Journal of Orthopedics & Rheumatology
Download PDF
<
Case Report
*Address for Correspondence: Mirco Lo Presti, 2nd Orthopaedic and Traumatology Clinic and Biomechanics Laboratory, Codivilla-Putti Research Center Istituto Ortopedico Rizzoli, University of Bologna, 1/10 – 40100 – Bologna, Italy, Tel: +051 6366507; E-mail: m.lopresti@biomec.ior.it
Citation: Presti ML, Francesco I, Sharma B, Raspugli GF, Bignozzi S, et al. Reasons for Early Failure in Medial Unicondylar Arthroplasty. Radiographic Analysis on the Importance of Joint Line Restoration. J Orthopedics Rheumatol. 2014;2(1): 5.
Copyright © 2015 Presti ML, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 2, Issue: 1
Submission: 10 July 2014 | Accepted: 06 January 2015 | Published: 12 January 2015
Reviewed & Approved by: Dr. Elliott H. Leitman, Director of Orthopaedic Education, Christiana Care Health System, USA.
Keywords: UKA; Knee; Joint line; Alignment; Failure mechanism
An independent observer (GR), expert in this field, blindly evaluated pre- and post-operative radiographs, measuring the femoro-tibial angle (FTA), tibial plateau angle (TPA) and posterior tibial slope (PTS): measurements were performed on digital A-P and lateral radiographs three times, on three different days, usingpreviously reported techniques [38]. (Intra-observer variability, FTA = 0.87, TPA = 0.83, PTS = 0.80). Moreover, since limb alignment and survivorship in a UKA are very sensitive to change in JL [39-41]; a previously validated method, based on the correlation between femoral width and the distance from the femoral adductor tubercle to JL, was used for radiographic JL measurement [42]. Briefly, the JL was assessed by calculating the distance from the adductor tubercle according to the femoral width multiplied by a validated ratio [43].The magnification of the digital radiograph was set to 40% pixels and the image was changed from black to white, without changing the contrast settings in the proprietary software, to provide the best image quality. Failures and matched control group were compared in terms of pre- post-operative changes in alignment (FTA, TPA, PTS) and JL line position (Figure 2).
Reasons for Early Failure in Medial Unicondylar Arthroplasty. Radiographic Analysis on the Importance of Joint Line Restoration
Mirco Lo Presti*, Iacono Francesco , Bharat Sharma, Giovanni Francesco Raspugli, Simone Bignozzi, Bruni Danilo, Stefano Zaffagnini, Maria Pia Neri and Maurilio Marcacci
- 2Orthopaedic and Traumatology Clinic and Biomechanics Laboratory, Codivilla-Putti Research Center Istituto Ortopedico Rizzoli, University of Bologna, Italy
*Address for Correspondence: Mirco Lo Presti, 2nd Orthopaedic and Traumatology Clinic and Biomechanics Laboratory, Codivilla-Putti Research Center Istituto Ortopedico Rizzoli, University of Bologna, 1/10 – 40100 – Bologna, Italy, Tel: +051 6366507; E-mail: m.lopresti@biomec.ior.it
Citation: Presti ML, Francesco I, Sharma B, Raspugli GF, Bignozzi S, et al. Reasons for Early Failure in Medial Unicondylar Arthroplasty. Radiographic Analysis on the Importance of Joint Line Restoration. J Orthopedics Rheumatol. 2014;2(1): 5.
Copyright © 2015 Presti ML, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 2, Issue: 1
Submission: 10 July 2014 | Accepted: 06 January 2015 | Published: 12 January 2015
Reviewed & Approved by: Dr. Elliott H. Leitman, Director of Orthopaedic Education, Christiana Care Health System, USA.
