Journal of Nutrition & Health
Download PDF
Research Article
*Address for Correspondence: Teruyoshi Amagai, Department of Human Environmental Sciences, School of Human Environmental Sciences, Mukogawa Women’s University, Nishinomiya, Hyōgo, Japan, Tel: 81798459855; E-mail: amagait@nutrped.com
Citation: Itoh M, Nishimoto Y, Masui H, Etani Y, Takagishi K, et al. Addition of Alpha-Amylase and Thickener to Blenderized Rice Provides Suitable Viscosity for Use in Nutritional Support. J Nutri Health. 2016;2(1): 7.
Copyright © 2016 Amagai et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Nutrition and Health | ISSN: 2469-4185 | Volume: 2, Issue: 1
Submission: 12 April, 2016 | Accepted: 30 April, 2016 | Published: 05 May, 2016
Method 3
Results 4
Addition of Alpha-Amylase and Thickener to Blenderized Rice Provides Suitable Viscosity for Use in Nutritional Support
Mao Itoh1, Yukiko Nishimoto2, Hiroshi Masui1, Yuri Etani3, Kazuko Takagishi1, Shinobu Ida3 and Teruyoshi Amagai4*
- 1Master’s Program, Administration Food Sciences and Nutrition Major, Graduate School of Human Environmental Sciences, Mukogawa Women’s University, Osaka, Japan
- 2Department of Nutrition, Osaka Medical Center and Research Institute for Maternal and Child Health, Hyōgo, Japan
- 3Department of Pediatric Gastroenterology, Nutrition and Endocrinology, Osaka Medical Center and Research Institute for Maternal and Child Health, Hyōgo, Japan
- 4Department of Human Environmental Sciences, School of Human Environmental Sciences, Mukogawa Women’s University, Hyōgo, Japan
*Address for Correspondence: Teruyoshi Amagai, Department of Human Environmental Sciences, School of Human Environmental Sciences, Mukogawa Women’s University, Nishinomiya, Hyōgo, Japan, Tel: 81798459855; E-mail: amagait@nutrped.com
Citation: Itoh M, Nishimoto Y, Masui H, Etani Y, Takagishi K, et al. Addition of Alpha-Amylase and Thickener to Blenderized Rice Provides Suitable Viscosity for Use in Nutritional Support. J Nutri Health. 2016;2(1): 7.
Copyright © 2016 Amagai et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Nutrition and Health | ISSN: 2469-4185 | Volume: 2, Issue: 1
Submission: 12 April, 2016 | Accepted: 30 April, 2016 | Published: 05 May, 2016
Abstract
Background: Blenderized diets have been widely adopted as nutritional support, particularly for patients receiving formulae via an enteral route. Although the viscosity of thickened formulae is a determinant of adverse events, no study has examined the viscosity of blenderized diets.Aim: To examine the viscosity and temperature of four types of blenderized diet.
Methods: Four types of rice porridge were prepared: rice porridge (RP) (Method 1); rice porridge with 0.5% alpha-amylase (RPA) (Method 2); rice porridge with 0.5% alpha-amylase and 0.5% thickener (RPAT) (Method 3); and rice porridge with 0.5% alpha-amylase and 0.5% thickener frozen overnight and defrosted (RPATFD) (Method 4). The viscosity and temperature of these four types of blenderized diet were measured for 30 minutes with a B-type viscometer.
Results: The viscosity of blenderized diets over 30 minutes increased with decreasing temperature with Methods 1, 3, and 4. With Method 2, viscosity at 5 minutes was significantly lower than that with Method 1 (p < 0.05). Moreover, unlike the other three methods, viscosity with Method 2 decreased significantly over the 30 minutes (p < 0.05). This phenomenon might have been related to the activation of added amylase. Viscosity during the 30 minutes was within the range of 3,500-10,000 mPa.s, which is reported acceptable in clinical settings. Overnight freezing and defrost of the blenderized diet in Method 4 appeared to stably maintain the viscosity within the likely acceptable range achieved with Method 3.
Conclusion: The addition of 0.5% thickener with 0.5% alphaamylase, either alone or followed by overnight freezing followed by defrosting, appeared to stably maintain the viscosity of a blenderized diet within the range likely acceptable in clinical settings. These findings might aid in the development of clinically usable blenderized diets.
