Journal of Surgery
Download PDF
Case Report
*Address for Correspondence: Wenjie Zhong, University of New South Wales, Sydney, Australia, E-mail: great3811@hotmail.com
Citation: Zhong W, Kumar R. Trauma in a Developed Country: A Review from Both Surgical and Non-Surgical Perspectives. J Surgery. 2016;4(2): 4.
Copyright © 2016 Zhong W, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 4, Issue: 2
Submission: 29 November, 2016 | Accepted: 20 December, 2016 | Published: 26 December, 2016
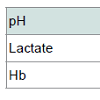
A diagnosis of cardiac tampenade and left hemopneumothorax was made immediately. Consequently, pericardio centesis was performed and a left chest drain was inserted. Within one hour, the former drained 500 ml of blood and the latter drained 1500 ml of blood. Arterial blood gas (Table 2) showed lactic acidosis (decreased pH and increased lactate). It had developed as a result of hypoperfusion secondary to excessive hemorrhage, where host cells responded by burning glucose anaerobically for energy, leading to lactate accumulation (Luft, 2001). The loss of blood was also consistent with the decreased hemoglobin (Hb) level (Table 2).
In cardiac tamponade, as shown in Figure 3, pericardial effusion and right-sided heart collapse are highly noticeable.
Trauma in a Developed Country: A Review from Both Surgical and Non-Surgical Perspectives
Wenjie Zhong* and Rakesh Kumar
- University of New South Wales, Sydney, Australia
*Address for Correspondence: Wenjie Zhong, University of New South Wales, Sydney, Australia, E-mail: great3811@hotmail.com
Citation: Zhong W, Kumar R. Trauma in a Developed Country: A Review from Both Surgical and Non-Surgical Perspectives. J Surgery. 2016;4(2): 4.
Copyright © 2016 Zhong W, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 4, Issue: 2
Submission: 29 November, 2016 | Accepted: 20 December, 2016 | Published: 26 December, 2016
Abstract
Introduction: Despite higher economic status and better societal infrastructure, trauma still persists in developed nations. The present paper is based upon a trauma case report, with aims to identify the unique social, cultural, economic and behavioral factors contributing to this health problem in Australia, as well as the relevant surgical anatomy for educational purposes.Case History: A twenty-six year old male patient presented to the emergency department with a stab wound to the left chest. The patient was found to have cardiac tamponade and hemopneumothorax, with resultant cardiogenic and hypovolemic shock. Patient was resuscitated and underwent definite surgical management, and ultimately had recovered well.
Discussion: Alcohol-related trauma is widespread even in a developed country such as Australia. The present paper discusses the cultural, economical and behavioral factors that contribute to the prevalence to the problem. Also discussed in the present paper are, relevant surgical anatomy and a systemic approach to manage trauma, for educational purposes.
Keywords
Trauma; Alcohol-related injury; Developed country; Cardiac tamponade; HemopneumothoraxIntroduction
Trauma is still prevalent in developed countries despite higher economic status and better societal infrastructure. The present paper is based upon a trauma case report, with aims to identify the unique social, cultural, economic and behavioral factors contributing to the persistence of trauma in Australia, as well as relevant surgical anatomy for educational purposes.History of Presenting Complaint
A twenty-six year old male patient was brought in by ambulance, with a stabbing injury to his left anterior chest wall following a fight at a bar. Upon arrival to the emergency department, patient was alert and complained of severe left anterior chest pain and shortness of breath. The pain radiated to the left shoulder, and had a score of 8/10. Collateral history from patient’s partner revealed that patient had two minutes of syncope on the ground. After regaining consciousness, the patient noticed active bleeding from a stab wound on his left chest.Retrospectively, patient remembered being involved in a fight after having approximately five standard drinks but was unable to recall the mechanism of the stabbing injury, neither did patient’s partner.
Patient denied any previous medical or surgical history, and did not have any allergy. Patient had a family history of ischemic heart disease.
Socially, patient lives with two friends, who are his main carers during hospitalization. Patient is a habitual smoker for the past twelve years, smoking one pack a day for the first ten years and two packs a day for the recent two years. He has been drinking alcohol for five years and routinely consumes four to five standard drinks twice a month before getting drunk. He has also tried cannabis and amphetamine out of curiosity.