Abstract
Background: Survivorship of Unicompartimental Knee Arthroplasty (UKA) remains a drawback, especially compared to the outcome of Total knee Arthroplasty (TKA). However, this could be improved by identifying and correcting failure mechanisms. To this purpose, this study aims at exploring failure modalities of UKA, with particular focus on the role of Joint Line (JL) position and alignment as variable to be optimized for a successful outcomeMaterial & methods: This study explores modes of failure in 266 medial UKAs, by analyzing the correlation between changes in the obtained alignment and the ideal JL position. In detail, a radiological comparison was performed between 24 failures and 24 matched controls, to determine the importance of UKA positioning in terms of femoro-tibial angle (FTA), tibial plateau angle (TPA), and posterior tibial slope (PTS).
Results: Failure occurred for subsidence of the tibial component in two knees, unexplained pain in seven patients, aseptic loosening of the tibial component in eight, aseptic loosening of the femoral component in three, medial tibial fracture in one, and overall osteoarthritis progression in three. The radiographic analysis showed that statistically significant differences could be found in the failure group in terms of higher variation of FTA, PTS, and JL height with respect to the control group.
Conclusions: A successful outcome after UKA is determined by a correct alignment in all planes, as demonstrated by the failures analyzed in our series: not appropriate coronal alignment, distal JL line positioning, and abnormal PTS were observed and correlated with the failed cases. Thus, based on the results of this study, it could be recommended that the JL position should be carefully controlled while implanting a UKA not only with regard to the coronal plane: in fact, attention should be paid on the implant component positioning in all planes.
Keywords: UKA; Knee; Joint line; Alignment; Failure mechanism
Introduction
In recent years unicondylar knee replacement (UKA) has come forth as a plausible alternative to total knee Arthroplasty (TKA) for specific patient categories [1-5]. This success of surgical option has been favoured by increasing awareness on the importance of proper selection criteria, as well as by advances in prosthesis design and surgical technique. Compared to TKA, UKA is less traumatic, conserves more bone stock and preserves native knee kinematics; resulting in earlier convalescence and better subjective outcome [6-8]. These advantages have expanded its indications to include primary osteonecrosis, younger and more active populations [9-11]. And have also inspired research in bicondylar UKA replacement.However, unexplained UKA failures [12-24], presenting as aseptic component loosening, polyethylene wear, and antero-medial pain, suggest the existence of not yet well identified parameters that, once addressed, could help to further improve the results, which currently present a slightly poorer long-term survivorship in comparison to TKA [25,26]. This represents a sizable population of patients, whose failure cannot be attributed to infection, progression of osteoarthritis, tibial plateau fracture, instability, and metabolic diseases [12-24]. A variety of factors may play a role in these failures. Patient selection, [18,27] implant design, [22,28] and surgical technique [18,21,22,27,29] have been considered among the factors playing a major role in earlier publications [21,28,29]. However, failures have been reported also in cases presenting optimal characteristics in terms of demographic parameter and postoperative alignment [12,13,15,17]. Earlier failure rate unrelated to change in coronal alignment was reported to range from 3.6% to 28.6%: with either unexplained femoral [12,15,17] or tibial loosening [13].
Among the failure mechanisms that should be explored to understand the high failure rate still attributed to unknown factors, prosthetic component positioning deserves further attention. In fact, success may be not only related to the coronal alignment, but could also depend on the appropriateness of JL restoration in terms of UKA positioning in different planes.
Thus, the aim of this study was to evaluate, in a large cohort of patients, how changes in terms of JL level restoration in the different planes may determine failures in UKA.
Materials and Methods
The study cohort consisted of 246 patients (men/women: 87/159),who underwent 266 medial UKAs. UKAs were implanted in 187 patients (70.3 %) for osteoarthritis isolated to medial compartment and in 79 (29.7 %) for primary osteonecrosis of medial femoral condyle. Selection criteria were: patients more than 50 years old, involved in low-demand activity, with a BMI less than 35 kg/m2, a knee ROM of at least 90 degrees, less than 10 degrees of fixed flexion deformity, without clinical cruciate ligament instability and major angular deformities [30]. If the patient was involved in a high-demand activity, UKA was offered only if such activity could be curtailed after surgery. Inflammatory arthritis, secondary spontaneous osteonecrosis of the knee (SPONK) or involvement of other compartments were considered as contraindication for the procedure [9,30-32].Preoperatively, all patients had weight bearing anteroposterior and lateral radiographs of the knee [33]. The UKA’s were all performed by three senior surgeons (MM, SZ, FI) through a minimally invasive, quadriceps-sparing surgical exposure [34-36], using a surgical technique recommended by the manufacturer, to implant the cemented femoral and all-polyethylene tibial components (Preservation® Uni-Compartmental Knee; DePuy Orthopaedics Inc, Warsaw, IN, USA) (Figure 1). The size of the all-poly tibia component used was selected and applied in order to restore the presumed prepathological varus deformity [37]. As estimated from the contra lateral limb.
