Journal of Cancer Sciences
Download PDF
Research Article
*Address for Correspondence: S. David Nathanson, MD, FRCS, FACS, Department of Surgery, Henry Ford Health System, 2799 W. Grand Boulevard, Detroit, MI 48202, USA, Tel: 313-916-2917; Fax: 313-916-8193; E-mail: dnathan1@hfhs.org
Citation: Shah R, Rosso KJ, Nathanson SD, Chitale D, Mahan M. The Association amongst ‘Triple Negative’ Breast Cancers, Lymph Node Metastasis, Disease Free and Overall Survival. J Cancer Sci. 2015;2(1): 5.
Copyright © 2015 Nathanson et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Cancer Sciences | ISSN: 2377-9292 | Volume: 2, Issue: 1
Submission: 12 January 2015 | Accepted: 11 February 2015 | Published: 14 February 2015
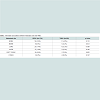
There was significantly more brain (p=0.012), lung (p<0.001), and soft tissue (p=0.002) metastases in the TNBC group as compared to the RPBC group (Table 2).
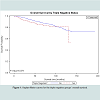
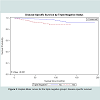
A logistic regression using TNBC status as the predictor of metastasis demonstrated that having triple negative disease increased the odds of metastasis by 2.15 times; however, the confidence interval included 1.0 and the p-value approached but did not reach statistical significance. Overall survival in patients with TNBC trended towards being worse (p=0.079) with a 2.71-fold increased risk of cancer death compared to RPBC. When analyzed separately, survival of these patients was lower in the first 8 years of diagnosis but was comparable thereafter (Figures 1 and 2).
The Association amongst ‘Triple Negative’ Breast Cancers, Lymph Node Metastasis, Disease Free and Overall Survival
Rupen Shah1, Kelly J. Rosso1, S. David Nathanson1*, Dhananjay Chitale2 and Meredith Mahan3
- 1Department of Surgery, Henry Ford Health System, Detroit, Michigan, USA
- 2Department of Pathology, Henry Ford Health System, Detroit, Michigan, USA
- 3Division of Biostatistics, Department of Public Health Sciences, Henry Ford Health System, Detroit, Michigan, USA
*Address for Correspondence: S. David Nathanson, MD, FRCS, FACS, Department of Surgery, Henry Ford Health System, 2799 W. Grand Boulevard, Detroit, MI 48202, USA, Tel: 313-916-2917; Fax: 313-916-8193; E-mail: dnathan1@hfhs.org
Citation: Shah R, Rosso KJ, Nathanson SD, Chitale D, Mahan M. The Association amongst ‘Triple Negative’ Breast Cancers, Lymph Node Metastasis, Disease Free and Overall Survival. J Cancer Sci. 2015;2(1): 5.
Copyright © 2015 Nathanson et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Cancer Sciences | ISSN: 2377-9292 | Volume: 2, Issue: 1
Submission: 12 January 2015 | Accepted: 11 February 2015 | Published: 14 February 2015
Abstract
‘Triple negative’ breast cancer (TNBC) has fewer specific targets for systemic therapy. We hypothesized that patients with TNBC have an increased incidence of sentinel lymph node (SLN) metastases and decreased disease-specific and overall survival.Method: Pertinent clinical, pathologic and follow-up data from all breast cancer patients undergoing SLN biopsy from 1995 through 2008 were prospectively accrued and retrospectively analyzed. Overall survival was determined by Kaplan-Meier and regression analysis with particular attention to TNBC compared to “receptor positive breast cancer” (RPBC) that expressed any of the three targets: ER, PR and/or Her-2/neu.
Results: 1,971 patients treated by standard loco-regional and systemic therapies were followed for 1 to 16.4 years. 230 (11.7%) patients had TNBC. Median and mean follow-up times for all patients were 54 and 59.7 months, respectively. There was no significant difference in the rate of SLN metastases between TNBC and RPBC (p=0.564). In the univariate analysis TNBC demonstrated a higher incidence of lymphovascular invasion (LVI) (p=0.016), larger tumor size (p<0.001), and higher grade (p<0.001). Age and tumor grade were significantly different in the multivariable model (p=0.009 and p<0.001, respectively). TNBC increased the odds of distant metastases by 2.15 fold; however this was not statistically significant (p=0.063). There was a 2.71-fold increased risk of cancer death in the TNBC group in the first 8 years after initial treatment. Overall survival tended to be worse but did not reach statistical significance (p=0.079).
Conclusion: Patients with TNBC had an increased mortality in the first eight years after treatment when compared to patients with RPBC. There was no difference in rates of SLN metastasis.
