Journal of Surgery
Download PDF
Research Article
A Study of the Demography, Clinical Features and Management of Inguinal Hernia in a Tertiary Care Hospital
Sujan Narayan Agrawal*
- Department of Surgery, Late Shri BRKM Government Medical College, India
*Address for Correspondence: Sujan Narayan Agrawal, Department of Surgery, Late Shri BRKM Government Medical College, Chattisgarh-494 001, India, Tel: 09406070087/09009054353, Email: drsujanagrawal@gmail.com
Citation: Agrawal SN. A Study of the Demography, Clinical Features and Management of Inguinal Hernia in a Tertiary Care Hospital. J Surgery. 2018;6(2): 5.
Copyright: © 2018 Agrawal SN. This is an open access articledistributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 6, Issue: 2
Submission: 07 September, 2018| Accepted: 03 October, 2018 | Published: 10 October, 2018
Abstract
Background: An inguinal hernia is a common condition that affects all ages and both sexes. Its surgical management is also a common surgical procedure. The risk factor includes muscle weakness, COPD, Bronchial Asthma, heavy weight lifting, chronic constipation, pregnancy, obesity etc.
Patients and method: A retrospective analytical study was conducted on patients admitted to surgical units. The study includes 1086 surgical admissions. The 116 cases of inguinal hernias are studied and analyzed. An inguinal hernia confirmed by noting demographic profile, thorough clinical examination and necessary investigations.
Result: An inguinal hernia is more common in male as compared to female. In the present study out of 116 cases, 96.55% of the male is suffering from an inguinal hernia while this incidence is only 3.45% in female. The peak incidence is in <10 and 50+ age group. All the cases are managed by surgical intervention.
Conclusion: Inguinal hernias are a common cause of admission in the surgical unit. They also outnumber other surgical procedures. Their peak incidence is in paediatric age group and in 4th, & the 5th decade of life. The most accepted treatment is surgical intervention.
Keywords
Demographic profile; Herniorrhaphy; Mesh hernioplasty; Inguinal hernia risk factors; Strangulation
Introduction
Sir Astley Cooper defined a hernia in 1800 as “Hernia is a protrusion of any viscus from its proper cavity. The protruded part is generally contained in a sac-like structure formed by the membrane with which the cavity is naturally lined” Schwartz et al. defined a hernia as protrusion of a viscus through an opening in the wall of a cavity in which it is contained [1].
The word hernia is derived from the Latin word for “rupture”. A hernia constitutes an important public health problem and often poses a surgical dilemma even for the most skilled surgeon. They can be congenital or acquired, complete or partial, external or internal, reducible or irreducible, direct or indirect, and primary or recurrent. The various studies indicate that external hernias are more common than an internal hernia [2].
Evidence of surgical repair of inguinal hernia can be traced back to civilization of ancient Egypt and Greece [3]. Early management of inguinal hernia involved a conservative approach using trusses; however, the inefficiency of this approaches prompted the initiation of a surgical approach to the problem. As a consequence of primitiveness of the technique, the treatment was worse than the disease itself.
Failure of early techniques of hernia repair was based on inadequate knowledge of groin anatomy and poor understanding of the natural history of inguinal hernia formation. From late 1700 to early 1800s physicians such as Hasselbach, Cooper, Camper, Scarpa, Richter, and Gimbernat identified the vital component of inguinal region, and their contributions are reflected in the current nomenclature. By demonstrating a comprehensive understanding of the inguinal anatomy, Bassini (1844-1924) transformed inguinal hernia repair into a successful venture with minimal morbidity. The success of the Bassini’s repair over, any of its predecessors, ushered in an era of tissue based repairs. Modifications of Bassini’s repair were manifested in the McVay repair, as well as that of Shouldice repair.