Rehabilitation was started on first postoperative day afterdrain removal and dressing, with static quadriceps exercises andcontinuous passive motion: 90° of knee flexion achieved over 2 to 3days, while partial weight-bearing with two crutches was advised for 30 days. After gradual progression as tolerated, full weight-bearing was generally started in 45 days. Quadriceps strengthening by electrostimulation was done for 2 weeks after suture removal. Thereafter, patients continued unsupervised physiotherapy at home.
Revision was considered as a failure for this study. In this population, UKA failed in 30 patients who complained of unresolved clinical condition within 2 years and underwent a revision at a mean 24.8 months (range 1 – 58 months) after primary surgery. The UKA was revised with primary TKA (PFC® Sigma® RP; DePuy Orthopaedics Inc) in 24 knees and with a constrained modular design (PFC® Sigma® TC3; DePuy Orthopaedics Inc) in 6 knees. The constrained modular design was used if the patient had poor underlying bone, bone defects requiring augmentation, joint instability, septic loosening of the prosthesis and medial tibial fracture. Augments were used in all six patients who underwent revision with constrained modular design. While prosthetic infection was revised in two stages, all other failures were revised in one stage. Among these revised UKA, 24 failures, not related to infection and with both pre-operative and post-operativeradiographs, were included in the analysis (among the 6 cases not included in the study, 3 were drop outs lost at follow-up, and 3 were septic failures).
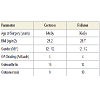
The demographic profile of the failured patients was classified by age (< 60 years, >60 years), gender (men, women), BMI (< 30 kg/m2, ≥ 30 kg/m2) and pre-operative activity (sedentary, active). According to these criteria, a case control group was selected from the overall population of not failed patients, identifying 24 survivors, at at least 2 year follow-up, matching the demographic profile, as well as the etiology of the failure group (Table 1). Since the study did not involve any additional radiographs, interventions, or followup, an institutional review board approval or informed consent was not obtained from each patient whose data was acquired and used ensuring anonymity.
An independent observer (GR), expert in this field, blindly evaluated pre- and post-operative radiographs, measuring the femoro-tibial angle (FTA), tibial plateau angle (TPA) and posterior tibial slope (PTS): measurements were performed on digital A-P and lateral radiographs three times, on three different days, usingpreviously reported techniques [38]. (Intra-observer variability, FTA = 0.87, TPA = 0.83, PTS = 0.80). Moreover, since limb alignment and survivorship in a UKA are very sensitive to change in JL [39-41]; a previously validated method, based on the correlation between femoral width and the distance from the femoral adductor tubercle to JL, was used for radiographic JL measurement [42]. Briefly, the JL was assessed by calculating the distance from the adductor tubercle according to the femoral width multiplied by a validated ratio [43].The magnification of the digital radiograph was set to 40% pixels and the image was changed from black to white, without changing the contrast settings in the proprietary software, to provide the best image quality. Failures and matched control group were compared in terms of pre- post-operative changes in alignment (FTA, TPA, PTS) and JL line position (Figure 2).
Figure 2: Graphic representation of femorotibial angle (FTA), tibial plateau angle (TPA), posterior tibial slope (PTS), and joint line (JL) height measurements. Radiograph of a failed Unicondylar Arthroplasty (A) UKA prior to revision; Revision with Primary Total Knee Arthroplasty (B) Short film (C) Panoramic View.