Keywords
Blenderized diet; Viscosity; Temperature; Enteral feedingIntroduction
Registered dietitians in pediatric nutritional practice often encounter healthcare issues with severely handicapped children returning home after an extended period of hospitalization. Severely disabled children have difficulty in their intellectual ability and movement. Moreover, it is essential to provide enteral feeding immediately after birth because of dysphagia accompanying impairment of the central nervous system. Therefore, the first prescription diet must often be based on enteral nutrient formulae, which might lower their QOL. In addition, the use of a liquid nutritional supplement often results in multiple clinical complications which can might impair the growth and development of the child, such as vomiting, nausea [1].Against this background, thickened formula (TF) has been widely adopted as a novel type of nutritional support, particularly in preventing adverse events in clinical settings [2-4]. Two types of TF are available in ordinary clinical settings, mainly in developed countries such as the United States [2-7], a liquid type and a blenderized diet (BD). TF with a viscosity close to that of chewed foodstuffs is reported to be absorbed and digested normally [8,9]. Although the viscosity of these diets is considered a determinant of adverse events in clinical settings, such as diarrhea and symptoms related to gastro-esophageal reflux disease [2-4], the reports on the viscosity of blenderized diets (BDs) has not been conducted. Teresa et al. evaluated the clinical necessity and feasibility of BDs in clinical settings via a questionnaire survey of registered dietitians (RDs) belonging to the Pediatric Nutrition Practice Group, with particular regard to clinical experience with blenderized whole foods, defined as BDs with whole diets as included in the present study [10]. More than half (57.6%) of responding RDs considered that blenderized whole diets were the most suitable type of diet for administration via an enteral tube, and most parents (70.2%) wished to use them, with only 6.1% of parents preferring the use of natural, non-chemical foods. This survey suggests that blenderized whole diets might be considered the leading option for patients with an enteral tube.
In clinical settings, caregivers often utilize BDs administered through an enteral tube to provide required nutrients to patients on a daily basis.
For the patients with head and neck cancers, evidences with thickened liquids are extremely limited [11]. Additionally, not thicken liquid but puree like Nectar was proved to be able to swallow without aspiration [12]. However, the studies on the effect of viscosity of the diets putting directly into the stomach without swallowing in patients with swallowing difficulties are not conducted by the present study. To our knowledge, the present study is the first to examine the viscosity of BDs.
Here, to better understand the use of BDs in clinical settings, we analyzed the viscosity of various fundamental BD formulae.
Methods
Preparation of blenderized dietsEighty grams of milled white rice (Tamba Sasayama Koshihikari brand; Hyogo Prefecture, Japan) was washed with 400 ml of water at a temperature between 28-30 °C, drained with a sieve, combined with a further 400 ml water and cooked by boiling with a rice cooker (“RC-10MM”, Toshiba Corporation, Tokyo, Japan). Cooking was conducted using the automatic setting of the rice cooker, under which the rice was soaked for 30 minutes to absorb water followed by steaming for 75 minutes (Figure 1). The rice was stored at 15 °C before use according to a previous report [13].
The four methods below were designed to determine whether the various types of rice porridge could be prepared within the viscosity and temperature ranges acceptable for easy and safe delivery to patients through an enteral tube. Following preparation using Methods 1-4, the viscosity and temperature of the four types of rice porridge were measured by stirring with a blender (Braun MR730CC Multi Quick 7 cordless hand blender, De’ Longhi Japan Corporation, Tokyo, Japan).
Method 1
Rice porridge (RP): Boiled rice porridge (RP, Figure 1) was stirred with the blender using a stirring speed of 5,400±1,000 rate per minute (rpm). The viscosity and temperature of the RP were then measured every 15 seconds for the next 30 minutes.
Method 2
Addition of 0.5% alpha-amylase to RP (RPA): To ensure RP reached the reported target viscosity range (7), 0.5 w/w% of alpha-amylase was added to the RP and the mixture was stirred for 60 seconds with the blender (Figure 2). In this study, the 0.5% concentration was adopted based on the experimental preliminary finding on the addition of 0.125%, 0.25%, or 0.5% concentrations of alpha-amylase to RP that 0.5% had a standard deviation less than 0.5% (Figure 3). Alpha-amylase (Kissei Pharmaceutical Company Limited, Nagano, Japan) is composed of alpha-amylase 0.2% and dextrin 99.8%. Alpha-amylase products were selected based on their easy market availability as an enzymatic product for food adjustment in nursing care settings.