Era of tissue based repair was supplanted by the tension- free repairs with the widespread acceptance of prosthetic materials for inguinal floor reconstruction. The repair capitalized on the concept of the mypectineal orifice of Fruchaud, which was based on the notion that whatever the type of inguinal hernia, the defect lay in the integrity of the transversalis fascia. This was superior to the previous tissue based repairs in that the weakness of the transversalis fascia could be restored by bridging the defect with mesh, rather than placing the tension between tissues to close the defect.
With the advent of minimally invasive surgery, inguinal hernia repair underwent its most recent transformation. Laparoscopic inguinal hernia repair has added to the armamentarium of the general surgeon, providing a technique that lessens the postoperative pain and improve recovery.
Irrespective of the approach to hernia repair, the current state of surgical treatment of the inguinal hernia depends on the sound foundation of the inguinal anatomy. The application of the current technologies to this anatomical knowledge has led to successful treatment of inguinal hernias with minimal morbidity and fast recovery.
Epidemiology
Inguinal hernia repair is one of the most commonly performed surgical interventions, owing to its lifetime incidence and a variety of successful treatment modalities. Majority of inguinal wall hernias occur in the groin. An inguinal hernia which is, among the most common of the abdominal wall hernia, accounting for almost 75% with a lifetime risk of 27% in men and 3% in women [4]. Of inguinal hernia repairs 90% are performed in males and 10% in females. Approximately 70% of femoral hernia repairs are performed in females [5].
Repair of an inguinal hernia is one of the most common operations in general surgery, with rates ranging from 10 per 100,000 of the population in the United Kingdom to 28 per 100,000 in the United States [6]. The incidence of inguinal hernia has a bimodal distribution with peaks before one year of age and then again after 40 years. The prevalence of abdominal wall hernia among all the age group is estimated to be 1.7% and 4% for those aged over 40 years.
The incidence of a groin hernia in adults is almost 12 times more common in male than in females. In men, the rate is 70 per 10,000 aged 45-64 years, rising to 150 per 10,000 aged 75+ years [7].
In 1973/4 10,000 patients underwent surgical repair of an inguinal hernia and there were 5600 repairs of a femoral hernia in the NHS in England [8].
The most common symptom of a hernia includes a swelling in the groin or inguinoscrotal swelling, with the visible expansion of swelling on coughing, lifting heavy weight, or standing/bending over. There may be heaviness or pain in the groin region. The patient may be asymptomatic and the hernia is incidentally detected in medical examination done for some other cause. The common causes of a groin hernia are muscle weakness, strain, chronic cough, constipation, weight lifting, obesity etc. The complications of a groin hernia include incarceration, obstruction, and strangulation. A complicated hernia is an emergency. The objective of this study is to determine the prevalence, clinical features, and treatment in a tertiary care hospital.
Patients and Method
Research design and sampling
The study was conducted on the patients admitted with the diagnosis of an inguinal hernia in the department of surgery, SBRKM Government medical college, Jagdalpur (Bastar) Chhattisgarh. The study period is from November 2016 to December 2017. A total of 116 patients were included in the study, out of 1086 surgical admissions. The study population consists of the inguinal hernia only, the other type of a hernia like femoral, abdominal wall hernia and internal hernias are excluded from the study.
Data collection
History taking is the first part of data collection. It includes identification of the patient, patient’s demographic profile like age, sex, marital status, residential address, relevant past history, chronic illness, addiction to tobacco, smoking etc.
All the patients underwent detailed clinical examination. The diagnosis is confirmed by clinical findings like inguino-scrotal swelling, impulse on coughing, deep ring occlusion test, ring invagination test, reducibility or otherwise of the swelling etc. The diagnosis confirmed by ultrasound studies. In rare cases when the diagnosis is in doubt help of computerized tomography/ magnetic resonance imaging is taken [9]. The diagnosis of an inguinal hernia is usually made through history and physical examination findings. The sensitivity and specificity of physical examination were 75% and 96% respectively [10].
