Journal of Surgery
Download PDF
Editorial
Stump Appendicitis and the Critical View of Safety
Eoghan P. Burke*, Salama M, Saeed M, Ahmed I
Department of Surgery, Ireland
*Address for Correspondence:
Eoghan P. Burke, Department of Surgery, Our Lady of Lourdes Hospital,
Drogheda, Ireland, E-ma.il: eoghanburke@rcsi.ie
Submission: 26 June, 2019;
Accepted: 03 July, 2019;
Published: 05 July, 2019
Copyright: © 2019 Burke EP. This is an open access article distributed
under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided
the original work is properly cited.
Editorial
We present a case of a 27-year-old gentleman who presented to
our hospital. He underwent a laparoscopic appendectomy six months
previously. His surgery was complicated by a post-operative collection
which was drained under CT guidance. He had no past medical
history and was on no regular medication. He presented with a one
day history of Right Iliac Fossa (RIF) pain. The pain was constant, dull
in nature and was progressively getting worse. It was associated with
anorexia, nausea and two episodes of vomiting. He denied rigors,
diarrhoea, constipation or urinary tract symptoms. On examination,
he was febrile (39 o
C), his abdomen was soft but tender in the RIF
with guarding. His laboratory investigations were significant for a
C-reactive protein level of 32 mg/L and a white cell count of 14x109/L.
The differential included a post-operative collection. He underwent a
CT scan of his abdomen and pelvis.
The CT scan showed a thickened oedematous wall of the inferior
pole of the cecum along with an appendicular stump which was
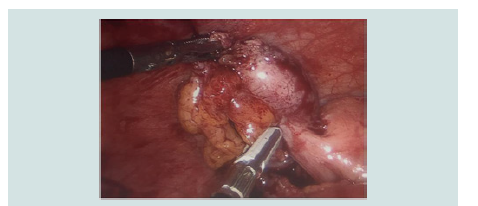
acutely inflamed (Figure 1). The patient underwent laparoscopy in
which an acutely inflamed appendicular stump was seen (Figure 2). It was successfully resected. The patient recovered well and was
discharged home on post-operative day 2. He has reported no further
complications at his 3-month review clinic.
Acute appendicitis is one of the most common indications for
emergency abdominal surgery accounting for approximately 1% of all
surgical operations. Common post-operative complications include
wound infections, intra-abdominal infections and adhesions. The first
two cases of stump appendicitis were reported by Rose et al in 1945
[1]. The precise pathogenesis remains poorly understood, however
it is postulated that obstruction of the remaining stump lumen by
a fecolith may be the causative factor. This increases intraluminal
pressure, impairs venous drainage and allows subsequent bacterial
infection. There are approximately 62 cases reported in the literature
although most authors would suggest that it is underreported. Most
reported cases do not have radiographic or photo-documentation of the appendicular stump being acutely inflamed.
Figure 2: Intraoperative image from completion appendectomy. Identifies
appendicular stump measuring greater than the recommended 5 mm.
Stump appendicitis was traditionally felt to be more common
following a laparoscopic appendectomy secondary to the absence of
tactile feedback and a 3-dimensional perspective. However, the most
extensive review to date on the topic conducted by Subramanian et
al disproved this theory and found it to be more common in open
appendectomies [2].
Multiple factors are thought to contribute to incomplete
appendectomy, the most important being incorrect identification of
the surgical anatomy. This led Subramanian et al to propose A Critical
View of Safety (CVS) for appendectomy similar to that famously
developed by Strasberg et al in 1995 for laparoscopic cholecystectomy
[2]. This CVS for appendectomy centres on correctly identifying the
appendicular-cecal junction and thus the appendicular base. The CVS
is achieved when the taenia libera is seen clearly on the surface of
the cecum running into the base of the appendix with the appendix
elevated and displaced inferiorly and the terminal ileum in the
foreground at laparoscopy. In this position, the mesoappendix can
then be divided appropriately and the base clearly identified.
The length of the appendicular stump left behind is crucial. Most
authors recommend leaving less than 5mm behind. A stump of
greater than 5mm is thought to be large enough to act as a reservoir
for a fecolith [3]. In Figure 3 we depict an intraoperative image from
our patient’s initial laparoscopic appendectomy (Figure 3). We can
see that the CVS has not been identified. This led the surgeon to
incorrectly assume he had identified the appendicular base leading
him to leave a stump of greater than 5 mm behind.
Figure 3: Intraoperative image from initial laparoscopic appendectomy. Endo
GIA fired too high secondary to inadequate visualisation of appendicular
base.
Stump appendicitis continues to pose a diagnostic dilemma
both for surgeons and emergency department clinicians. We quickly
remove acute appendicitis from our differential diagnosis list in patients presenting with RIF pain when we learn they have had
previous appendectomy. The temporal relationship between index
appendectomy and onset of stump appendicitis is hugely variable
ranging from weeks to years which further complicates matters.
We can aim to limit the risk of stump appendicitis by encouraging
surgeons to adopt the CVS for appendectomy suggested by
Subramanian et al.