Keywords
Metastasis; Sentinel lymph nodes; Triple negative breast cancer; Overall survivalSynopsis
Triple negative breast cancer (TNBC) is an aggressive disease especially in young African-American women and has a higher mortality than other breast cancer subtypes. In our study, TNBC did not have a higher incidence of sentinel and non-sentinel axillary metastasis.Introduction
Breast cancer prognosis is most often dependent upon tumor size, grade, lymph node metastasis and distant metastasis. Triple negative breast cancers (TNBCs) account for about 15% of all invasive breast cancers, are usually larger and have a higher histologic grade than other breast cancer subtypes originating from ductal epithelium [1-5]. TNBCs more commonly metastasize to viscera, particularly to the lungs and brain, and are less likely to metastasize to bone [6,7]. The fact that TNBC slack specific target receptors for systemic therapymay account for worse outcomes compared to receptor positive breast cancer (RPBC) [6].Despite the increasing evidence that TNBC is a biologically unique breast cancer phenotype, little is known about its mechanism of metastasis to the regional lymph nodes (RLNs). It is understood that the likelihood of systemic metastases correlates directly with the presence of RLN metastasis [8]. Increased biological aggressiveness [9] and large primary tumor burden [8] lead to a higher incidence of SLN metastasis and could explain the increased rates of systemic metastasis and death in TNBC.
This study investigates the hypothesis that patients with TNBC have an increased incidence of SLN metastases and decreased disease free and overall survival when compared to RPBC.
Methods
Clinical, pathological and outcomes data for women undergoing SLN biopsy (SLNB) for breast cancer at Henry Ford Health System was gathered into a prospectively accrued and retrospectively analyzed database from 1995 to 2008. Implementation and maintenance of this database was supported by the Institutional Review Board. All patients in this study were diagnosed and managed by a multidisciplinary team of breast cancer physicians and ancillary staff in an integrated academic health system. Patients were offered operative SLNB by appropriately trained and credentialed surgeons as part of their breast cancer management and all patients with positive SLN were further managed by complete axillary lymph node dissection (CALND).At the time of inquiry, our database consisted of 1,971 patients. Median and mean follow-up times for all patients were 54 and 59.7 months, respectively. Patients were classified as TNBC if they were ER, PR, and HER2- negative; and tumors expressing ER, PR and/or Her-2 were considered RPBC.
The clinical data included: age, race, tumor size, stage, surgery performed, chemotherapy (yes or no), breast irradiation (yes or no), systemic metastasis (yes or no) and sites of metastasis. The pathologic data included: primary tumor size, stage, histology, grade, lymphovascular invasion (LVI), SLN metastasis (yes or no), size of the lymph node metastasis, extra capsular extension (ECE) and the number of nodes positive.
Follow-up clinical, imaging and laboratory studies were done at the discretion of the oncologist and the surgeon. The identification of new systemic and/or loco-regional metastases and the date of any death was documented and recorded in the database.
The data was analyzed to compare TNBC and RPBC. Those with statistical significance by univariate analysis were further analyzed by multivariate analysis. Disease-specific and overall survivals were determined using the Kaplan-Meier method. Statistical analysis was performed using SAS 9.2 (SAS Institute Inc., NC).
Results
Of the 1,971 patients in our database, 230 (11.7%) patients had TNBC and the remainder was identified as having RPBC. A total of 1,829 underwent SLNB and the remainder (7.2%) underwent a CALND if the SLN was not identified. Median and mean follow-up times for all patients were 54 and 59.7 months, respectively.TNBC was seen more commonly in younger (p<0.001) and African-American (p<0.001) patients (Table 1). TNBC had a higher incidence of ductal carcinoma (p<0.001), larger tumor size (p<0.001), higher incidence of LVI (p=0.016), a higher grade (p<0.001), higher stage and a greater proportion of systemic metastases in the univariate analysis. Age and tumor grade were significantly different in the multivariable model (p=0.009 and p<0.001, respectively). A significantly higher number of TNBC patients received systemic chemotherapy (p<0.001).There was no significant difference in the rate of SLN metastases between TNBC and RPBC (p=0.564). The number of malignant lymph nodes in the axilla in TNBC and RPBC were 5.1±7.1 and 3.7±4.8 (p=0.79) respectively. A subset analysis was done to examine if patients with positive SLNs and TNBC developed systemic metastases more often than patients with positive SLNs without triple-negative status. Of the 390 total patients with positive SLNs, 47 developed systemic metastases and 343 did not or their metastatic status was unknown.