A total of 116 Patients of different age and sex attending outpatients department and admitted to the surgical unit for operation of a hernia are included in this study. It consisted of unilateral and bilateral hernia, congenital and adult hernia and primary or a recurrent hernia. Presence of scar was taken as recurrence of a hernia. The study carried out for a period of fourteen months extending from November 2016 to December 2017.
Results
Sex wise distribution
In the present study, the inguinal hernia was present in 112 (96.55%) male and in 4 (3.45%) female. Rutkow et al. in his epidemiological study found that 90% of inguinal hernia repairs are done in males and only 10% in females. He found that 70% of femoral hernia repairs are performed in females in United States [5].
It is obvious that the incidence of an inguinal hernia is far more in male than in the female. It is a well-known fact that the femoral hernias are more common in female as compare to an inguinal hernia due to their wider pelvis.
Age of patients
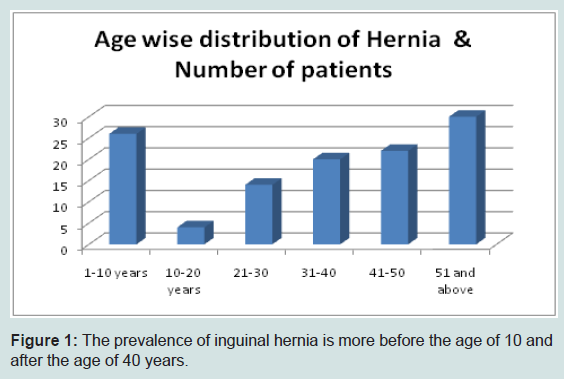
The first peak is in paediatric age group and they are congenital hernias due to patent process us vaginalis. In our study 26 (22.41%) patients were below 10 years of age. Most of the patients are above 30 years of age. 40-50 year age group and above is most affected. In this age group, we found 52 inguinal hernias out of 116 patients (44.82%). It means the hernias are common in their productive age group, and if not treated in time their earning capacity is affected considerably with the burden on the family and society. Incidence of inguinal hernia in male has a bimodal distribution with peaks before 1 year of age and then again after 40 years of age (Figure 1).
Figure 1: The prevalence of inguinal hernia is more before the age of 10 and after the age of 40 years.
Site wise distribution
It is found that the right sided hernia is more common than the left side. 83 (71.56%) patients are having right sided hernia and 32 (27.58%) patients have left sided hernia. One patient had a bilateral hernia (0.86%).
Co-morbidities
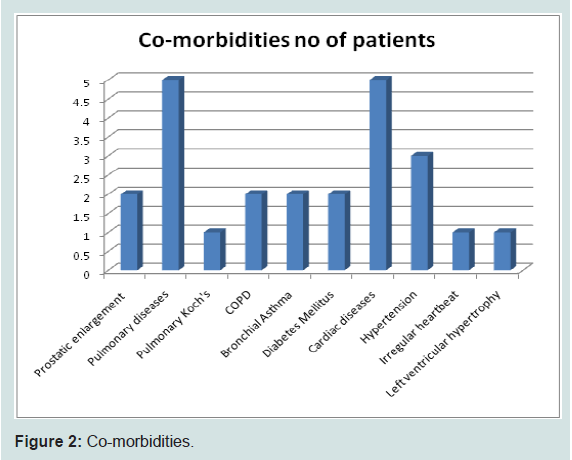
Co-morbidities noted in older patients and they mainly consist of hypertension, diabetes mellitus and pulmonary diseases like pulmonary Koch’s, COPD, Bronchial Asthma etc (Figure 2).