Examination and Investigation
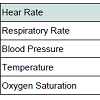
A trauma notification and massive transfusion protocol were initiated prior to patient’s arrival. Primary survey revealed a patent airway, with collar in-situ to protect C-spine. There was unequal air entry with diminished breath sound on the left side. No tracheal deviation noted. In terms of circulation, the patient appeared lethargic and pale, with prolonged capillary refilling time. Patient was tachycardic and in shock, evidently by non-recordable blood pressure and non-palpable femoral pulse (Table 1). The heart sound was muffled. A linear stabbed wound was noted in patient’s left anterior chest, measuring to approximately five centimeters. E-FAST ultrasound was performed which revealed pericardial tamponade, and moderate amount of left pleural effusion. Patient’s GCS was twelve (E3V4M5).A diagnosis of cardiac tampenade and left hemopneumothorax was made immediately. Consequently, pericardio centesis was performed and a left chest drain was inserted. Within one hour, the former drained 500 ml of blood and the latter drained 1500 ml of blood. Arterial blood gas (Table 2) showed lactic acidosis (decreased pH and increased lactate). It had developed as a result of hypoperfusion secondary to excessive hemorrhage, where host cells responded by burning glucose anaerobically for energy, leading to lactate accumulation (Luft, 2001). The loss of blood was also consistent with the decreased hemoglobin (Hb) level (Table 2).
Management
Concurrently, whilst awaiting surgical management, the emergency department was primarily focused on resuscitative measures, which included fluid resuscitation together with massive transfusion protocol. Patient had suffered a class III hemorrhage, as defined by his hypotensive, tachycardic and worsening mental status with evidence of peripheral hypoperfusion [1]. Besides aggressive intravenous crystalloid fluid infusion, patient received a total of sixteen units of red blood cells. One unit of platelets was also delivered to prevent thrombocytopenia. A secondary survey was performed to identify further co-existing injuries, which were fortunately not present.Subsequently, patient received urgent surgical care under the cardiothoracic team. An intraoperative transoesophageal echocardiography (TOE) was performed, which showed moderate pericardial effusion with right atrium (RA) collapse and large left pleural effusion. This was consistent with the diagnosis of cardiac tamponade and hemothorax [2].
Median sternotomy was performed to release the tamponade and patient’s hemodynamics improved gradually. Hemothorax was subsequently evacuated. A laceration on the left ventricle (LV) was also found and repaired primarily with non-absorbable monofilament suture.
Electrocardiography was applied to monitor patient’s cardiac functioning post-operatively. The mediastinal and left chest drains were in-situ to minimize blood accumulating in the pericardial and pleuralcavity. Imaging such as ultrasound and x-ray were done on a daily basis to monitor his recovery progress. Patient had been recovering well and was discharged within an expected time frame.
Discussion One
Relevant normal anatomy and its use in interpretation of clinical manifestations and findings on imagingThe anterior aspect of the heart consisting mostly of the right ventricle (RV)with some of the RA on the right and some of the LV on the left faces anteriorly (Figure 1A). The pleura surround the pericardium bilaterally (Figure 1B). Hence patient’s penetrating injury entering below the left nipple tore the pericardium and left pleura simultaneously, as well as lacerated the LV instead of the RV.
Subsequently, the accumulated blood in the pericardial space resulted in biventricular failure, leading to decreased cardiac output. Hence tachycardia developed to compensate. Similarly, the accumulated blood in the pleural cavities impaired the lung’s ability to expand, leading to dyspnea.
The patient’s radiating pain to his left shoulder can be explained by the fact that, parietal pericardium and pleura are both innervated by the phrenic nerves, in which, are responsible for somatic sensation [3]. For this reason, pain from pericardial and pleural problems may be referred to the supra clavicular region of the should error lateral neck area, dermatomes for spinal cord segments C3, C4, and C5.
Ultrasound echo cardiography can diagnose cardiac tamponade. For a normal person, a four-chamber heart can be seen clearly with intact valvular and septal structures (labeled in Figure 2) [4].
Figure 2: (A) Normal cardiac anatomy shown in echocardiogram; (B) Schematic diagram of the heart [7].
Hemothorax can also be visualized by ultrasound as seen in Figure 4, in which the lung is pushed smaller by the presence of blood in the supra diaphragmatic space.
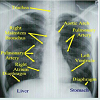
Cardiac tamponade and hemothorax can also be visualized through the chest X-Ray. An example of a normal chest x-ray labeling some thoracic anatomy is shown in Figure 5.
In cardiac tamponade, a chest X-Ray would reveal an enlarged globular cardiac shadow, which is suggestive of pericardial effusion as seen in Figure 6A. In hemothorax, the chest X-Ray shows features similar to pleural effusion as seen in Figure 6B.
Figure 6: (A) Cardiac tamponade; (B) Left hemothorax [4].
Discussion Two
Social, cultural, economic and behavioral factors contributing to the health problem or issueThe trauma in this case is alcohol-related, which accounts for about one-tenth of the global burden of disease [7]. They are divided into two categories: unintentional injuries, including road traffic injuries, drowning, burns, poisoning and falls; and intentional injuries, resulting from deliberate acts of violence against oneself or others [7]. Alcohol-related injury, as a health problem, is attributable to a number of factors. The following analyzes this issue from sociocultural, behavioral and economic points of view.