Discussion
A comparison between TNBC and RPBC groups demonstrated that TNBC patients had a greater likelihood of dying from their disease or other co-morbid conditions in the first eight years after initial treatment and a higher likelihood of metastases to lungs, brain and soft tissues, but they did not have a higher likelihood of either SLN metastases, increased size of metastasis or increased rate of metastases to the non-sentinel axillary nodes. Patients with TNBC were younger at diagnosis and more likely to be African American than patients with RPBC. The pathological analysis of TNBC showed a significantly higher incidence of dedifferentiated tumors and a trend towards larger size and increased lymphovascular invasion.Standard clinical management of breast cancer relies on traditional prognostic factors including nodal status, tumor histological grade, primary tumor size, estrogen receptor, progesterone receptor, and HER-2/neu expression. Although recent advances in immunehistochemical and genetic techniques have led to a better understanding of TNBCs, these tumors remain a heterogeneous group with difficult to define subtypes [10-12]. Available data indicate that TNBCs benefit neither from hormonal therapies nor from treatments targeted against the HER-2/neu receptor [7,13,14]. TNBCs tend to be larger than other subtypes of breast cancer and are usually high grade invasive ductal carcinomas of no special type [1,5,15,16]. In our study, these tumors were seen more often in younger African American women, in line with other reports [4,17]. They were found to be larger in size, higher pathological grade and higher incidence of LVI, which could explain the aggressive nature and poorer outcome associated with this subtype.
Basal-like cancers, which are usually triple-negative, [18,19] are more likely than other subtypes to be node-negative [16,20-22]. We found no difference in the SLN positivity rate between TNBCs and RPBCs. Node positivity in patients undergoing SLN biopsy was consistently higher than in patients in whom CALND was the first procedure done to determine the status of the axillary nodes [23]. This finding can likely be attributed to the variation in sectioning and processing of these two respective specimen types [23-25].
The total tumor burden in the axilla might also be different in patients with TNBC if the receptor status was in some way involved in the mechanisms of loco regional spread [26]. The mechanism of lymph node metastasis is not yet fully understood [27] but a number of interacting molecular and mechanical factors have already been shown to play a major role. The absence of biochemically important molecules, such as estrogen, progesterone and Her-2/neu receptors, could be part of a larger aberration of active proteins and peptides involved in the initiation and progression of metastasis. The volume of tumor in the SLN was also examined in these two groups and neither the total number of lymph nodes with disease nor the size of the tumor within the SLN was found to be different.
TNBCs are more likely to metastasize to the lungs and brain, and less likely to metastasize to bone [1,6,7,17,28]. Our study observed a higher incidence of TNBC metastasis to the brain, lung and soft tissue.
Dent et al. studied the patterns of recurrence in 1601 women with breast cancer during a median follow-up of 8.1 years [1]. They found a distinct difference between the recurrence patterns of TNBC and other forms of breast cancer. This pattern was characterized by a higher number of breast cancer recurrences in the first 2 years after primary treatment, with a peak at 2-3 years after diagnosis. The risk of recurrence subsequently declined over the next 5 years. The majority of patients with TNBC who did not experience recurrence up to 8 years after treatment were less likely to experience a recurrence thereafter, whereas in other forms of breast cancer, the risk of recurrence increased as time progressed. The shape of the survival curve for TNBC patients differs from that for patients with other types of cancers: there is a decrease in survival during the first few years after diagnosis but is comparable to RPBC thereafter [1,5,6]. Our study also observed a decline in TNBC survival in the first 8 years, after which the two groups had similar survival curves.
Conclusion
In conclusion TNBCs were found in younger African American women, were of higher pathological grade, had a higher incidence of LVI and metastasized to the lung, brain and soft tissue at a higher rate than RPBC. The patterns, incidence and volume of axillary lymph node metastasis were no different in these two groups. When compared to RPBC, TNBC demonstrated an early aggressiveness and increased mortality in the first 8 years after diagnosis and treatment.References
- Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, et al. (2007) Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13: 4429-4434.
- Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, et al. (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A 98: 10869-10874.
- Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, et al. (2003) Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A 100: 8418-8423.
- Reis-Filho JS, Tutt AN (2008) Triple negative tumours: a critical review. Histopathology 52: 108-118.
- Tischkowitz M, Brunet JS, Begin LR, et al (2007) Use of immunohistochemical markers can refine prognosis in triple negative breast cancer. BMC Cancer 7: 134.
- Liedtke C, Mazouni C, Hess KR, André F, Tordai A, et al. (2008) Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol 26: 1275-1281.
- Dent R, Hanna WM, Trudeau M, Rawlinson E, Sun P, et al. (2009) Pattern of metastatic spread in triple-negative breast cancer. Breast Cancer Res Treat 115: 423-428.
