Journal of Urology & Nephrology
Download PDF
Case Report
*Address for Correspondence: Naheed Ansari, Jacobi Medical Center, 1400 Pelham Parkway South, Bronx, NY 10461, USA, E-mail: aznahaal@aol.com
Citation: Yedla S, Burugu S, Jim B, Ansari N. Antifreeze is always not Ethylene Glycol. J Urol Nephrol. 2014;1(1): 3.
Copyright © 2014 Yedla S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Urology & Nephrology | ISSN 2380-0585 | Volume: 1, Issue: 1
Submission: 25 February 2014 | Accepted: 18 April 2014 | Published: 24 April 2014
Reviewed & Approved by:Dr. Phillip M. Pierorazio, Assistant Professor, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins Medical Institutions, Maryland, USA
Antifreeze is always not Ethylene Glycol
Siddhartha Yedla, Shivakanth Burugu, Belinda Jim and Naheed Ansari*
- Division of Nephrology/Department of Medicine, Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY, USA
*Address for Correspondence: Naheed Ansari, Jacobi Medical Center, 1400 Pelham Parkway South, Bronx, NY 10461, USA, E-mail: aznahaal@aol.com
Citation: Yedla S, Burugu S, Jim B, Ansari N. Antifreeze is always not Ethylene Glycol. J Urol Nephrol. 2014;1(1): 3.
Copyright © 2014 Yedla S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Urology & Nephrology | ISSN 2380-0585 | Volume: 1, Issue: 1
Submission: 25 February 2014 | Accepted: 18 April 2014 | Published: 24 April 2014
Reviewed & Approved by:Dr. Phillip M. Pierorazio, Assistant Professor, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins Medical Institutions, Maryland, USA
Abstract
We describe a case of methanol intoxication resulting from antifreeze ingestion. A 23 year old Hispanic male presented to emergency room with vomiting, abdominal pain and blurry vision 48 hours after ingestion of gas line antifreeze in a suicidal attempt. The physical examination was unremarkable on presentation. Initial laboratory data was significant for a severe anion gap metabolic acidosis with an elevated osmolal gap. Urine examination under microscope did not demonstrate any crystals. With concern for ethylene glycol or methanol intoxication, the patient received intravenous fomepizole and was started on hemodialysis. He received a total of two sessions of hemodialysis and completed the fomepizole treatment along with administration of folic acid, thiamine and pyridoxine with an improvement in the acidosis and osmolal gap. His toxicology screen revealed an elevated methanol level (72 mg/dl) with normal ethanol and ethylene glycol levels. As methanol, but not ethylene glycol poisoning, can cause injuries to the optic nerve and retina resulting in blindness, an ophthalmologic examination is critical and was normal in this patient. After correction of his intoxication, the patient was subsequently discharged to a psychiatric unit.We caution that all antifreeze is not ethylene glycol, depending on the type, it may be methanol. Thus, obtaining information on the type of antifreeze is an important part of history taking in suspected cases of toxic ingestions and to predict organ involvement as well as plan of treatment.Keywords
Methanol; Antifreeze; Ethylene glycol; Calcium oxalate crystals; Fomepizole; Thiamine; Pyridoxine; HemodialysisIntroduction
Antifreeze poisoning commonly manifests as ethylene glycol intoxication in the form of central nervous system depression, cardiopulmonary instability, renal failure and presence of calcium oxalate crystals in the urinary sediment. It can be fatal in severe cases without immediate treatment. We report a case of methanol intoxication as a result of antifreeze ingestion.Case Study
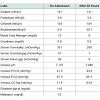
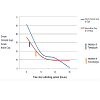
A 23 year old Hispanic male with a past medical history of severe depression presented to the emergency department (ED) with multiple episodes of vomiting, abdominal pain and blurry vision two days after ingestion of 700 ml of antifreeze along with anunknown quantity of beer. He denied headache, nausea, urinary symptoms, loss of consciousness or dizziness, but admitted to blurry and double vision. His social history was significant for severe depression for one year after the death of his young daughter. On arrival to the ED his vital signs showed a blood pressure of 151/100 mmHg, heart rate of 118 beats per minute, respiratory rate of 22 breaths per minute, temperature of 36.3°C, and a pulse oximetry of 98% on room air. His physical examination was unremarkable except for slowed speech and tachypnea.His laboratory findings demonstrated a serum sodium of 141 mEq/L, potassium of 4.8 mEq/L, chloride of 98 mEq/L, bicarbonate of 6.8 mEq/L, blood urea nitrogen of 15 mg/dL, and creatinine of 0.8 mg/dL (Table 1). His measured serum osmolality was 351 mOsm/kg. His anion gap and osmolal gaps were 36 mEq/l and 51 mOsm/kg respectively (Figure 1). Venous blood gas on room air showed a pH of 7.181, partial pressure of carbon dioxide (pCO2) of 21.5 mmHg, and partial pressure of oxygen (pO2) of 71.8 mmHg. On the day of admission, the serum ethanol concentration was < 10 mg/dl. Salicylate and acetaminophen levels were < 1 mg/dl and < 10 mg/l respectively. His urinalysis demonstrated a specific gravity of 1.030 with an unremarkable urine sediment under microscope.