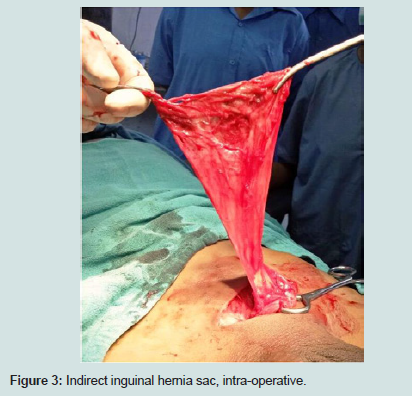
Presentation with complication
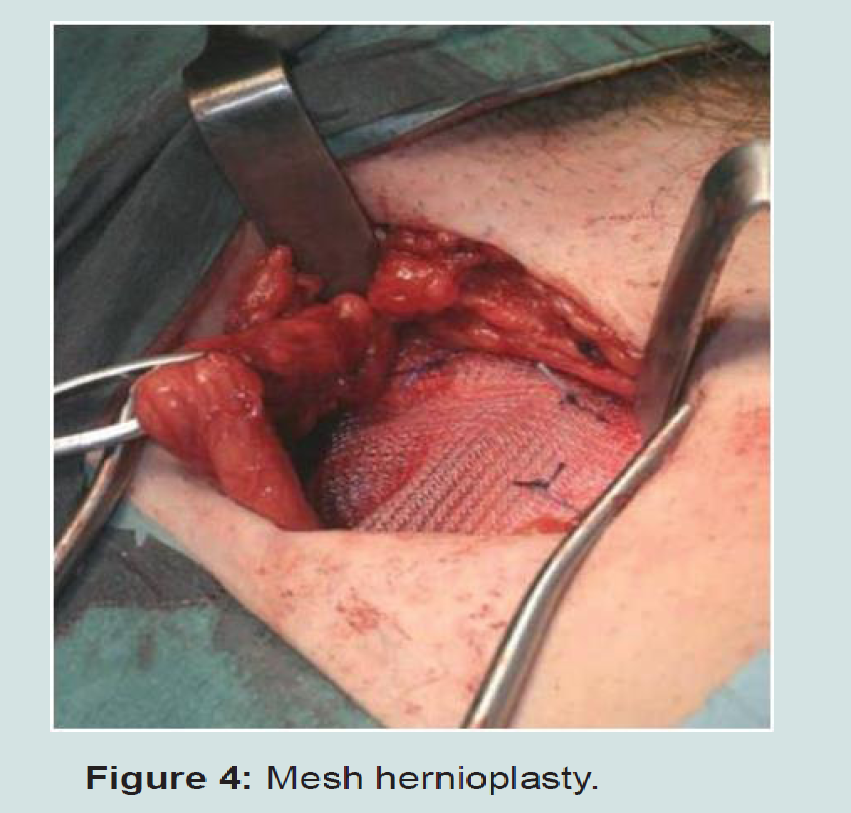
11 cases (9.4%) presented as an emergency. They presented with the obstructed hernia. After the investigation, they are taken for emergency surgery. The obstruction is relieved and after ensuring the viability of bowel, the contents are deposited in the abdomen. The preferred method of management is herniorrhaphy, since using mesh may be disastrous due to the presence of infection and tissue reaction. If the bowel strangulation is found, the preferred course of action is resection and anastamosis of the bowel. In case of strangulated omentum, omentectomy and herniorrhaphy is the operation of choice (Figures 3 and 4).
Management of an inguinal hernia is essentially surgical. At our institute, all adult hernias are managed by Lichtenstein mesh repair because the basic pathology is the weakness of post wall of the inguinal canal. A meta-analysis from the EU Hernia Trialists Collaboration compared mesh with sutured techniques from 58 trials comprising in total 11 174 patients [11].
Individual patient data were available for 6901 patients. Recurrence was less common after mesh repair (odds ratio 0.43 (95% confidence interval 0.34 to 0.55). A population-based study examining the risk of recurrence in five years or more after primary mesh (Lichtenstein repair) and sutured inguinal hernia repair in 13,674 patients found that recurrence after mesh repair was a quarter of that after sutured repair (hazard ratio 0.25 (0.16 to 0.40) [12].
Open repair is the preferred repair technique for primary inguinal hernia (by 96% of UK surgeons, 99% of Japanese surgeons, 95% of Danish surgeons and 86% of US surgeons [13].