- Nathanson SD, Kwon D, Kapke A, Alford SH, Chitale D (2009) The role of lymph node metastasis in the systemic dissemination of breast cancer. Ann Surg Oncol 16: 3396-3405.
- Fisher B, Wolmark N, Coyle J, Saffer E, Fisher ER (1975) Studies concerning the regional lymph node in cancer. VIII. Effect of two asynchronous tumor foci on lymph node cell cytotoxicity. Cancer 36: 521-527.
- Rakha EA, El-Sayed ME, Green AR, Lee AH, Robertson JF, et al. (2007) Prognostic markers in triple-negative breast cancer. Cancer 109: 25-32.
- Weigelt B, Baehner FL, Reis-Filho JS (2010) The contribution of gene expression profiling to breast cancer classification, prognostication and prediction: a retrospective of the last decade. J Pathol 220: 263-280.
- Metzger-Filho O, Tutt A, de Azambuja E, et al. (2012) Dissecting the heterogeneity of triple-negative breast cancer. J Clin Oncol 30: 1879-1887.
- Tan DS, Marchió C, Jones RL, Savage K, Smith IE, et al. (2008) Triple negative breast cancer: molecular profiling and prognostic impact in adjuvant anthracycline-treated patients. Breast Cancer Res Treat 111: 27-44.
- Amos KD, Adamo B, Anders CK (2012) Triple-negative breast cancer: an update on neoadjuvant clinical trials. Int J Breast Cancer 2012: 7.
- Colleoni M, Cole BF, Viale G, Regan MM, Price KN, et al. (2010) Classical cyclophosphamide, methotrexate, and fluorouracil chemotherapy is more effective in triple-negative, node-negative breast cancer: results from two randomized trials of adjuvant chemoendocrine therapy for node-negative breast cancer. J Clin Onco l28: 2966-2973.
- García Fernández A, Giménez N, Fraile M, González S, Chabrera C, et al. (2012) Survival and clinicopathological characteristics of breast cancer patient according to different tumour subtypes as determined by hormone receptor and Her2 immunohistochemistry. a single institution survey spanning 1998 to 2010. Breast 21: 366-373.
- Foulkes WD, Smith IE, Reis-Filho JS (2010) Triple-negative breast cancer. N Engl J Med 363: 1938-1948.
- Bertucci F, Finetti P, Cervera N, Esterni B, Hermitte F, et al. (2008) How basal are triple-negative breast cancers? Int J Cancer 123: 236-240.
- Diaz LK, Cryns VL, Symmans WF, Sneige N (2007) Triple negative breast carcinoma and the basal phenotype: from expression profiling to clinical practice. Adv Anat Pathol 14: 419-430.
- Cheang MC, Voduc D, Bajdik C, Leung S, McKinney S, et al. (2008) Basal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clin Cancer Res 14: 1368-1376.
- Ozbas S, Ozmen V, Igci A, Muslumanoglu M, Ozcinar B, et al. (2012) Predicting the likelihood of nonsentinel lymph node metastases in triple negative breast cancer patients with a positive sentinel lymph node: Turkish Federation of Breast Disease Associations protocol MF09-01. Clin Breast Cancer 12: 63-67.
- Liu ZB, Liu GY, Yang WT, Di GH, Lu JS, et al. (2008) Triple-negative breast cancer types exhibit a distinct poor clinical characteristic in lymph node-negative Chinese patients. Oncol Rep 20: 987-994.
- Giuliano AE, Dale PS, Turner RR, Morton DL, Evans SW, et al. (1995) Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg 222: 394-399.
- Fisher ER, Swamidoss S, Lee CH, Rockette H, Redmond C, et al. (1978) Detection and significance of occult axillary node metastases in patients with invasive breast cancer. Cancer 42: 2025-2031.
- Kingsley WB, Peters GN, Cheek JH (1985) What constitutes adequate study of axillary lymph nodes in breast cancer? Ann Surg 201: 311-314.
- Hernandez-Aya LF, Chavez-Macgregor M, Lei X, Meric-Bernstam F, Buchholz TA, et al. (2011) Nodal status and clinical outcomes in a large cohort of patients with triple-negative breast cancer. J Clin Onco 29: 2628-2634.
- Nathanson SD (2003) Insights into the mechanisms of lymph node metastasis. Cancer 98: 413-423.
- Xu Z, Schlesinger D, Toulmin S, Rich T, Sheehan J (2012) Impact of triple-negative phenotype on prognosis of patients with breast cancer brain metastases. Int J Radiat Oncol Biol Phys 84: 612-618.