals with low severity of alcohol use disorder, those with social and environmental stability, or those who prefer (or require) to maintain family and career obligations [14,16,21]. As health care priorities center on increasing accessibility to treatment programs and reducing costs, creating outpatient programs that are similar in outcome to inpatient programs may have the potential to reduce costs without sacrificing efficacy [14,16,19,25]. More traditional outpatient programs can also be made more flexible by being accessible at various times of the day, or at weekends.
Intense outpatient, or day-treatment (also called day hospital) care, is an approach that models long-term inpatient treatment [14/a>-19]. Sessions may occur in a hospital or clinical setting and the structure often involves group psycho education for the greater part of the day, at least five days per week [21]. Psycho education does not differ greatly from sessions offered in inpatient care, and both approaches include therapeutic work through mutual support and relapse prevention. Intense outpatient care can have a similar daily structure as inpatient care, and is usually predetermined for the individual, leaving little room for obligations outside of treatment [14-19]. Additionally, day-treatment, while reducing health care expenditures, is still costly-nearly twice as much compared to traditional outpatient programs [16].
Another difference from an inpatient program can be that outpatient programs do not routinely provide individual therapy, and that 12-step involvement [26,27] may be strongly encouraged but not mandatory [27,28]. Traditional outpatient, also called standard outpatient, is less intense than day hospital and provides ambulatory, or short-term, services [21]. These services can occur in a variety of settings such as community mental health clinics or patient-run support groups where the care needs of the client dictate the intensity of the program [6,16,21]. Other outpatient programs, such as 12-step self-help approaches, are available along with novel formats such as phone-based interventions [24,25].
In conclusion, there are multiple overlapping styles of treatment, and apart from the obvious difference in that individuals in inpatient/residential programs are not living in their own house, there are no other clear consistent differentiating factors.
Significant features of treatment
Significant features of inpatient and outpatient care, such as duration of treatment, goal intensity, and structure of care setting, psycho education, therapeutic alliance, and human capital may all contribute to increased probability of positive post-treatment outcomes. The potential influence of each of these is examined.
Duration of care: The duration of engagement in substance use treatment programs greatly influences post-treatment outcomes with some studies finding length of stay (LOS) to be the most significant predictor of successful recovery [5,17,29,30]. Other studies find LOS to affect sobriety indirectly through encouraging entrance into supplementary aftercare programs [31]. The precise LOS that produces the best outcome is relatively unclear; however, it appears a minimum of 30 days of hospital-based inpatient care, and 3 months of non-hospital inpatient care (i.e. residential) significantly improves success rates 12 months post-treatment [8,20,29,30,32]. A study of 367 adults in abstinence-based inpatient “caring community” for substance use disorders (SUDs) found the duration of inpatient treatment to substantially impact commitment and participation in aftercare programs [17]. Over 70% of individuals who successfully completed more than 80 days of inpatient treatment had better posttreatment outcomes at 6 months than others who completed 25 days or less.
Day-hospital and traditional outpatient programs are variable in duration with some lasting a few months, while more intense programs are usually of shorter duration [6,18,33,34]. In a study of 668 randomized and 405 self-selected participants treatment outcomes of day-hospital were compared to traditional outpatient care at 6 months post-treatment [16]. Day-hospital and traditional outpatient groups involved mandatory attendance and bioverified abstinence (i.e. urine, blood, breath tests) during the course of the 8-week rehabilitation study. Both groups were involved in the same therapeutic structure including supportive group therapy, relapse prevention and off-site 12-step attendance, but day-hospital consisted of many more sessions (104 vs. 24) over 8-weeks of treatment. Participants who were randomized displayed similar improvements in outcome measures after completion of either method; however, those with mid to high psychiatric severity had higher rates of abstinence after day-hospital compared to traditional treatment. In the self-selected group, those completing day-hospital were nearly 3 times more likely to achieve abstinence than those who self-selected traditional outpatient. These findings suggest that a longer-term, and intensive, day-hospital program may be a useful part of any comprehensive treatment program.
Goal intensity: Treatments for SUDs include abstinence-based programs that mandate complete cessation of substance use and harm reduction programs that work toward reduction of substance use to minimize aversive consequences. In one study of 178 substance use treatment programs in Canada, nearly two-thirds of substance abuse treatment programs maintained that moderate alcohol use was unacceptable [35]. Although non-abstinence may be viewed as inappropriate for inpatient programs, the majority of outpatient programs reviewed in the same study applied harm reduction approaches, rather than insisting on complete abstinence. However, goal intensity varies significantly between outpatient treatment programs, and more intense formats, such as day hospital, may require abstinence and incorporate bioverification through blood, breath and urine tests [16,19,35-37]. One study of 1,007 substance users in Scotland found 57% of participants prefer abstinencebased programming while the remaining 43% preferred treatment offering goals other than abstinence, such as stabilization and harm reduction [38]. This is relevant since individuals entering treatment may not yet have the ability to discontinue substance use, and harm reduction approaches may act as a starting point for improvements. Incorporating varying goal opportunities within one treatment program may appeal to diverse needs and encourage a reduction of substance use and eventual cessation. This approach is also known as the gradualism approach through the harm reduction-abstinence continuum [39,40]. Unfortunately, current research evidence is not clear enough to determine if there is a particular level of goal intensity that is most effective in terms of long-term outcomes.