Method 3
Addition of 0.5% thickener to materials used in Method 2 (RPAT): To ensure that the viscosity of materials used in Method 2 reached the previously reported target range [14], 0.5 w/w% thickener (Cliniko Company Limited, Tokyo, Japan) was added to RPA, and the mixture was stirred for 60 seconds as in Method 2 (Figure 2). Components of this thickener were dextrin, glucomannan, xanthan gum, carrageenan, gellan gum, and locust bean gum. This thickener was selected because of its heating-free characteristics and wide use in clinical settings, especially in home-nursing care.
Method 4
Effect of freezing and defrosting on the material used in Method 3 (RPATFD): To ensure these observations reflected ordinary clinical settings, in which blended diets are frozen for storage and then defrosted before via enteral tube delivery, we also evaluated these materials under a freeze/defrost cycle. RPAT used in Method 3 was frozen overnight followed by defrosting. Freezing conditions were as follows: storage for 6 hours at -12 °C in a domestic freezer (R-23RA, Hitachi, Co. Ltd. Tokyo, Japan), followed by defrosting by warming in a microwave oven (NE-NS60, Panasonic Co. Tokyo, Japan) at 500 W for 4 minutes. Viscosity and temperature were then measured every 15 seconds for the next 30 minutes.
Measurement of viscosity and temperature
Viscosity and temperature were measured using a B-type viscometer (Brookfield Viscometer BasePlus No. 6701, Corporation Atago Headquarters, Tokyo, Japan) every 15 seconds for 30 minutes. For instance, average viscosity and temperature value at 5 minutes were presented as the average of 5 measurements. Viscosity and temperature at 0 minutes are not described, because recording started at 5 minutes. Measurement was conducted under the following conditions: room temperature 26-28 °C, sample amount 200 ml, glass container height 11.8 cm and diameter 6.7 cm. Measuring position of the sample and rotor is shown in Figure 4. The range of rotational speed and rotor torque were checked at the start and end of each measurement to ensure that they met the acceptable range of 15% to 100% of the validated measurement range. Accordingly, we set torque speed at 20 rpm for Methods 1, 3 and 4, and 4 rpm for Method 2. The torque speed and rotor in Method 2 must be decreased from 20 to 4 rpm in order to ensure torque range is within 15% and 100%.
Relationship between viscosity and temperature was measured by correlation analysis and expressed at 5-minute intervals for up to 30 minutes. Results are shown as the mean±standard deviation. Changes in viscosity and temperature over time were tested using the Friedman nonparametric test. Change in viscosity between samples was measured using the Kruskal-Wallis non-parametric test. Temperature and viscosity were correlated using Spearman’s correlation coefficient for non-parametric variables. Differences of p < 0.05 were considered statistically significant.
Results
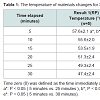
Results 1Rice porridge (RP): Viscosity of RP was significantly higher at 5 minutes than at 25 minutes or 30 minutes, (P < 0.01) (Figure 5). Temperature of RP was also significantly higher at 5 minutes than at 25 minutes or 30 minutes (P < 0.05) (Table 1). We speculate that these results represent the phenomenon of “higher viscosity with lower temperature”.
Addition of 0.5% alpha-amylase to RP (RPA): Viscosity of RPA at 30 minutes was significantly lower than that at 5 minutes (P < 0.05) (Figure 5). This decreasing tendency was observed with Method 2 only. Viscosity measured at 30 minutes with Method 2 was significantly lower than that at 5 minutes (P < 0.05) (Figure 5). The temperature of RPA measured at 30 minutes also significantly lower than that at 5 minutes (P < 0.01) (Table 1). Viscosity appeared to decrease as temperature decreased. This positive relation between viscosity and temperature was observed only with Method 2.
Results 3
Addition of 0.5% thickener to materials used in Method 2 (RPAT): Viscosities of RPAT at 30 minutes was significantly higher than that at 5 minutes (P < 0.05) (Figure 5). The temperature of the experimental material (RPAT) decreased with time, similarly to the findings with other methods (Table 1).
Results 4
Effect of freezing and defrosting on the material used in Method 3 (RPATFD): Contrary to our expectation, the viscosity and temperature of RPAT remained stable after overnight freezing and defrosting, and did not significantly change during the 30-minute observation period. This result might show that overnight freezing of RPAT material stabilized its viscosity within the acceptable range in clinical settings for at least 30 minutes.The results of Method 3 and Method 4 did not significantly differ, at least during the first 10 minutes (Figure 6).