Sociocultural Factors
Australia has a deep-rooted culture of alcohol consumption. Since the late 19th century, economic prosperity, mass media, women and labor movements have all played a role in shaping the Australian drinking culture. These changes include, the shift from consumption predominantly by males to both genders; the positive framing of alcohol, with alcohol developing an identity with social events. As a result, some social venues in metropolitan are as such as King’s Cross in Sydney, have been transformed into uncomfortable, crowded and poorly managed drinking areas, where alcohol-related injuries rate are amongst the highest [8].In relation to Aboriginal and Torres Strait Islanders (ATSIs), many who were employed by non-indigenous people became involved in binge drinking after European colonization in Australia [9]. Despite legislation prohibiting certain population access to alcohol, this issue was not solved, and a trend of rapid consumption of high alcohol content beverages continued and exaggerated, which perpetuated the binge drinking cycle [10]. Currently, ASTIs are over-represented in arrests for drunkenness, and the risk of alcohol-related injuries is much higher.
Economical Factors
Previous studies have attempted to quantify the relationships between social-economic status, alcohol consumption and alcoholrelated harm. According to Australian Government Department of Health and Aging, a greater proportion of men living outside the capital cities in Australia consume harmful levels of alcohol, which relates to higher domestic violence rate with in these areas [11]. Another example is that young adults from families of lower socioeconomic status are at higher risks of having alcohol-related injuries than their counterparts [8]. The underlying reasons are lack of surveillance, poor education and peer influences [8].Behavioral Factors
Alcohol-related injuries occur as a result of behavioral impairment by intoxication. Hazardous alcohol use, such as binge drinking, reduces self-control and the ability to assess risks, making certain drinkers more likely to resort to violence in confrontation [8]. For instance, drunk driving was associated with other risktaking behavior such as driving too fast or not wearing a seat belt. Intoxicated drivers involved in fatal crashes were about three times as likely as sober drivers to be driving too fast or be unbelted [12]. Similarly, reduced physical control and impaired ability to recognize warning signs in potentially dangerous situations can make some drinkers easy targets for perpetrators [8]. In addition, the behaviors of drinkers have been influenced by societal beliefs about the effects of alcohol, including increasing self- confidence and aggression. This means that some individuals misuse alcohol as preparation for violence involvement [8].Conclusion
Alcohol-related trauma is widespread even in a developed country such as Australia. From an educational perspective, this paper examined the relevant surgical management techniques that are pertinent to patient care in trauma situations. It is of equal importance to appreciate the social, cultural, economic and behavioral factors contributing to alcohol-related injuries.References
- Cabañas JG, Manning JE, Cairns CB (2004) Fluid and blood resuscitation. In: Tintinalli JE, Stapczynski JS, Ma OJ, Cline DM, Cydulka RK, et al. (Eds.) Tintinalli's emergency medicine. A Comprehensive Study Guide, 7th edn, McGraw-Hill Medical, New York, USA.
- Braunwald E (2008) Pericardial disease. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, et al. (Eds.) Harrison's principles of internal medicine. 18th edn, McGraw- Hill, New York, USA.
- Drake R, Vogl W, Mitchell AW (2010) Gray’s anatomy for students. 3rd edn, Churchill Livingstone/Elsevier, Philadelphia, USA.
- Skandalakis JE, Colborn GL, Weidman TA, Foster RS, Kingsnorth AN, et al. (2004) Skandalakis' surgical anatomy. Paschalidis Medical Publications, Athens.
- Boyd JS, Rupp JD, Ferre RM (2010) Emergency ultrasound. In: Knoop KJ, Stack LB, Storrow AB, ThurmanRJ (Eds.), The atlas of emergency medicine. McGraw-Hill Medical, New York, USA.
- http://www.brooksidepress.org/.
- World Health Organization (2007) Alcohol and injury in emergency departments: summary of the report from the WHO collaborative study on alcohol and injuries. Department of Mental Health and Substance Abuse, Department of Injuries and Violence Prevention.
- World Health Organization (2006) Youth violence and alcohol. pp. 1-16.
- Brady M (1998) The grog book: strengthening indigenous community action on alcohol. Common wealth Department of Health and Family Services, Canberra, Australia.
- Bourbon D, Saggers S, Gray D (1999) Indigenous Australians and liquor licensing legislation. National Centre for Research into the Prevention of Drug Abuse, Curtin University, Perth, Western Australia.
- Ministerial Council on Drug Strategy (2001) Alcohol in Australia: issues and strategies.
- FORS (1996) Alcohol and road fatalities. Monograph 10, FORS, Canberra, Australia