Care structure: As the need to reduce health care costs by limiting inpatient programs increases, the versatility and potential for success through outpatient care is increasingly important. One group compared outpatient with inpatient treatment for up to 18 months [41,42]. Both treatment formats were based on elements of therapeutic community (i.e. group sessions, relapse prevention), with the exception of residing in the care facility while outpatient participants maintained their primary environment. Outcomes were measured using the Addiction Severity Index (ASI) which examines core features of stability such as medical and psychological status, drug and alcohol use, social network and employment. Both outpatient and inpatient conditions demonstrated change in core features over time. Inpatient care only outweighed outpatient programming in aspects of social skills and psychiatric symptoms, which may mean individuals with concomitant psychiatric conditions or those who are socially unstable may benefit from environmental modification. Another study found the effectiveness of treatment delivery to influence outcomes in which retention and completion of either inpatient or outpatient treatment was directly related to client satisfaction [15]. In this study involving 4,165 male and female parolees in California, duration and treatment satisfaction were the strongest predictors of abstinence 12 months post-treatment, and were much more important than the individual care setting. In addition, those with low or high severity of alcohol (and other substance use disorders) benefitted equally from both inpatient and outpatient care.
Increasing accessibility to outpatient programs has encouraged the production of novel programs and delivery methods. An Interactive Voice Response (IVR) intervention was produced to help those with moderate alcohol use in one study in 187 individuals [25]. In this study the IVR program was automated to reduce error in reporting and recall, and was flexible, anonymous, cost-effective and easily accessible [25]. Subjects in this study were given free access to the self-guided change modules for 24 weeks, IVR training, and educational materials. The automated modules were presented to the listener in order of typical recovery and meant to supplement and support new recovery behaviour. Overall, 84% of participants experienced initial alcohol use resolution tracked through telephone interviews. However, these are preliminary results, and the potential utility of IVR, or other novel technological approaches, requires significantly more study. It should also be noted that up to 75% of individuals with alcohol use disorders resolve over time without formal treatment [43,45].
Psychoeducation and treatment approaches: Individuals seeking treatment for alcohol use disorders vary on a number of social and psychological dimensions; however, there is consistent evidence that distress, depression and dysfunctional cognitions accompany alcohol use disorders [8,29,32,46-48]. Behavioural approaches to alcohol abuse disorders incorporate aspects of cognitive behaviour therapy (CBT), motivational enhancement therapy, and Twelve-Step (12-step) Facilitation. CBT allows modification of cognitions related to substance use, such as cravings, peer pressure or emotional states, into adaptive responses to reduce the likelihood of relapse [49]. Motivational enhancement therapy encourages the use of personal resources to make changes related to harmful substance use through therapist motivation. In this model, the therapist broadly guides the client through stages of change; however, not through the recovery process [50-52]. Twelve-Step Facilitation acts as an introduction to other 12-Step programs, such as AA, and is based on self-recovery steps and peer support [26-29].
Psychological distress tolerance, the ability to endure psychological irritants while maintaining goal related behaviour, and inadequate coping skills both increase the probability of premature termination and relapse post-treatment [46,48]. One study examining distress tolerance training randomly placed 76 participants from a inpatient care to one of three conditions: treatment-as-usual; supportive counselling; or Skills for Improving Distress Intolerance [46]. All participants displayed low tolerance to distress in at least one goal directed task. Only individuals in the Skills for Improving Distress Intolerance group showed an increase in distress tolerance, while the supportive counselling group demonstrated increased intolerance, possibly suggesting that sharing events and emotions is not sufficient to aid in coping and may encourage avoidance behaviour.
Psychological distress tolerance, the ability to endure psychological irritants while maintaining goal related behaviour, and inadequate coping skills both increase the probability of premature termination and relapse post-treatment [46,48]. One study examining distress tolerance training randomly placed 76 participants from a inpatient care to one of three conditions: treatment-as-usual; supportive counselling; or Skills for Improving Distress Intolerance [46]. All participants displayed low tolerance to distress in at least one goal directed task. Only individuals in the Skills for Improving Distress Intolerance group showed an increase in distress tolerance, while the supportive counselling group demonstrated increased intolerance, possibly suggesting that sharing events and emotions is not sufficient to aid in coping and may encourage avoidance behaviour.
