Journal of Oral Biology
Download PDF
Case Report
*Address for Correspondence: Ana Sofia Silva Lopes, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, E-mail: asl486@nyu.edu
Citation: Sofia SLA, Ceballos L, Alqhtani M, Kim HM, Manasse M, et al. The Importance of the Appropriate Meso-Structure for the Success and Retention of Overdentures - Case Series. J Oral Bio. 2016; 3(1): 7.
Copyright © 2016 Sofia SLA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Oral Biology | ISSN: 2377-987X | Volume: 3, Issue: 2
Submission: 30 April 2016 | Accepted: 18 June 2016 | Published: 23 June 2016
Panoramic radiographs were obtained; and 4 to 6 implants were placed in the maxilla and mandible.
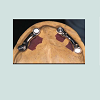
13. The Locator abutments (Zest Anchors, Escondido, CA, USA) were laser-welded on the meso-structure with a parallel path of insertion (Figures 7 and 8).
17. Postoperative instructions were given to the patient at the day of the new overdenture delivery including daily hygiene and maintenance care (Figure 10).
Clinical procedures (second group, old denture adjusted)
19. The overdenture was trimmed and polished. Occlusion was verified and adjusted.
The Importance of the Appropriate Meso-Structure for the Success and Retention of Overdentures - Case Series
Ana Sofia Silva Lopes*, Lara Ceballos, Mohammad Alqhtani, Hyun Min Kim, Maryse Manasse, Yung Cheng Paul Yu, Mazen Natour and Sang-Choon Cho
- Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York
*Address for Correspondence: Ana Sofia Silva Lopes, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, E-mail: asl486@nyu.edu
Citation: Sofia SLA, Ceballos L, Alqhtani M, Kim HM, Manasse M, et al. The Importance of the Appropriate Meso-Structure for the Success and Retention of Overdentures - Case Series. J Oral Bio. 2016; 3(1): 7.
Copyright © 2016 Sofia SLA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Oral Biology | ISSN: 2377-987X | Volume: 3, Issue: 2
Submission: 30 April 2016 | Accepted: 18 June 2016 | Published: 23 June 2016
Abstract
Lack of retention and stability is one of the most challenging problems in wearing conventional dentures due to the atrophy of the alveolar ridge. In addition, pain or discomfort can be frequently present with a poor load-bearing capacity of the tissues. The treatment of choice, among several options for edentulous patients is the implant-supported overdenture prosthesis. Locators have been the most popular method used as an unsplinted anchorage system. Poorly angled or unfavorably positioned implants cause lack of parallelism, resulting in compromised esthetics, phonetics, and function. The use of overdentures with meso-structures and paralleled Locator attachments is one option for solving this problem. The purpose of this report was to present a case series, and document a step-by-step procedure to fabricate overdentures with meso-structures and to discuss the indications, contraindications, advantages and disadvantages of meso-structures.Keywords
Overdenture; Meso-structure; Implant angulation; StabilityIntroduction
Lack of retention and stability is one of the most challenging problems in wearing conventional dentures due to atrophy of the alveolar ridges. In addition, pain or discomfort can be frequently present with a poor load-bearing capacity of the tissues [1].The treatment of choice, among the several treatment options for edentulous patients is the implant-supported over denture prosthesis. According to Hebel et al. the advantages of an implant supported over denture are 1) ease for oral hygiene procedures, 2) superior esthetics, 3) virtual elimination of denture movement enhancing function and phonetics, 4) the ability to remove the prosthesis at bedtime to reduce the effects of nocturnal parafunction, 5) increased masticatory efficiency when compared with complete dentures and 6) less critical implant position [2].
The implant-supported overdenture can achieve retention through splinted or unsplinted methods. Previously, the Hader bar (Sterngold Dental, Attleboro, MA, USA) or milled bar have been used to splint implants for over dentures. Recently, Locators have been the most popular method as an unsplinted anchorage system. Locators are less technique-sensitive, less expensive and more suitable for oral hygiene maintenance [3,4].
The accurate placement of implants is significant for getting an esthetically acceptable and functional overdenture. Poorly angled or unfavorably positioned implants cause lack of parallelism between implants, resulting in compromised esthetics, phonetics, and function [5-8]. Placing implants parallel in the maxilla is much more challenging due to the divergent nature of the alveolar housing. Several different methods have been suggested to correct misangulated implant placements during the prosthetic phases of treatment. The most common method is the use of angulated or custom abutments, which allows for positional correction (Allows the correction of 40º of divergence). However limitation still exists to achieve the ideal parallelism.