Statistical Analysis
For each group, differences between pre-operative and postoperative data were compared with paired Student t-test, after verification of normal distribution, with Sahpiro Wilk W test, of all data for each cohort. Comparison of continuous parameters between cohorts was analyzed with unpaired Student t-test. Comparison of categorical variables, such as sex or etiology, between the two cohorts was done with Chi-square test.Significance was set at p=0.05.
Results
Failure occurred for subsidence of the tibial component in two knees, unexplained pain in seven patients, aseptic loosening of the tibial component in eight, aseptic loosening of the femoral component in three, medial tibial fracture in one, and overall osteoarthritis progression in three.No difference between the two cohorts in terms of BMI (29.2±3.7 Control; 28.7±2.7 Fail)
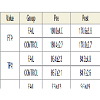
Average variation of FTA after surgery was 2.3±1.7° (95% CI 1.5 to 3.0) in the control group and 4.0±3.2° (95% CI 2.6 to 5.4) in the failure group. The difference between groups was statistically significant (p=0.0222).
Average variation of TPA after surgery was 2.7±2.4° (95% CI 1.7 to 3.7) in the control group and 3.5±2.2° (95% CI 2.5 to 4.4) in the failure group. The difference between groups was non-significant (p=n.s.).
Average variation of PTS after surgery was 1.9±1.4° (95% CI 1.3 to 2.5) in the control group and 4.8±4.1° (95% CI 2.9 to 6.8) in the failure group. The difference between groups was statistically significant (p=0.0025).
Average variation of JL height was 1.2±2.7 mm (95% CI 0.1 to 2.4) in the control group and 4.3±3.8 mm (95% CI 2.7 to 6.0) in the failure group. The difference between groups was statistically significant (p=0.0022) (Table 2).
Discussion
The results of this study underline the importance of the correct prosthetic components positioning for the success of the implant. JL restoration is a key factor in the explanation of aseptic failures. In particular, success may be not only related to the appropriate coronal alignment, and failures otherwise attributed to unknown factors may be actually due to a failure mechanism based on an incorrect UKA positioning in different planes, as shown by this study.The current report is a case-control study: 24 aseptic failures were evaluated radiographic to compare the limb alignment and JL position in the different planes with a series of demographically matched UKA controls from the same cohort of patients treated in our Institute by the surgical equip and evaluated at the same followup time. Radiographs retrieved in these 48 patients were evaluated for FTA, TPA, PTS, and JL position, and data were analyzed to correlate the prosthetic components positioning with otherwise unexplained UKA failures.
While many parameters have been associated with early failure of UKA, some of these associations are still controversial leaving lot of unexplained failures. Contradictory reports exist on the association between early outcome of UKA and younger age [21], obesity [17,44], polyethylene thickness [28], gender or patellofemoral arthritis [44]. There are suggestions that errors in patient selection and surgical technique lead to early failure and revision in the post-operative period [24]. Existing literature helped identify the ideal indications, contraindications, sterilization protocols, surgical technique, polyethylene thickness, implant design, bearing surface and cementing techniques for a successful UKA. This led to the current minimally invasive UKA surgery that aims to restore the JL by realigning the limb to a presumed pre-operative alignment. However, there is a significant unexplained early failure after UKA within the first two years after surgery.
In fact, unexplained failures have been already reported also in other studies applying similar patient selection criteria, surgical technique, and implant design. Hamilton et al. identified eight unexplained femoral component loosening in a series of 221 medial UKA’s with a 4.1% failure rate at 13.3 month follow-up [15]. Mariani et al. reported a 28.6% failure rate in 39 medial UKA’s AT 9-12 month follow-up, all of which were due to femoral loosening [16]. Naal et al. reported a single case of femoral and tibial loosening each in a series of 88 UKA, with a 3.1% failure rate at 2 years [17]. In a metal backed, mobile bearing tibial component variant of the current design, Arastu et al. reported a 21% failure rate due to pain (44%) and tibial loosening(33%), at 22 months follow-up of 43 UKA’s [13].