Over 50% of individuals with substance use disorders have depressive symptoms, with higher rates in inpatient care, contributing to increased likelihood of early withdrawal from treatment [32,34]. The prevalence of depressive symptoms in conjunction with alcohol abuse disorders has been proposed to be, in part, due to deficiencies in positive reinforcement, which is relevant since behavioural activation theory depicts insufficient positive reinforcement as the source of depression [32]. A program for alcohol abuse disorders, known as LETS ACT, was modelled after this theory, and was compared to supportive counselling to examine retention through modifying depressive symptoms in inpatient care. Out of 58 participants from an inpatient care facility only 3% of the LETS ACT group prematurely terminated treatment in comparison to 24% in the supportive counselling group, although individuals in both conditions had similar improvements in depressive symptoms [32].
Maladaptive schemas and cognitions, such as inaccurate assessments of the impacts of alcohol use, may also play a significant role in treatment outcomes such as abstinence after completion of treatment [53]. Many inpatient and outpatient programs provide psycho-education to counter cognitions influencing alcohol use, and one study focused on beliefs about alcohol as a predictor of abstinence post-treatment [47]. Although positive alcohol beliefs are consistently associated with alcohol use, 53 male clients at a 10-day inpatient program who had positive alcohol expectancies did not consume more alcohol at the 1-month follow up. At the 3-month follow up, however, negative alcohol expectancies influenced a reduction in alcohol consumption, possibly indicating the importance of modifying cognitions associated with substance use in treatment programs. This study did not examine longer-term abstinence and so it is uncertain if this theoretical approach is more widely applicable.
In terms of program intensity, the evidence remains mixed. For example, in one study in 102 alcohol-dependent but socially stable patients, a two-phase intensive outpatient program was utilized [18]. The first phase of treatment was 12-weeks of motivational enhancement therapy, followed by up to 9 months of therapy sessions, for a full year of treatment. Group therapy sessions, including behaviour therapy, CBT, problem-oriented and family sessions, were provided 2 to 3 times per week for a total of 80-120 sessions with each session lasting approximately 100 minutes. Abstinence was mandatory during the study period as measured by breathalyser and blood analysis. However, at 12 month follow-up in this intensive outpatient program, 57% of participants had relapsed.
Another approach has been to try and combine CBT with use of the opiate antagonist naltrexone, which reduces cravings to use alcohol [54]. In this study 372 participants were instructed to take 50 mg of naltrexone 30-60 minutes before potential situations involving alcohol, in combination with 8 semi-structured CBT sessions lasting 50-60 minutes over 18-20 weeks. The severity of cravings, consumption of alcohol or adherence to naltrexone during treatment did not predict engagement, and over 50% of participants terminated attendance by the fourth session of basic treatment and before CBT components offered in sessions 5-8. Again, this novel approach does not appear to be one that is likely to be widely generalizable.
Taken together, current research evidence suggests that the components of psycho-education do not differ significantly between inpatient and outpatient programs in terms of content. It remains uncertain if the different components affect outcomes specifically, or if there are key elements to psycho education that are required for good outcomes.
Therapeutic alliance: Collaboration between client and therapist within the scope of treatment decision making and planning is the core element of therapeutic alliance [55]. This alliance may be enhanced through unconditional acceptance, support and congruence on treatment-specific goals [56]. Therapeutic alliance may be an important factor influencing treatment outcomes and encouraging engagement in aftercare programming [19,24,48,57]. The collaboration and social bond that is developed has been linked to early improvements in treatment, increased engagement, retention and abstinence self-efficacy [19,57,58]. One study observed the effects of therapeutic alliance on young adults, aged 18-24 [48]. In the sample of 303 patients, of whom 28% has alcohol as their primary use disorder, they were assessed for therapeutic alliance at baseline, midtreatment (14 days), and at discharge (average of 24 days) regardless of treatment completion. Individuals with strong commitment to Alcoholics Anonymous or Narcotics Anonymous, adaptive coping skills, and abstinence self-efficacy, were more likely to report high levels of alliance. A stronger sense of therapeutic alliance produced a notable decrease in psychological distress at mid-treatment; however, it was not found to influence commitment to 12-step program, coping skills, abstinence self-efficacy or motivation to complete treatment at discharge.