Correlation coefficients between the viscosity and temperature of materials in Methods 1, 2, 3, and 4 were p < 0.001, R=-0.644; p < 0.001, R=0.794; p=0.59; R=-0.328, and p < 0.001, R=0.624, respectively. These negative Rs in Methods 1 and 3 show the negative correlation that viscosity increases as temperature decreases. In contrast, a positive correlation R means that viscosity decreases as temperature decreases, as observed in Methods 2 and 4.
Discussion
Although the use of thickened enteral formulae has been reported to lower the incidence of adverse events, such as diarrhea, vomiting and weight loss [2-4], a mechanism to explain these nutritional advantages has not been described. One possibility is that viscosity is raised: to prevent adverse events with non-thickened ordinary formulae. In clinical settings, caregivers often utilize blenderized whole diets delivered through an enteral tube to provide nutrients for patients [5-7]. Higher or lower viscosity BDs might be considered unsuitable, for instance due to the difficulty entailed in pushing higher viscosity diets through an enteral tube and more frequent tube blockage. In contrast, excessively low-viscosity diets might induce diarrhea or vomiting, leading to the failure to provide nutritional support. Accordingly, optimum viscosity might lie within a narrow range, such as between the 3,500-10,000 mPa.s reported to prevent adverse events [14]. Although blenderized whole diets are mainly used in clinical settings, particularly in home care, we chose a simple diet instead of a whole diet with a naturally heterogeneous composition [5-7] to better illustrate the basic principal underlying the viscosity of blenderized whole diets. We selected rice porridge as suitable for this purpose.The results of Method 1 can be summarized to state that the viscosity of simply prepared rice porridge is markedly higher than the 10,000 mPa.s reported as the upper limit of the acceptable range (AR) of 3,500-10,000 mPa.s in clinical settings [14]. We then added Method 2 to lower viscosity to the acceptable range. Contrary to our expectations, however, results exceeded the lower limit of AR (Figure 5). Method 3 was therefore included, in which thickener was added to the material used in Method 2. The results observed with Method 3 appear within the acceptable AR (Figure 5). For Method 4, the experimental material used in Method 3 was frozen overnight and then defrosted to reflect home care settings. Method 4 also met the AR (Figure 5). These results can be summarize in three ways: (1) the viscosity of ordinary rice porridge might be higher than the AR; (2) RP, with 0.5% alpha-amylase, appears lower than the AR; and (3) RP with alpha amylase and a 0.5% thickener with freezing and defrosting appeared to meet the AR. Method 4 might be suitable for use in clinical settings.
We also measured the temperatures of the experimental materials in all four methods, given the effect of temperature to decrease viscosity [15]. Although the mechanism of this effect of temperature on viscosity is unknown, the added amylase in Methods 2, 3, and 4 might have played a role. With Method 2, where the viscosity and temperature decreased with time elapsed contrary to the other three methods, amylase contained in the materials is thought to be activated, resulting in the decreasing tendency in viscosity (Table 1). For Methods 1, 2, and 3, the temperature and viscosity of experimental materials differed significantly between at the timing of 5 minutes and 30 minutes, whereas they did not differ in Method 4 (Figure 5, Table 1), suggesting that the temperature of the BDs might a determinant of viscosity. To our knowledge, this is the first report to have proved the relation between the viscosity and temperature of the four different types of RP as the simplest models of BDs.
Another aspect of these findings should be considered. In Method 4, the viscosity of the material did not change according to changes in temperature, whereas their viscosity did not change significantly over time of experimental period (Figure 5 and Table 1). This observation might be interpreted to mean that the freeze/defrost cycle stabilized viscosity, allowing it to meet the AR for clinical settings. The mechanism of this effect warrants further investigation.
Several limitations of the present study should be mentioned. First, the physiological and nutritional composition of the experimental material was simplified to facilitate analysis. In clinical practice, however, more complicated BDs are administered. The viscosity and clinical outcomes with BDs should also be analyzed. Second, although viscosity of the material in all four methods was measured after stirring, stirring conditions, such as speed and torque, differed between Method 2 and the others, because the measurement range depended on these conditions being met within the narrow range of the rheometer used, namely the viscometer type B. As different conditions might show different results, further studies should examine different viscometers and different types of BDs, which would in turn reveal the physiological and nutritional characteristics of a wide range of BDs. Such studies should include careful recording of observations result of BDs viscosity, including viscosity measurement conditions, such as type of viscometer. Third, experimental numbers for each method were limited. Although an optimum number might be difficult to determine, and would be subject to financial, human, and time limitations, more examinations would provide stronger evidence. Fourth, the study of the change of pH of the materials was not conducted, whereas the effects of changes of pH of the materials must influence on their changes of the viscosity [16]. These studies also must be conducted in further investigations.