Small Molecule Inhibitors of Hsp90
Given a compelling history of ingestion of a toxic alcohol, the patient was empirically initiated on intravenous (IV)-fomepizole therapy with a loading dose of 10 mg/kg along with oral folic acid, thiamine and pyridoxine in the ED. IV Fomepizole was continued every 12 hours for following 48 hours. The patient was then admitted to the intensive care unit. Emergent hemodialysis was initiated for possible ethylene glycol or methanol intoxication. After one session of hemodialysis, the patient’s serum anion gap and serum osmolal gap improved to 14 mEq/l and 17 mOsm/kg respectively. On second day of hemodialysis, his serum anion gap and serum osmolal gap were 9 mEq/l and 1 mOsm/kg respectively. His toxicology screen assay sent at time of admission revealed an ethylene glycol level of < 10 mg/dl (negative), but a methanol level of 72 mg/dl which returned on the third day of admission. Upon further questioning, patient admitted to taking specifically gas line anti-freeze. In suspicion of ocular toxicity, ophthalmology consult was obtained which showed normal fundoscopic examination.The patient was then transferred to psychiatry service for subsequent management of severe depression with suicidal ideation.
Discussion
Intoxication with methanol and ethylene glycol occurs not infrequently and may be lethal. Both of these alcohols are primarily metabolized in liver by the enzyme alcohol dehydrogenase (ADH) which results in the production of toxic metabolites. Methanol produces formic acid and formaldehyde while ethylene glycol produces oxalic acid, glycolate, glyoxylate. Accumulation of these metabolites contributes to development of anion gap acidosis with an osmolal gap and various clinical consequences. Even ingestion of limited amounts of these alcohols may be lethal [1]. The minimal lethal dose in adults is 1 g/kg for methanol and 1.5 g/kg for ethylene glycol, while a serum level of more than 20 mg/dl is considered to be toxic for both the alcohols. Formic acid, the product of methanol metabolism can lead to neurologic disturbances, injury to optical nerve and retina, resulting in visual difficulties [1-3]. Vision disturbances in methanol intoxication are due to destruction of mitochondria and microtubules in the optic nerve [4]. Toxic metabolites from ethylene glycol metabolism, particularly glycolic acid and oxalic acid are primarily responsible for metabolic acidosis and organ failure. Deposition of oxalate with calcium in brain, heart, kidney leads to neurological, cardiopulmonary and renal dysfunction [5,6].Ethylene glycol is a common constituent in automotive antifreeze, coolant liquid, cleansers and polishes while methanol is frequently used in gas line anti-freeze, gas cleaners and windshield wiper fluid. The source of anti-freeze should be an integral part of history taking in suspected poisoning cases to predict the possible alcohol intoxication, pertinent organ involvement, and plan of treatment.
The management of methanol and ethylene glycol intoxication involves two steps. The first step is the correction of metabolic acidosis by intravenous bicarbonate administration and the prevention of conversion of methanol and ethylene glycol to toxic metabolite by competitive inhibition of alcohol dehydrogenase by fomepizole. The second step involves the elimination of parent compound and its toxic acid metabolites by hemodialysis. Hemodialysis is the definitive treatment in most alcohol poisonings especially in patients who present with severe metabolic acidosis and acute kidney injury [6,7]. Methanol has a half-life of more than 50 hours which increases the need for hemodialysis in many patients to avoid adverse consequences like subarachnoid hemorrhage and blindness. Ethylene glycol has a much shorter half-life of less than 14 hours though the management of its intoxication is similar to that of methanol.