The use of overdentures with meso-structures (ODMS) is one option for solving this problem. The Meso-structure is fabricated by precision milling of casted frameworks [5-10 ]. Paralleled Locator attachments can becasted, screwed or laser-welded on the meso-structure in a more favorable position. In 2012, Kim et al. reported that implant overdenture using a locator bar system fabricated with the drill and tapping technique provided stability, support, and retention to dentures for fully edentulous patients [11]. However, considering the wide range of different intraoral locations of milled bars, there is a lack of information regarding the evaluation of meso-structures in various cases and the long-term maintenance [12-21].
Therefore, the purpose of this report was to present a case series and document a step-by-step procedure to fabricate over dentures with meso-structures (ODMS) and to discuss the indications, contra indications, advantages and disadvantages of meso-structures.
Materials and Methods
Patient selection Clinical data in this study was obtained from the Implant Database (ID). This data set was extracted as de-identified information from the routine treatment of patients at the Ashman Department of Periodontology and Implant Dentistry at New York University College of Dentistry. The ID was certified by the Office of Quality Assurance at New York University College of Dentistry. This study is in compliance of the Health Insurance Portability and Accountability Act (HIPAA) requirements.
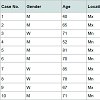
Between 2000 and 2015, 10 patients (i.e. 6 males, 4 females), mean age of 66 (i.e. range 40 to 85), received a total of 40 implants (Table 1). Inclusion criteria consisted of patients who were dissatisfied with their conventional dentures or previous overdentures due to lack of stability in functioncaused by misangulated implants. Patients with a history of alcohol abuse, drug dependency, smoking, bruxism, head and neck radiation treatment, poor health, or any other medical, physical, or psychologic factor that might affect the surgical procedure or the subsequent prosthodontic treatment and the required follow up examinations, were excluded from this study.
Clinical procedures (first group, new overdenture)
The milled meso-structures were CAD/CAM manufactured for all the patients; the first group of patients chose to have a newly fabricated overdenture to connect to the meso-structure. The second group, due to financial limitations had the old denture adapted to the milled meso-structure. The clinical procedures were documented according to these two groups.
1. A thorough clinical examination including the evaluation of the old overdenture (Figures 1-5), a panoramic radiograph and mounting of the diagnostic casts was completed.
2. A customized tray was used and the borders were molded with compound sticks. The posterior extension of the tray was determined by the location of the vibrating line.
3. Open tray impression copings were placed for each implant. Periapical radiographs were taken to verify the proper seating of the impression copings.
4. An open tray implant level impression was completed with the custom tray (Triad VLC System; Dentsply Trubyte, York, PA, USA) and with Hydrophilic Vinyl Polysiloxane impression material (Reprosil Regular body and Light body: Dentsply Trubyte, York, PA, USA) to record the position of the implants.
5. The implant analogs were attached to the impression copings.
6. A gingival replica was completed in silicone material (GI Mask; Coltene/Whaledent, Cuyahoga Falls, OH, USA), and the definitive cast was poured in Type IV die stone (ResinRock; Whip Mix Corp, Louisville, KY, USA).
7. A maxillary verification index was fabricated on the definitive cast with autopolymerizing acrylic resin (GC Pattern; GC-America, Alsip, IL, USA). The index was sectioned into segments on the definitive cast after complete polymerization.
8. Segments were evaluated individually intraorally and reconnected with acrylic resin. The accuracy of the definitive cast was then verified with the index.
9. The maxillary and mandibular casts were mounted on an articulator using the face-bow transfer and the interocclusal record of the vertical dimension.
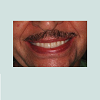
10. The position of the artificial teeth was established to allow the fabrication of a proper meso-structure. Therefore, a wax try-in of the selected artificial teeth was delivered to ensure the proper tooth position for lip support, esthetics, phonetics, and the interocclusal record was verified.
11. A CAD/CAM milling process was used to create the mesostructure.
12. Passive fit of the meso-structure was verified clinically and radiographically (Figure 6).
14. Another trial insertion appointment was made to verify the passive fit of the newly placed Locators on the meso-structure.
15. A conventional denture was fabricated in the maxilla.16. A metal housing was incorporated in the maxillary overdenture to provide additional strength (Figure 9).
17. Postoperative instructions were given to the patient at the day of the new overdenture delivery including daily hygiene and maintenance care (Figure 10).