Nonetheless, therapeutic alliance has been proposed to have the potential to be a universal moderator for both inpatient and outpatient programs in diverse populations [19,59]. Data collected by the National Treatment Improvement Evaluation Study from 1992-1995, and an analysis of self-reporting interviews of 6,593 participants from multiple substance use treatment programs in the United States, supported the importance of client-provider relationship in all treatment modalities [19]. Specifically, the strength of the therapeutic alliance was found to have a significant and direct impact on duration of treatment and substance use post-treatment in outpatient programs. Other studies have suggested that the quality of the alliance, as perceived by both client and provider, to be more important than the specific techniques provided by the therapist [19,48,55,58]. However, the characteristics encouraging the formation of an alliance vary greatly and are challenging to pinpoint, so features guiding this process are unclear [48,57]. Thus, currently the potential role of a strong therapeutic alliance on outcomes remains uncertain, as does the best method for achieving this.
Social and human capital: Inpatient care programs may be tailored to individuals with inadequate levels of social and human capital. Human capital is often defined as cumulative skills and competencies that an individual has which may be leveraged in order to achieve abstinence; social capital refers to the ability to form social bonds and affiliate with abstinent peers [17,26,60]. Substance use may begin in young adulthood, which is a vulnerable time during which development of social and human capital often occurs. For this reason, treatments relying on these factors may not be successful if the underlying skills are underdeveloped. A study of 303 inpatients aged 18-24 years found that while individuals may be committed to abstinence upon entering treatment, they may lack the appropriate management tools to attain their goals [8]. Coping skills and the belief in one’s ability to avoid alcohol, or abstinence self-efficacy, were found to be the strongest predictors of treatment success when comparing baseline measures to those at discharge.
Successful outpatient care depends on and appropriate social and environmental situation which will enhance, rather than disrupt, the recovery process. Non-specific support from a social network may mediate a lack of alcohol specific social support in individuals with alcohol use disorders [61]. Environments that are meaningful to the individual can have a positive or negative impact on substance use. A study of 148 outpatients found environmental variables, such as social support, influenced subjective feelings of wellbeing as well as alcohol abuse. Other studies indicate social and environmental stability, as well as abstinence self-efficacy, to be features enabling successful treatment in outpatient settings [26,27,58]. Outpatient programs promoting peer involvement and social support may supplement other forms of treatment allowing the formation ofprosocial networks. Interestingly, perhaps, it is possible to consider a 12-step approach to be one such prosocial network.
12-Step approach: Twelve-step programs are based on self-help and mutual support in which individual motivation and commitment to abstinence are the only membership requirements [62]. In a sample from the National Treatment Outcome Research Study, 142 clients from 8 hospital-based inpatient programs were interviewed at intake and again at 1, 2 and 5 years post-treatment to examine the impact of Alcoholics Anonymous (AA) or Narcotics Anonymous [63]. Frequent Alcoholics Anonymous attendance, at least weekly, predicted consistent abstinence at every follow-up interval in individuals with only alcohol use disorders. Involvement in AA may have long-term benefits for those who are motivated to participate and believe in the tenets of this program. When comparing the effects of non-12-step treatments to AA and no treatment for alcohol use disorders in 466 participants, AA proved to be more effective than on-12-step treatment for problem drinkers at 1-year and 3-year follow up, but outcomes were equivalent at 8-year follow up [45]. Short term studies on formal treatment in combination with AA find this format to be superior to either program alone.
Some inpatient programs are structured around 12-step involvement in which attendance is a mandatory part of the daily program. In a study using 7 inpatient care facilities in 3 metropolitan cities in the U.S. 733 participants were interviewed at 2, 4, and 8 weeks during treatment and again at 6 and 12 months post-treatment to determine the effects of mandatory AA involvement on alcohol use outcomes [31]. Coerced or mandatory involvement in AA did not improve alcohol outcomes in this study. This may be related to personal factors, such as readiness to change, or incongruence between AA principles and personal beliefs.
The impact of programs like AA may be due to the establishment of a supportive social network. In a study with 655 participants from 10 alcohol treatment programs, involvement in AA activities and embracing the social network contributed to abstinence at both 1-year and 3-year follow-up [26]. A significant predictor of relapse includes the number of heavy drinkers in one’s social network, and it is possible that attendance at AA may modify aspects of lifestyle that influence abstinence. Additionally, individuals who seriously engaged in AA activities, such as step-work, finding a sponsor, and studying self-help manuals, doubled their probability of successful long-term recovery from alcohol use. The association between social influences through AA and drinking outcomes was also examined in a study comparing 952 outpatients and 774 patients post-inpatient care [64]. Participants were randomly assigned to one of three conditions: CBT, motivational enhancement therapy or 12-Step treatment. Individuals in the motivational enhancement therapy condition engaged in 4 sessions over 12 weeks while CBT and 12-Step treatment groups experienced 12 sessions over 12 weeks. A significant predictor of treatment outcome, regardless of care modality, was the social network at treatment intake. Further, one pro-drinker in one’s social network is capable of overriding one pro-abstainer even when involved in AA. In a similar study on alcohol use disorder with over 1,700 participants, comparisons were made between the effects of CBT, motivational enhancement therapy and 12-Step Facilitation on outcomes 12-months post-treatment [43]. The findings of this study indicate the relative similarity in outcomes from all 3 forms of intervention, with minimal statistical significance distinguishing superiority. Additionally, over 60% of participants engaged in formal treatment had near equal post-treatment outcomes as those who were untreated, reinforcing the notion of natural recovery. Taken together, the current findings do not support the efficacy of the 12-step program as something that is better than other approaches.