Among the factors involved in the failure mechanism, the coronal alignment has been accounted as key factor with controversial evidence. Some studies reported no difference in post-operative coronal plane between survivors and failures, although it had been overcorrected in both groups [21,23,28], especially at least in the early follow-up [15]. In a previous report evaluating a similar population, coronal plane alignment was correlated to excellent and good outcome on HSS score, but not with failures [36]. On the other hand, in another study an increased PTS was associated with failure of UKA in primary SPONK, [38]. Thus, JL line position should be considered in all planes to properly address its influence on the failure rate. However, up to now, JL has not been extensively explored in the literature to address the importance of its position on different planes, independently from the coronal plane alignment, for the associationwith early failures in UKA.
The results of our study suggest that change in JL position can affect the outcome of UKA, independently from the change in coronal plane angle. The ideal JL position was derived from a ratio between femoral width and distance from the adductor tubercle. Unlike in the control group (of survivors), the post-operative JL line was 3 mm distal compared to the ideal position in the failure group. Moreover, also the variation of PTS was significantly correlated with the failure group, thus confirming the importance of the appropriate JL restoration in all planes. The JL position of the treated compartment should be controlled intra-operatively with validated methods that to reduce the incidence of failures [45-47].
Beside the significant findings in terms of UKA failure mechanism explanation, this study also presents some limitations. The main limitation is the retrospective design, which also caused the evaluation of some demographic characteristics only as dichotomic variables, and the presence of drop outs. However, this study considers a large survey and the failure group was matched with survivors with similar demographics, surgical procedure and implant, thus allowing to explore differences in the study populations that could be related to otherwise unexplained failures. Other limitations are also related to the methodology to document prosthetic components positioning. While the visualization of the radiograph was standardized, it is possible that the exposure, hip rotation, position of the x-ray tube and knee flexion could have been variable. Moreover, the rotation of the tibial component has been suggested to influence the final outcome [48,49]. And how this could have contributes to the failure mechanism also in our series has not been evaluated. However, while further studies with a prospective study design and a stronger methodology will better assess how the variation of implant positioning in different planes may determine the final outcome, this study shows that surgeons shouldn’t just focus on the coronal alignment.
Alignment has to be considered in all planes, since JL and PTS are also key aspects to determine a successful outcome after UKA.
Conclusions
Variations of FTA but also PTS and JL height have been correlated with the failures observed in our series. Thus, based on the results of this study, it could be recommended that the JL position should be carefully controlled while implanting a UKA not only with regard to the coronal plane: in fact, attention should be paid on the implant component positioning in all planes.References
- Dettoni F, Bonasia DE, Castoldi F, Bruzzone M, Blonna D, et al. (2010) High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J 30: 131-140.
- Griffin T, Rowden N, Morgan D, Atkinson R, Woodruff P, et al. (2007) Unicompartmental knee arthroplasty for the treatment of unicompartmental osteoarthritis: a systematic study. ANZ J Surg 77: 214-221.
- Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V, et al. (2008) Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop Ago 79: 499-507.<
- Laurencin CT, Zelicof SB, Scott RD, Ewald FC (1991) Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res 273: 151-156.
- Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW, et al. (2012) Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res 470: 84-90.
- Dalury DF, Fisher DA, Adams MJ, Gonzales RA (2009) Unicompartmental knee arthroplasty compares favorably to total knee arthroplasty in the same patient. Orthopedics 32.
- Robertsson O, Borgquist L, Knutson K, Lewold S, Lidgren L (1999) Use of unicompartmental instead of tricompartmental prostheses for unicompartmental arthrosis in the knee is a cost-effective alternative. 15,437 primary tricompartmental prostheses were compared with 10,624 primary medial or lateral unicompartmental prostheses. Acta Orthop Scand 70: 170-175.
- Heyse TJ, El-Zayat BF, De Corte R, Chevalier Y, Scheys L, et al. (2014) UKA closely preserves natural knee kinematics in vitro. KSSTA 22: 1902-1910.