Clinical procedures (second group, old denture adjusted)
1. A thorough clinical examination including a panoramic radiograph and mounting of diagnostic casts was accomplished.
2. The impression tray was customized to fit the maxillary arch (Triad VLC System; Dentsply Trubyte, York, PA, USA).
3. Open tray impression copings for each implant were placed. Periapical radiographs were taken to verify the proper seating of the impression copings.
4. An open tray implant level impression was completed with the custom tray (Triad VLC System; Dentsply Trubyte, York, PA, USA) and with Hydrophilic Vinyl Polysiloxane impression material (Reprosil Regular body and Light body: Dentsply Trubyte, York, PA, USA) to record the position of the implants.
5. The implant analogs were attached to the impression copings.
6. A gingival replica was completed in silicone material (GI Mask; Coltene/Whaledent, Cuyahoga Falls, OH, USA), and the definitive cast was poured in Type IV die stone (ResinRock; Whip Mix Corp, Louisville, KY, USA).
7. A maxillary verification index was fabricated on the definitive cast with auto polymerizing acrylic resin (GC Pattern; GC-America, Alsip, IL, USA). The index was sectioned into segments on the definitive cast after complete polymerization.
8. Segments were evaluated individually intraorally and reconnected with acrylic resin. The accuracy of the definitive cast was verified with the index.
9. The maxillary and mandibular casts were mounted on an articulator using the face-bow transfer and the interocclusal record of the vertical dimension.
10. A conventional milling process was used to create the mesostructure.
11. The passive fit of the meso-structure was verified clinically and radiographically.
12. The Locator abutments (Zest Anchors, Escondido, CA, USA) were fabricated on the meso-structure with a parallel path of insertion.
13. Another trial insertion appointment was made to verify the passive fit of the newly placed Locator on the meso-structure.
14. The existing denture was reduced from the intaglio surface to fit the meso-structure and the position of the new Locator attachments.
15. Vinyl Polysiloxane indicator material (Fit-Checker; GCAmerica, Alsip, IL, USA) was used to verify the clearance between the Locator attachments connected to the meso-structure and the old denture.
16. An impression using the old denture was completed with Hydrophilic Vinyl Polysiloxane (Heavy body: DentsplyTrubyte, York, PA, USA).
17. The cast was poured in Type III stone (Microstone; Whip Mix Corp, Louisville, KY, USA).
18. Denture repair material (Jet Denture Repair; Lang Dental, Wheeling, IL, USA) was poured inside the denture after the stone separator (Al-Cote; Dentsply Trubyte, York, PA, USA) was applied (Figure 11).
19. The overdenture was trimmed and polished. Occlusion was verified and adjusted.
20. Postoperative instructions were given to the patient, including daily hygiene and maintenance care.
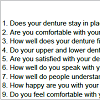
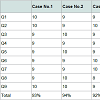
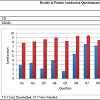
Follow up: A telephone interview with subjective evaluation was performed as follow-up. This interview included the patients’ evaluation of their previous dentures. In the present study, a Patient Satisfaction Questionnaire (PSQ) (Table 2) was used to evaluate and compare the grade of the patients’ satisfaction who had previously worn conventional dentures (CD) or overdentures.
Results
A total of 40 implants were placed in 10 patients. All 10 patients functioned with their ODMSs throughout the entire study period. Patient satisfaction questionnaire scores reported that ODMS resulted in improvement in stability (Q1), comfort (Q2), fitness (Q3 and Q4), occlusion (Q4), satisfaction (Q5, Q8), speech (Q6 and Q7) and social life (Q9) compared to the wearing of complete denture (Tables 3 and 4).Discussion
All patients functioned well with overdentures with mesostructures. The patients, who mentioned being more satisfied with ODMSs than their previous conventional maxillary dentures, were willing to undergo the surgical and prosthetic treatment again if needed and would suggest ODMSs to friends and relatives with comparable problems of wearing a conventional maxillary denture.The use of angled abutments is one of the methods to correct implant angulation because of low cost and reduced chair time [13]. However, the customized abutments seem to provide better results than angled abutments for ideal crown contours and peri-implant soft tissue support [14]. Among the variety of custom abutments that can be satisfactorily utilized for implant-retained prostheses, the UCLA castable type is one of the most popular. This abutment consists of a plastic cylinder that directly connects to the implant and may be customized by waxing and casting using a base metal alloy such as cobalt-chromium [15]. Its low cost, ability to overcome problems such as limited inter-occlusal spaces and small interproximal distances between implants, and the possibility of implant angulation error correction are its main advantages. However, a drawback of this abutment is that the required laboratory steps could cause implant/abutment misfit, which may result in screw loosening and/or fracture [16]. The use of UCLA Locator abutments may have contributed to the high frequency of prosthetic complications because their casting procedures are very technique-sensitive and may have somewhat altered the fit at the implant/abutment interfaces [16].