It should be noted that although AA attempts to appeal to all religious and non-religious denominations, the spiritual content, including the Lord’s Prayer at the end of every session at some community settings and submitting to a “Higher Power”, may prevent certain individuals from participating in this program [65,66]. Additionally, there is evidence linking premorbid religiosity and positive connection to God with higher probability of AA membership [67]. This may become a deterrent to treatment for individuals who require the structure and intensity of inpatient care or supplementary support to outpatient programs but are reluctant to attend AA sessions frequently. Additionally, concomitant psychiatric conditions, such as attachment avoidance and anxiety, may make social engagement difficult for certain individuals and create ambivalence toward 12-step approaches to recovery [28].
Overall, the evidence seems to support involvement in an AA program, or something similar, in terms of successful outcomes. However, there appears no consistent evidence to suggest that involvement during an inpatient program is better than during an outpatient program.
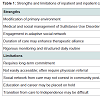
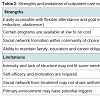
Strengths and Limitations
When considering conclusions from the available data set, a significant limitation is the relatively poor amount of good research in this area. Issues with the research have been recognized for more than 20 years [30], as well as in more recent publications [5,14,16]. Therefore, it is difficult to make definitive conclusions when many factors remain uncertain. Thus, it is not certain of the differences in outcomes for such issues as the severity of alcohol abuse, whether the abuse has gone on for a period of time, if many other treatments have been tried, and the presence of a range of comorbid conditions. These qualifications regarding the overall quality of the data should be recognized when considering the findings that are available.The findings available to date suggest that hospital-based inpatient programs are beneficial for medically assisted detoxification and stabilization of withdrawal symptoms; however, the short duration of care may not effectively support the social needs of individuals with substance use disorders [16,26,60]. Inpatient care may link, in a step-down approach, to residential or outpatient care, both of which may provide a supportive and safe environment enhancing successful long-term recovery. It is conceivable that the goal intensity of inpatient programs may be beneficial for those who are unable to control alcohol consumption, and who therefore require mandatory abstinence-based programming. In addition, the longer duration of treatment might enable in-depth psycho education and skills training in order to develop ample human capital. Despite all of these potential benefits, however, the literature to date does not appear to demonstrate clear differences for most individuals from an inpatient setting. Similarly, although a significant strength of inpatient and inpatient treatment is the removal of the client from their primary environment, this may also be a limitation (Table 1). The transition from a nurturing environment free from potential triggers to the “realworld” is a considerable shift that may tax newly developed coping skills. It is during this transition that potential for relapse is high; nonetheless, it is possible that supplementary outpatient programs may provide additional support to mitigate these environmental triggers.Outpatient programs can be the first line of treatment, or can offer supplementary aftercare as well as offering flexibility in duration, level of commitment, and approach (Table 2). In addition, the ability to maintain family and career obligations may strongly influence commitment to treatment. Engaging in treatment while remaining in the primary environment is both a strength and limitation of this format: individuals with high levels of motivation, abstinence self-efficacy and supportive environment may benefit from using skills acquired immediately within their community, while those without these features may find this format challenging. Traditional outpatient programs have a lax structure and this may not benefit individuals requiring strict daily organization and monitoring in order to recover successfully.