A paediatric/congenital hernia is managed by herniotomy only. It is because the basic pathology is patent processus vaginalis and NOT the weakness of posterior wall of the canal [14].
Discussion
An inguinal hernia is a common surgical problem both in male and female and in almost all age group. Challenges in developing country include delayed clinical presentation of patientás due to ignorance and economic causes.
Inguinal hernia may be considered a congenital or acquired disease. In all likelihood, inguinal hernias in adult are acquired defect in the abdominal wall. Our study highlights the prevalence of a hernia; their causes, treatment, and complications in a tertiary care setup.
Most of the times the symptoms are manageable but the complicated hernias are very demanding and usually are managed in an emergency. The integrity of the abdominal wall is primarily dependent upon the strength of abdominal muscles and their conjoint tendons. These muscles assist respiration and control the expulsive forces of urination, defecation, coughing, and parturition. The contour and strength of the muscle depending on the age, muscle mass, muscle tone, obesity, intra-abdominal pathology, parity, posture etc. All these factors play a significant role in the formation of a hernia.
A number of studies have attempted to delineate the precise cause of inguinal hernia formation; one of the most intriguing areas under study is the role of tissue biology in hernia formation. There are very limited data available regarding the role of tissue biology in the causation of hernias. The microscopic examination of skin of inguinal hernia patients demonstrated significantly decreased ratio of type I to type III collagen. Type III collagen does not contribute to wound tensile strength as significantly as type I collagen. Additional analysis of similar skin revealed disaggregated collagen tracts with decreased collagen fibre density [15].
An inguinal hernia is more common in male, while a femoral hernia is more common in the female. Wide pelvis and repeated childbirth may be attributed to its prevalence (in female). Moreover, their internal ring is not wide since it admits only the round ligament. In the present study out of 116 cases 96.55% of male, are suffering from, an inguinal hernia while this incidence is only 3.45% in female. Gupta et al. reported an incidence of 96% male as compared to the female while Charles et al reported 93.2% of all the cases to be male [16,17].
On the analysis of age wise distribution, there are two peaks i.e. in the paediatric age group below 10 years of age and the second peak is 40-50 years and above. The study by Babar Sultan et al shows peak incidence of various hernias above 50 years of age [18].
Grosfeld JL has reported the incidence of inguinal hernias as 3% to 5% in term infants and 13% in an infant born at less than 33 weeks of gestational age [19].
In the present study, the incidence of right-sided hernia is 71.56% (83 patients) left sided is 27.58% (32 patients) and bilateral is 0.86% (1 patient) only. Ayesha Fatima et al. in her study found 58.8% right sided hernia, 31.3% left-sided and 5.25 hernias were bilateral. The study done by other authors like Charles, Bin Bisher Saeed also shows a higher prevalence of right sided hernia than left [20]. The probable cause of right sided predominance may be due to late descend of right testis and more frequent failure of closure of right processes vaginalis [21,22].
The classical teaching says that most of the unilateral hernias occur on right side. With the advent of the laparoscopic techniques, the contra- lateral side can also be examined without additional incision or trochar. In a study by Bochkarev et al. it was found that 22% of patients had an occult contra-lateral hernia during laparoscopic inguinal hernia repair. Although asymptomatic, at the time of diagnosis, these hernias have potential to become clinically significant as the patient ages [23].
The co-morbidities are found more in the age group of 50+ and above. The common co-morbidities are hypertension, diabetes mellitus, Bronchial Asthma, COPD, prostatic enlargement, constipation etc. All these causes are responsible for the chronic and intermittent increase of intra abdominal pressure. The presence of hypertension and diabetes mellitus increases the morbidity if not mortality.
The learning points
- Inguinal hernia is the most common surgical interventions.
- The prevalence has bimodal distribution i.e. in childhood and then, 40 year age group and after.