Traditionally, implant frameworks were fabricated using the lostwax technique and casting noble alloys. It has been well established that casting errors may be corrected using various soldering techniques. If a clinical passive fit was not obtained, frameworks should be sectioned, an intraoral index made, and then the segments should be re-soldered [17]. CAD/CAM frameworks have been found to fit more accurately than frameworks cast with gold alloys. Multiple studies have reported that CAD/CAM titanium frameworks achieve superior fit to the implant/abutment versus those obtained with cast metal frameworks [18-23]. Moreover, titanium and its alloys are difficult to cast due to their high melting points, low density, and reactivity with elements in casting investments. Porcelain veneer fractures were also common technical complications in implant-supported zirconia restorations. Porcelain veneer failures were related to differences in coefficients of thermal expansion between core and veneering porcelains, and their respective processing techniques [17].
According to the results, the ODMS is shown to have excellent stability and resistance to lateral and rotational forces. The attachments provide retention along the path of insertion. The selection of simple and ease to replace attachments simplifies maintenance. The fact that the prosthesis is detachable by the patient allows easier oral hygiene, and at the same time provides similar stability and increased masticatory efficiency as a fixed restoration. Furthermore, superior esthetics and phonetics are noticeable benefits not always obtained with fixed prostheses. The anterior-posterior spread of the implants will allow for an extension of the cantilevers to the area of the first molar. In most situations, this will approximate a cantilever length of 15 mm [2].
Unfortunately, ODMSs usually require more appointments and are technique sensitive when fabricating the prosthesis [3]. Also, the restoration of the edentulous arch requires a certain amount of vertical space between the opposing arches to ensure adequate restorative material thickness, space for the retentive elements, esthetics, and cleansability. The estimated interarch space required for an implant retained overdenture measured from the implant shoulder to the incisal edge is approximately 12 to 14 mm. 2 to 3 millimeters of soft tissue thickness is generally present above the implant, 2 mm of space from the edentulous ridge mucosa to the bar is recommended for cleansability, 4.5 mm for the height of the bar, 2 mm for the acrylic resin and metal housing, and 3 mm for the teeth above the denture base [24-26].
Conclusion
In this study, the overdentures with meso-structures (ODMSs) provided excellent stability and resistance to lateral and rotational forces with high survival rates. When asked to evaluate the ODMSs, patients reported an increase in comfort, function, stability, fit, occlusion, satisfaction, phonetics, and social life over an average of 48 months (Figure 12). To date, the use of ODMSs in the maxilla and mandible has shown excellent results. Further studies are required to determine long-term success and predictability of this treatment modality and possible applicability for ODMSs.References
- Visser A, Raghoebar GM, Meijer HJ, Vissink A (2009) Implant-retained maxillary overdentures on milled bar suprastructures: a 10-year follow-up of surgical and prosthetic care and aftercare. Int J Prosthodont 22: 181-192.
- Hebel KS, Galindo D, Gajjar RC (2000) Implant position record and implant position cast: minimizing errors, procedures and patient visits in the fabrication of the milled-bar prosthesis. J Prosthet Dent 83: 107-116.
- Lin WS, Özdemir E, Morton D (2012) A three-appointment alternative treatment protocol for fabricating an implant-supported milled bar overdenture. J Prosthet Dent 107: 75-79.
- Lee JH, Frias V, Woo C, Maiberg R (2007) Fixed prosthesis with a milled bar for correcting misangled implants: a clinical report. J Prosthet Dent 97: 129-132.
- Krennmair G, Piehslinger E (2009) Removable implant-supported maxillary prostheses anchored on milled bars: a retrospective evaluation of two concepts. Int J Prosthodont 22: 576-578.
- Krennmair G, Krainhöfner M, Piehslinger E (2008) Implant-supported maxillary overdentures retained with milled bars: maxillary anterior versus maxillary posterior concept--a retrospective study. Int J Oral Maxillofac Implants 23: 343-352.
- Kim MS, Yoon MJ, Huh JB, Jeon YC, Jeong CM (2012) Implant overdenture using a locator bar system by drill and tapping technique in a mandible edentulous patient: a case report. J Adv Prosthodont 4: 116-120.