Conclusion and Future Directions
The ability to identify a program that would consistently and effectively treat alcohol use disorders would be of significant benefit both to individuals with this condition as well as to society as a whole. However, the complexity of these disorders and their care makes the development of a single universal treatment unlikely. The findings from the current review also do not suggest that there is a single approach that is consistently effective for all individuals. In terms of the relative benefits of inpatient/residential approaches compared to a purely outpatient approach, again the findings are mixed. This is likely to support a greater move to outpatient programs, ideally of longer duration, as a primary treatment for most jurisdictions for economic reasons.Nonetheless, specific characteristics of the individual seeking treatment may make one treatment approach more effective than another. Furthermore, both inpatient and outpatient programs can have barriers to entry for specific individuals that include limited accessibility and availability of these programs. They can also vary widely depending upon multiple factors (such as geographic location and health care coverage), and as noted in this review, the specific details within each program also varies widely. There is some evidence to suggest that individuals with social and environmental instability and concomitant psychiatric conditions may benefit more from the structure and goal intensity of inpatient programs, and might potentially have a higher likelihood of successful recovery. In contrast, there is some evidence to suggest that individuals with a high degree of motivation and social support may do better in an outpatient setting. Furthermore, a lack of consistency in study populations, experimental methods, and outcome measures limit the ability to effectively compare studies. These aspects are necessary for appropriate decision making regarding the best form of treatment for an individual. Future research must take into account both patient and treatment factors in order to accurately identify which aspects of treatment are necessary and sufficient for a given patient profile. An ideal system would provide access to both types of care, inpatient and outpatient, depending upon needs. However, it is likely that the long-term move to increased outpatient care is likely to continue for economic reasons, and the evidence from the published literature shows, that for most individuals, a long-term outpatient program is likely better than a shorter-term inpatient/residential program. At this point, the inconclusive evidence suggests that the details included in the individual program do not appear as important as the time spent in such a program. The only conclusion that can be made is that the longer an individual is in a program, then the more likely it is that a positive outcome is to occur.
References
- Edwards G (1997) Alcohol policy and the public good. Addiction 92: S73-S79
- Room R, Babor T, Rehm J (2005) Alcohol and public health. Lancet 365: 519-530.
- (2014) National Institute on Alcohol Abuse and Alcoholism. Alcohol Facts and Statistics.
- World Health Organization (2014) Global status report on alcohol and health 2014.
- Stein BD, Kogan JN, Sorbero M (2009) Substance abuse detoxification and inpatient treatment among Medicaid-enrolled adults: rates and duration of subsequent treatment. Drug Alcohol Depend 104: 100-106.
- Kaskutas LA, Witbrodt J, French MT (2004) Outcomes and costs of day hospital treatment and nonmedical day treatment for chemical dependency. J Stud Alcohol 65: 371-382.
- Lievens D, Vander Laenen F, Christiaens J (2014) Public spending for illegal drug and alcohol treatment in hospitals: an EU cross-country comparison. Subst Abuse Treat Prev Policy 9: 26.
- Kelly JF, Urbanoski KA, Hoeppner BB, Slaymaker V (2012) “Ready, willing, and (not) able” to change: Young adults’ response to inpatient treatment. Drug Alcohol Depend 121: 224-230.
- Weisner C, Delucchi K, Matzger H, Schmidt L (2003) The role of community services and informal support on five-year drinking trajectories of alcohol dependent and problem drinkers. J Stud Alcohol 64: 862-873.
- Witbrodt J, Mertens J, Kaskutas LA, Bond J, Chi F, et al. (2012) Do 12-step meeting attendance trajectories over 9 years predict abstinence? J Subst Abuse Treat 43: 30-43.
- Moos RH (2007) Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend 88: 109-121.
- Moos RH (2007) Theory-based processes that promote the remission of substance use disorders. Clin Psychol Rev 27: 537-551.
- McLellan AT, Carise D, Kleber HD (2003) Can the national addiction treatment infrastructure support the public’s demand for quality care? J Subst Abuse Treat 25:117–121.
- Finney JW, Hahn AC, Moos RH (1996) The effectiveness of inpatient and outpatient treatment for alcohol abuse: the need to focus on mediators and moderators of setting effects. Addiction 91: 1773-1796.
- Burdon WM, Dang J, Prendergast ML, Messina NP, Farabee D (2007) Differential effectiveness of inpatient versus outpatient aftercare for parolees from prison-based therapeutic community treatment programs. Subst Abuse Treat Prev Policy 2: 16.
- Weisner C, Mertens J, Parthasarathy S, Moore C, Hunkeler EM, et al. (2000) The outcome and cost of alcohol and drug treatment in an HMO: day hospital versus traditional outpatient regimens. Health Serv Res 35: 791-812.
- Arbour S, Hambley J, Ho V (2011) Predictors and outcome of aftercare participation of alcohol and drug users completing inpatient treatment. Subst Use Misuse 46: 1275-1287.
- Bottlender M, Soyka M (2004) Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol Alcohol 39: 357-361.
- Shin HC, Marsh JC, Cao D, Andrews CM (2011) Client-provider relationship in comprehensive substance abuse treatment: differences in residential and nonresidential settings. J Subst Abuse Treat 41: 335-346.
- Corrigan D, O'Gorman A (2007) Report of the HSE working group on inpatient treatment & rehabilitation (Substance Users). Health Service Executive, Dublin.
- Ilgen MA, Tiet Q, Finney JW, Harris AH (2005) Recent suicide attempt and the effectiveness of inpatient and outpatient substance use disorder treatment. Alcohol Clin Exp Res 29: 1664-1671.