- Myers TG, Cui Q, Kuskowski M, Mihalko WM, Saleh KJ (2006) Outcomes of total and unicompartmental knee arthroplasty for secondary and spontaneous osteonecrosis of the knee. J Bone Joint Surg Am 88: 76-82.
- Parratte S, Argenson JN, Pearce O, Pauly V, Auquier P, et al. (2009) Medial unicompartmental knee replacement in the under-50s. J Bone Joint Surg Br 91: 351-356.
- Price AJ, Dodd CA, Svard UG, Murray DW (2005) Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br 87: 1488-1492.
- Aleto TJ, Berend ME, Ritter MA, Faris PM, Meneghini RM (2008) Early failure of unicompartmental. knee arthroplasty leading to revision. J Arthroplasty 23: 159-163.
- Arastu MH, Vijayaraghavan J, Chissell H, Hull JB, Newman JH, et al. (2009) Early failure of a mobile-bearing unicompartmental knee replacement. Knee Surg Sports Traumatol Arthrosc 17: 1178-1183.
- Furnes O, Espehaug B, Lie SA, Vollset SE, Engesaeter LB, et al. (2007) Failure mechanisms after unicompartmental and tricompartmental primary knee replacement with cement. J Bone Joint Surg Am 89: 519-525.
- Hamilton WG, Collier MB, Tarabee E, McAuley JP, Engh CA Jr, et al. (2006) Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty 21: 98-107.
- Mariani EM, Bourne MH, Jackson RT, Jackson ST, Jones P (2007) Early failure of unicompartmental knee arthroplasty. J Arthroplasty 22: 81-84.
- Naal FD, Neuerburg C, Salzmann GM, Kriner M, von Knoch F, et al. (2009) Association of body mass index and clinical outcome 2 years after unicompartmental knee arthroplasty. Arch Orthop Trauma Surg 129: 463-468.
- Riebel GD, Werner FW, Ayers DC, Bromka J, Murray DG (1995) Early failure of the femoral component in unicompartmental knee arthroplasty. J Arthroplasty 10: 615-621.
- Rothwell AG, Hooper GJ, Hobbs A, Frampton CM (2010) An analysis of the Oxford hip and knee scores and their relationship to early joint revision in the New Zealand Joint Registry. J Bone Joint Surg Br 92: 413-418.
- Saenz CL, McGrath MS, Marker DR, Seyler TM, Mont MA, et al. (2010) Early failure of a unicompartmental knee arthroplasty design with an all-polyethylene tibial component. Knee 17: 53-56.
- Schai PA, Suh JT, Thornhill TS, Scott RD (1998) Unicompartmental knee arthroplasty in middle-aged patients: a 2- to 6-year follow-up evaluation. J Arthroplasty 13: 365-372.
- Skyrme AD, Mencia MM, Skinner PW (2002) Early failure of the porous-coated anatomic cemented unicompartmental knee arthroplasty: A 5- to 9-year follow-up study. J Arthroplasty17: 201-205.
- Song MH, Kim BH, Ahn SJ, Yoo SH, Lee MS (2009) Early complications after minimally invasive mobile-bearing medial unicompartmental knee arthroplasty. J Arthroplasty 24: 1281-1284.
- Vardi G, Strover AE (2004) Early complications of unicompartmental knee replacement: the Droitwich experience. Knee 11: 389-394.
- (2011) Australian Orthopaedic Association National Joint Replacement Registry. Annual Report.
- Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, et al. (2000) The Norvegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand 71: 337-353.
- Skolnick MD, Bryan RS, Peterson LF (1975) Unicompartmental polycentric knee arthroplasty: description and preliminary results. Clin Orthop Relat Res 112: 208-214.
- Knight JL, Atwater RD, Guo J (1997) Early failure of the porous coated anatomic cemented unicompartmental knee arthroplasty. Aids to diagnosis and revision. J Arthroplasty 12: 11-20.