- Davodi A, Nishimura R, Beumer J 3rd (1997) An implant-supported fixedremovable prosthesis with a milled tissue bar and Hader clip retention as a restorative option for the edentulous maxilla. J Prosthet Dent 78: 212-217.
- Krennmair G, Krainhöfner M, Piehslinger E (2008) The influence of bar design (round versus milled bar) on prosthodontic maintenance of mandibular overdentures supported by 4 implants: a 5-year prospective study. Int J Prosthodont 21: 514-520.
- Moeller MS, Duff RE, Razzoog ME (2011) Rehabilitation of malpositioned implants with a CAD/CAM milled implant overdenture: a clinical report. J Prosthet Dent 105: 143-146.
- Rossetti PH, Bonachela WC, Rossetti LM (2010) Relevant anatomic and biomechanical studies for implant possibilities on the atrophic maxilla: critical appraisal and literature review. J Prosthodont 19: 449-457.
- Bedrossian E, Stumpel L 3rd, Beckely ML, Indersano T (2002) The zygomatíc implant: preliminary data on treatment of severely resorbed maxillae. A clinical report. Int J Oral Maxillofac Implants 17: 861-865.
- Dario LJ (2002) A maxillary implant overdenture that utilizes angle-correcting abutments. J Prosthodont 11: 41-45.
- Borges T, Lima T, Carvalho A, Dourado C, Carvalho V (2013) The influence of customized abutments and custom metal abutments on the presence of the interproximal papilla at implants inserted in single-unit gaps: a 1-year prospective clinical study. Clin Oral Implants Res 25: 1222-1227.
- Krennmair G, Suto D, Seemann R, Piehslinger E (2012) Removable four implant-supported mandibular overdentures rigidly retained with telescopic crowns or milled bars: a 3-year prospective study. Clin Oral Implants Res 23: 481-488.
- Montero J, Manzano G, Beltrán D, Lynch CD, Suárez-García MJ, et al. (2012) Clinical evaluation of the incidence of prosthetic complications in implant crowns constructed with UCLA castable abutments. A cohort follow-up study. J Dent 40: 1081-1089.
- Drago C, Howell K (2012) Concepts for designing and fabricating metal implant frameworks for hybrid implant prostheses. J Prosthodont 21: 413-424.
- Krennmair G, Krainhöfner M, Piehslinger E (2008) The influence of bar design (round versus milled bar) on prosthodontic maintenance of mandibular overdentures supported by 4 implants: a 5-year prospective study. Int J Prosthodont 21: 514-520.
- Torsello F, di Torresanto VM, Ercoli C, Cordaro L (2008) Evaluation of the marginal precision of one-piece complete arch titanium frameworks fabricated using five different methods for implant-supported restorations. Clin Oral Implants Res 19: 772-779.
- Spyropoulou PE, Razzoog ME, Duff RE, Chronaios D, Saglik B, et al. (2011) Maxillary implant-supported bar overdenture and mandibular implant-retained fixed denture using CAD/CAM technology and 3-D design software: a clinical report. J Prosthet Dent 105: 356-362.
- Drago C, Saldarriaga RL, Domagala D, Almasri R (2010) Volumetric determination of the amount of misfit in CAD/CAM and cast implant frameworks: a multicenter laboratory study. Int J Oral Maxillofac Implants 25: 920-929.
- Drago CJ, Peterson T (2007) Treatment of an edentulous patient with CAD/ CAM technology: a clinical report. J Prosthodont 16: 200-208.
- Goodacre CJ, Garbacea A, Naylor WP, Daher T, Marchack CB, et al. (2012) CAD/CAM fabricated complete dentures: concepts and clinical methods of obtaining required morphological data. J Prosthet Dent 107: 34-46.
- Pasciuta M, Grossmann Y, Finger IM (2005) A prosthetic solution to restoring the edentulous mandible with limited interarch space using an implant-tissuesupported overdenture: A clinical report. J Prosthet Dent 93: 116-120.
- Cho SC, Froum S, Tai CH, Cho YS, Elian N, et al. (2007) Immediate loading of narrow-diameter implants with overdentures in severely atrophic mandibles. Pract Proced Aesthet Dent 19: 167-174.
- Weinländer M, Piehslinger E, Krennmair G (2010) Removable implantprosthodontic rehabilitation of the edentulous mandible: five-year results of different prosthetic anchorage concepts. Int J Oral Maxillofac Implants 25: 589-597.