- Haber P, Lintzeris N, Proude E, Lopatko O (2009) Guidelines for the treatment of alcohol problems. Australian government Department of Health and Ageing.
- United Nations (2002) Contemporary drug abuse treatment: A review of the evidence base.
- Carter RE, Haynes LF, Back SE, Herrin AE, Brady KT, et al. (2008) Improving the transition from inpatient to outpatient addiction treatment: gender differences in response to supportive telephone calls. Am J Drug Alcohol Abuse 34: 47-59.
- Schroder KE, Tucker JA, Simpson CA (2013) Telephone-based self-change modules help stabilize early natural recovery in problem drinkers. J Stud Alcohol Drugs 74: 902-908.
- Bond J, Kaskutas LA, Weisner C (2003) The persistent influence of social networks and alcoholics anonymous on abstinence. J Stud Alcohol 64: 579-588.
- Donovan DM, Ingalsbe MH, Benbow J, Daley DC (2013) 12-Step interventions and mutual support programs for substance use disorders: An overview. Soc Work Public Health 28: 313-332.
- Jenkins CO, Tonigan JS (2011) Attachment avoidance and anxiety as predictors of 12-step group engagement. J Stud Alcohol Drugs 72: 854-863.
- Deane FP, Wootton DJ, Hsu CI, Kelly PJ (2012) Predicting dropout in the first 3 months of 12-step inpatient drug and alcohol treatment in an Australian sample. J Stud Alcohol Drugs 73: 216-225.
- Gottheil E, McLellan AT, Druley KA (1992) Length of stay, patient severity and treatment outcome: sample data from the field of alcoholism. J Stud Alcohol 53: 69-75.
- Zemore SE, Kaskutas LA (2008) Services received and treatment outcomes in day hospital and inpatient programs. J Subst Abuse Treat 35: 232-244.
- Magidson JF, Gorka SM, MacPherson L, Hopko DR, Blanco C, et al. (2011) Examining the effect of the Life Enhancement Treatment for Substance Use (LETS ACT) on inpatient substance abuse treatment retention. Addict Behav 36: 615-623.
- Kolodziej ME, Muchowski PM, Hamdi NR, Morrissette P, McGowan AJ, et al. (2012) Adaptation of the patient feedback survey at a community treatment setting. Am J Addict 21: 63-71.
- Brown RA, Ramsey SE, Kahler CW, Palm KM, Monti PM, et al. (2011) A randomized controlled trial of cognitive-behavioral treatment for depression versus relaxation training for alcohol-dependent individuals with elevated depressive symptoms. J Study Alcohol Drugs 72: 286-296.
- Rosenberg H, Devine EG, Rothrock N (1996) Acceptance of moderate drinking by alcoholism treatment services in Canada. J Stud Alcohol 57: 559-562.
- Graff FS, Morgan TJ, Epstein EE, McCrady BS, Cook SM, et al. (2009) Engagement and retention in outpatient alcoholism treatment for women. Am J Addict 18: 277-288.
- NICE (2011) Alcohol-use disorders: diagnosis, assessment and management of harmful drinking and alcohol dependence. NICE clinical guideline 115.
- McKeganey N, Morris Z, Neale J, Robertson M (2004) What are drug users looking for when they contact drug services: abstinence or harm reduction? Drugs: Edu Prev Policy 11: 423-435.
- Futterman R, Lorente M, Silverman S (2004) Integrating harm reduction and abstinence-based substance abuse treatment in the public sector. Subst Abuse 25: 3-7.
- Kellogg SH (2003) On “Gradualism” and the building of the harm reduction-abstinence continuum. J Subst Abuse Treat 25: 241-247.
- Guydish J, Werdegar D, Sorensen JL, Clark W, Acampora A (1998) Drug abuse day treatment: A randomized clinical trial comparing day and inpatient treatment programs. J Consult Clin Psychol 66: 280-289.
- Guydish J, Sorensen JL, Chan M, Werdegar D, Bostrom A, et al. (1999) A randomized trial comparing day and inpatient drug abuse treatment: 18-month outcomes. J Consult Clin Psychol 67: 428-434.
- Cutler RB, Fishbain DA (2005) Are alcoholism treatments effective? The project MATCH data. BMC Public Health 5: 75.
- Sobell LC, Ellingstad TP, Sobell MB (2000) Natural recovery from alcohol and drug problems: Methodological review of the research with suggestions for future directions. Addiction 95: 749-764.
- Timko C, Moos RH, Finney JW, Lesar MD (2000) Long-term outcomes of alcohol use disorders: comparing untreated individuals with those in Alcoholics Anonymous and formal treatment. J Stud Alcohol 61: 529-540.