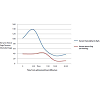
Methanol intoxication should be suspected strongly in patients with unexplained metabolic acidosis with an elevated anion gap and visual disturbances after ingestion of automotive or gas line antifreeze, or after consuming illicit liquors in habitual alcohol abusers. In such patients, consultation with a nephrologist should not be delayed until confirmatory methanol or ethylene glycol levels are available, which takes at least 2 days in most hospitals. Emergent hemodialysis along with Intravenous bicarbonate and supportive therapy can be lifesaving in methanol intoxication [8]. An ophthalmologic examination is crucial in suspected methanol ingestion and/or only in the first few days after the ingestion of parent alcohol. But as parent alcohols get metabolized, the serum osmolality will decrease and the serum anion gap will increase; the metabolites such as formate and glycolate will contribute to the unmeasured anions [9]. The anion gap will eventually fall when the metabolites undergo further metabolism [10,11] (Figure 2). As a result, the serum osmolal gap may not be a reliable clinical tool in patients with late presentations.
Conclusion
Antifreeze ingestion can manifest as either ethylene glycol or methanol intoxication. These intoxications can affect multiple organ systems. Anti-freeze is composed of either ethylene glycol or methanol. Ethylene glycol is a common ingredient in radiator antifreeze, coolant liquid, cleansers and polishes while methanol is commonly found in gas line anti-freeze, gas cleaners, windshield washer fluids and carburetor fluids. Physicians should inquire about the type of anti-freeze ingested upon admission from patient or family members to predict the appropriate intoxication and organ involvement. Conveniently, the treatment of both of these alcohols is similar, except for an ophthalmology evaluation for methanol intoxication.References
- Blanco M, Casado R, Vázquez F, Pumar JM (2006) CT and MR imaging findings in methanol intoxication. AJNR Am J Neuroradiol 27: 452-454.
- Jammalamadaka D, Raissi S (2010) Ethylene glycol, methanol and isopropyl alcohol intoxication. Am J Med Sci. 339: 276-281.
- Karayel F, Turan AA, Sav A, Pakis I, Akyildiz EU, et al. (2010) Methanol intoxication: pathological changes of central nervous system (17 cases). Am J Forensic Med Pathol 31: 34-36.
- Sharpe JA, Hostovsky M, Bilbao JM, Rewcastle NB (1982) Methanol optic neuropathy: a histopathological study. Neurology 32: 1093-1100.
- Eder AF, McGrath CM, Dowdy YG, Tomaszewski JE, Rosenberg FM, et al. (1998) Ethylene glycol poisoning: Toxicokinetic and analytical factors affecting laboratory diagnosis. Clin Chem 44: 168-177.
- Barceloux DG, Krenzelok EP, Olson K, Watson W (1999) American Academy of Clinical Toxicology practice guidelines on the treatment of ethylene glycol poisoning. Ad Hoc Committee. J Toxicol Clin Toxicol 37: 537-560.
- Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA, et al. (2002) American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol 40: 415-446.
- Kute VB, Godara SM, Shah PR, Gumber MR, Goplani KR, et al. (2012) Hemodialysis for methyl alcohol poisoning: a single-center experience. Saudi J Kidney Dis Transpl 23: 37-43.
- Coulter CV, Farquhar SE, McSherry CM, Isbister GK, Duffull SB (2011) Methanol and ethylene glycol acute poisonings – predictors of mortality. Clin Toxicol (Phila) 49: 900-906.
- Hovda KE, Hunderi OH, Rudberg N, Froyshov S, Jacobsen D (2004) Anion and osmolal gaps in the diagnosis of methanol poisoning: clinical study in 28 patients. Intensive Care Med 30: 1842-1846.
- Jacobsen D, Bredesen JE, Eide I, Ostborg J (1982) Anion and osmolal gaps in the diagnosis of methanol and ethylene glycol poisoning. Acta Med Scand 212: 17-20.
- Meatherall R, Krahn J (1990) Excess Serum Osmolality Gap after Ingestion of Methanol. Clin Chem 36: 2004-2007.