- Inguinal hernias are more common in male and femoral hernias in females.
- A proficient understanding of groin anatomy is essential to successful inguinal hernia treatment.
- Elective repair of inguinal hernia can be undertaken using a laparoscopic or open approach.
- The use of prosthetic mesh as a reinforcement significantly improves recurrence rate.
References
- Schwartz SI, Shires GT (1999) Principles of surgery. (7thedn). McGraw-Hill, New York, USA, pp. 2273.
- Fatima A, Mohiuddin MZ (2014) Study of incidence of inguinal hernias and the risk factors associated with the inguinal hernias in the regional population of a south Indian city. Int J Cur Res Rev 6: 9-13.
- Johnson J, Roth JS, Hazey JW, Pofahl WE (2004) The history of open inguinal hernia repair. Curr Surg 61: 49-52.
- Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362: 1561-1571.
- Rutkow IM (1998) Epidemiologic, economic and sociologic aspect of hernia surgery in the United States in the 1990s. Surg Clin North Am 78: 941-951.
- Devlin HB (1995) Trends in hernia surgery in the land of Astley Cooper. In: Soper NJ, (Ed), Problems in general surgery. Lippincott-Raven, Philadelphia, USA, 12: 85-92.
- Anonymous (1997) Digest of evidence: repair of a groin hernia in adults. J Clin Effectiveness 2: 22-23.
- Office of the population censuses and surveys (1995) Hospital episode statistics 1993/4. HMSO, London, Uk.
- Bickley LS, Prabhu FR (2003) Bates’ guide to physical examination and history taking. (8thedn). Lippincott Williams & Wilkins, Philadelphia, USA, pp. 359-372.
- Van den Berg JC, de Valois JC, Go PM, Rosenbusch G (1999) Detection of groin hernia with physical examination, ultrasound, and MRI compared with laparoscopic findings. Invest Radiol 34: 739-743.
- EU Hernia Trialists Collaboration (2002) Repair of a groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg 235: 322-332.
- Bisgaard T, Bay-Nielsen M, Christensen IJ, Kehlet H (2007) Risk of recurrence 5 years or more after primary Lichtenstein mesh and sutured inguinal hernia repair. Br J Surg 94: 1038-1040.
- Kingsnorth A (2005) Controversial topics in surgery: the case for open repair. Ann R Coll Surg Engl 87: 57-60.
- Agrawal SN (2017) Testicular descend, how and why: a review article. Int J Med Rev Case Rep 1: 23-27.
- Klinge U, Binnebosel M, Mertens PR (2006) Are collegens the culprit in the development of incisional and inguinal hernia disease? Hernia 10: 472-427.
- Gupta DK, Rohatgi M (1993) Inguinal hernia in children: and Indian experience. Pediatr Surg Int 8: 466-468.
- Charles NR, Christian LB, Sen T, Mahapatra S, Joshi BR (2000) A two year retrospective study of congenital inguinal hernia at western regional hospital Nepal. J Nep Med Assoc 39: 172-175.
- Sultan B, Qureshi Z, Malik MA (2009) Frequency of external hernias in Ayub Teaching Hospital Abbotabad. J Ayub Med Coll Abbotabad 21: 57-58.
- Grosfeld JL (1989) Current concepts in inguinal hernia in infants and children. World J Surg 13: 506-515.
- Saeed AB (2009) Inguinal Hernia Repair by Darning. Yemen J Med Sci 3: 1-5.
- Garba ES (2000) The pattern of adult external abdominal hernias in Zaria. Nigerian J Surg Res 2: 12-15.
- Mbah N (2007) Morbidity and mortality associated with inguinal hernia in north-western Nigeria. West Afr J Med 26: 288-292.
- Bochkarev V, RingleyC, Vitamvas M, Oleynikov D (2007) Bilateral laparoscopic inguinal hernia repair in patients with occult contralateral inguinal defects. Surg Endosc 21: 734-736.