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, Lejuez CW (2012) Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug Alcohol Depend 122: 70-76.
- Jones BT, McMahon J (1994) Negative and positive alcohol expectancies as predictors of abstinence after discharge from a inpatient treatment program: a one-month and three-month follow-up study in men. J Stud Alcohol 55: 543-548.
- Urbanoski KA, Kelly JF, Hoeppner BB, Slaymaker V (2012) The role of therapeutic alliance in substance use disorder treatment for young adults. J Subst Abuse Treat 43: 344-351.
- Fuller RK, Hiller-Sturmhofel S (1999) Alcoholism treatment in the United States. Alcohol Res Health 23: 69-77.
- Angres DH, Bettinardi–Angres K (2008) The disease of addiction: Origins, treatment, and recovery. Dis Mon 54: 696-721.
- Hettema J, Steele J, Miller WR (2005) Motivational interviewing. Annu Rev Clin Psychol 1: 91-111.
- Miller WR, Rose GS (2009) Toward a theory of motivational interviewing. Am Psychol 64: 527-537.
- Shorey RC, Stuart GL, Anderson S, Strong DR (2013) Changes in Early Maladaptive Schemas After Inpatient Treatment for Substance Use. J Clin Psychol 69: 912-922.
- Vuoristo-Myllys S, Lahti J, Alho H, Julkunen J (2013) Predictors of dropout in an outpatient treatment for problem drinkers including cognitive–behavioral therapy and the opioid antagonist naltrexone. J Stud Alcohol Drugs 74: 894-901.
- Ardito RB, Rabellino D (2011) Therapeutic alliance and outcome of psychotherapy: historical excursus, measurements, and prospects for research. Front Psychol 2: 270.
- Horvath AO, Symonds BD (1991) Relation between working alliance and outcome in psychotherapy: A meta-analysis. J Couns Psychol 38: 139-149.
- Meier PS, Barrowclough C, Donmall MC (2005) The role of the therapeutic alliance in the treatment of substance misuse: a critical review of the literature. Addiction 100: 304-316.
- Ilgen M, Tiet Q, Finney J, Moos RH (2006) Self-efficacy, therapeutic alliance, and alcohol-use disorder treatment outcomes. J Stud Alcohol 67: 465-472.
- Reid SC, Teesson M, Sannibale C, Matsuda M, Haber PS (2005) The efficacy of compliance therapy in pharmacotherapy for alcohol dependence: a randomized controlled trial. J Stud Alcohol 66: 833-841.
- Winstanley EL, Steinwachs DM, Ensminger ME, Latkin CA, Stitzer ML, et al. (2008) The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug Alcohol Depend 92: 173-182.
- Beattie MC, Longabaugh R, Elliott G, Stout RL, Fava J, et al. (1993) Effect of the social environment on alcohol involvement and subjective well-being prior to alcoholism treatment. J Study Alcohol Drugs 54: 283-296.
- (2013) Alcoholics Anonymous World Services.
- Gossop M, Stewart D, Marsden J (2008) Attendance at Narcotics Anonymous and Alcoholics Anonymous meetings, frequency of attendance and substance use outcomes after inpatient treatment for drug dependence: a 5‐year follow‐up study. Addiction 103: 119-125.
- Stout RL, Kelly JF, Magill M, Pagano ME (2012) Association between social influences and drinking outcomes across three years. J Stud Alcohol Drugs 73: 489-497.
- Dossett W (2013) Addiction, spirituality and 12-step programmes. Int Soc Work 56: 369-383.
- Karoll BR (2010) Applying social work approaches, harm reduction, and practice wisdom to better serve those with alcohol and drug use disorders. J Social Work 10: 263-281.
- Krentzman, AR, Robinson EA, Perron, BE, Cranford, JA (2011) Predictors of Membership in Alcoholics Anonymous in a Sample of Successfully Remitted Alcoholics. J Psychoactive Drugs 43: 20-26.
Maladaptive schemas and cognitions, such as inaccurate assessments of the impacts of alcohol use, may also play a significant role in treatment outcomes such as abstinence after completion of treatment [53]. Many inpatient and outpatient programs provide psycho-education to counter cognitions influencing alcohol use, and one study focused on beliefs about alcohol as a predictor of abstinence post-treatment [47]. Although positive alcohol beliefs are consistently associated with alcohol use, 53 male clients at a 10-day inpatient program who had positive alcohol expectancies did not consume more alcohol at the 1-month follow up. At the 3-month follow up, however, negative alcohol expectancies influenced a reduction in alcohol consumption, possibly indicating the importance of modifying cognitions associated with substance use in treatment programs. This study did not examine longer-term abstinence and so it is uncertain if this theoretical approach is more widely applicable.