- Palmer SH, Morrison PJ, Ross AC (1998) Early catastrophic tibial component wear after unicompartmental knee arthroplasty. Clin Orthop Relat Res 350: 143-148.
- Borus T, Thornhill T (2008) Unicompartmental knee arthroplasty. J Am Acad Orthop Surg 16: 9-18.
- Mont MA, Baumgarten KM, Rifai A, Bluemke DA, Jones LC, et al. (2000) Atraumatic osteonecrosis of the knee. J Bone Joint Surg Am 82: 1279-1290.
- Patel DV, Breazeale NM, Behr CT, Warren RF, Wickiewicz TL, et al. (1998) Osteonecrosis of the knee: current clinical concepts. Knee Surg Sports Traumatol Arthrosc 6: 2-11.
- LaValley MP, McLaughlin S, Goggins J, Gale D, Nevitt MC, et al. (2005) The lateral view radiograph for assessment of the tibiofemoral joint space in knee osteoarthritis: its reliability, sensitivity to change, and longitudinal validity. Arthritis Rheum 52: 3542-3547.
- Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM (2002) Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am 84-A: 2235-2239.
- Argenson JN, Parratte S, Flecher X, Aubaniac JM (2007) Unicompartmental knee arthroplasty: technique through a mini-incision. Clin Orthop Relat Res 464: 32-36.
- Bruni D, Iacono F, Russo A, Zaffagnini S, Marcheggiani Muccioli GM, et al. (2010) Minimally invasive unicompartmental knee replacement: retrospective clinical and radiographic evaluation of 83 patients. Knee Surg Sports Traumatol Arthrosc 18: 710-717.
- Whiteside LA (2005) Making your next unicompartmental knee arthroplasty last: three keys to success. J Arthroplasty 20: 2-3.
- Bruni D, Iacono F, Raspugli G, Zaffagnini S, Marcacci M (2012) Is unicompartmental arthroplasty an acceptable option for spontaneous osteonecrosis of the knee? Clin Orthop Relat Res 470: 1442-1451.
- Campbell D, Schuster AJ, Pfluger D, Hoffmann F (2010) Unicondylar knee replacement with a new tensioner device: clinical results of a multicentre study on 168 cases. Arch Orthop Trauma Surg 130: 727-732.
- Kasis AG, Pacheco RJ, Hekal W, Farhan MJ, Smith DM, et al. (2004) The precision and accuracy of templating the size of unicondylar knee arthroplasty. Knee 11: 395-398.
- O’Donnell T, Neil MJ (2010) The Repicci II® unicondylar knee arthroplasty: 9-year survivorship and function. Clin Orthop Relat Res 468: 3094-3102.
- Iacono F, Lo Presti M, Bruni D, Raspugli GF, Bignozzi S, et al. (2012) The adductor tubercle: a reliable landmark for analysing the level of the femorotibial joint line. Knee surgery sports traumatolo arthrosc 21: 2725-2729.
- Iacono F, Raspugli GF, Bruni D, Filardo G, Zaffagnini S, et al. (2014) The adductor tubercle as an important Landmark to determine the joint line level in total knee arthroplasty: from radiographs to surgical theatre. KSSTA 22: 3034-3038.
- Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, et al. (2010) Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee 17: 48-52.
- Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL (2000) Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arthroplasty 15: 354-359.
- Romero J, Seifert B, Reinhardt O, Ziegler O, Kessler O (2010) A useful radiologic method for preoperative joint-line determination in revision total knee arthroplasty. Clin Orthop Relat Res Mag 468: 1279-1283.
- Servien E, Viskontas D, Giuffrè BM, Coolican MR, Parker DA (2008) Reliability of bony landmarks for restoration of the joint line in revision knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 16: 263-269.
- Citak M, Suero EM, Citak M, Dunbar NJ, Branch SH, et al. (2013) Unicompartmental knee arthroplasty: is robotic technology more accurate than conventional technique? Knee 20: 268-271.
- Nicoll D, Rowley DI (2010) Internal rotational error of the tibial components is a major cause of pain after total knee replacement. JBJS Br 92: 1238-1244 .