Conclusion
In this study, we prepared four types of blenderized diet to measure their viscosity and temperature for 30 minutes after preparation. These four types were as follows: (1) in Methods 1, 3, and 4, the viscosity of the experimental BDs increased over the 30 minutes consistent with the decrease in temperature of the material. (2) In Method 2, the viscosity of BDs at 30 minutes was significantly lower than that observed in Method 1. (3) Also in Method 2, unlike with the other three methods, viscosity decreased significantly during the 30 minutes. This phenomenon might be related to activation of the added amylase. (4) Viscosity during the 30-minute observation remained within the range of 3,500-10,000 mPa.s, which has been reported to be acceptable in clinical settings. (5) Finally, the freezing overnight and defrosting of BD in Method 4 appeared to maintain viscosity stable within the acceptable range likely in method 3. To our knowledge, this is the first study to evaluate the viscosity and temperature of a blenderized diet. These results might provide basic information for further evaluation of the more complicated blenderized diets used in clinical practice.References
- Pahsini K, Marinschek S, Kahn Z, Dunitz-Scheer M, Scheer PJ (2015) Unintended side-effects of enteral nutrition support: the parental perspective: A qualitative analysis. J Pediatr Gastroenterol Nutr [Epub ahead of print].
- Nishiwaki S, Araki H, Shirakami Y, Kawaguchi J, Kawade N, et al. (2009) Inhibition of gastroesophageal reflux by semi-solid nutrients in patients with percutaneous endoscopic gastrostomy. JPEN J Parenter Enteral Nutr 33: 513-519.
- Shimoyama Y, Kusano M, Kawamura O, Zai H, Kuribayashi S, et al. (2007) High-viscosity liquid meal accelerates gastric emptying. Neurogastroenterol Motil 19: 879-886.
- Simonian HP, Maurer AH, Knight LC, Kantor S, Kontos D, et al. (2004) Simultaneous assessment of gastric accommodation and emptying: studies with liquid and solid meals. J Nucl Med 45: 1155-1160.
- Johnson TW, Spurlock A, Galloway P (2013) Blenderized formula by gastrostomy tube: A case presentation and review of the literature. Top Clin Nutr 28: 84-92.
- Pentiuk S, O'Flaherty T, Santoro K, Willging P, Kaul A (2011) Pureed by gastrostomy tube diet improves gagging and retching in children with fundoplication. JPEN J Parenter Enteral Nutr 35: 375-379.
- O'Flaherty T, Santoro K, Pentiuk S (2011) Calculating and preparing a pureed by gastrostomy-tube (PBGT) diet for pediatric patients with retching and gagging postfundoplication. Child Obes Nutr 3: 361-364.
- Rosenfeld L (1997) Gastric tubes, meals, acid, and analysis: rise and decline. Clin Chem 43: 837-842.
- Minard G (2006) The history of surgically placed feeding tubes. Nutr Clin Pract 21: 626-633.
- Johnson TW, Spurlock A, Pierce L (2015) Survey study assessing attitudes and experiences of pediatric registered dietitians regarding blended food by gastrostomy tube feeding. Nutr Clin Pract 30: 402-405.
- Barbon CE, Steele CM (2015) Efficacy of thickened liquids for eliminating aspiration in head and neck cancer: a systematic review. Otolaryngol Head Neck Surg 152: 211-218.
- Leder SB, Judson BL, Sliwinski, Madson L (2013) Promoting safe swallowing when puree is swallowed without aspiration but thin liquid is aspirated: nectar is enough. Dysphagia 28: 58-62.
- (2012) Ministry of agriculture, forestry and fisheries, management guidelines for the prevention of rice mold contamination. 19.
- Ichimaru S, Amagai T, Wakita M, Shiro Y (2012) Which is more effective to prevent enteral nutrition-related complications, high-or medium-viscosity thickened enteral formula in patients with percutaneous endoscopic gastrostomy?: a single-center retrospective chart review. Nutr Clin Pract 27: 545-552.
- Wakita M, Masui H, Ichimaru S, Amagai T (2012) Determinant factors of the viscosity of enteral formulas: basic analysis of thickened enteral formulas. Nutr Clin Pract 27: 82-90.
- Ghorbani Gorji S, Ghorbani Gorji E, Mohammadifar MA (2015) Effect of pH on turbidity, size, viscosity and the shape of sodium caseinate aggregates with light scattering and rheometry. J Food Sci Technol 52: 1820-1824.