Journal of Surgery
Download PDF
Special Issue: Surgical Oncology
Case Report
*Address for Correspondence: Evan Ong, MD, MS, FACS, Department of Surgery, Swedish Medical Center, 1221 Madison St., Arnold Pavilion, Suite 1401 and 1411, Seattle, WA 98104, USA, Tel: 206-386-6700; Fax: 206-386-6706; E-mail: Evan.Ong@swedish.org
Citation: Rose J, Ong E. Irreversible Electroporation as a Treatment for Pancreatic Neuroendocrine Tumors. J Surgery. 2014; S(2): 5.
Copyright © 2014 Rose J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Special Issue: 2
Submission: 22 September 2014 | Accepted: 10 October 2014 | Published: 15 October 2014
Editors:Dr. Marlon A Guerrero, Assistant Professor of Surgery, University of Arizona, USADr. James A Warneke, Associate Professor of Surgery, University of Arizona, USA
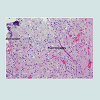
We followed this patient with routine CT scans and chromogranin-A levels. His lesion recurred on imaging (Figure 2) and with an elevated chromoganin-A level of 328. IRE had not completely destroyed the lesion, and it needed to be excised. At this point, he was amenable to an enucleation. 10 months after his initial surgery, we took him back to the operating room and performed a robotic assisted laparoscopic pancreatic enucleation with IRE for margin accentuation. We were able to excise the mass in its entirety. His pathology revealed a mixed serous cystadenoma with a well-differentiated neuroendocrine tumor (Figure 3). He had evidence of giant cells (Figure 4) and macrophages (Figure 5) consistent with apoptosis secondary to ablation of his initial lesion. To our knowledge, this is the first case report showing the pathologic findings of apoptosis in an operative specimen after treatment with IRE. He did well in the postoperative period and was discharged on post-operative day 4.
Irreversible Electroporation as a Treatment for Pancreatic Neuroendocrine Tumors
Jessica Rose1 and Evan Ong2*
- 1Department of Surgery, University of Arizona School of Medicine, Arizona, USA
- 2Department of Surgery, Swedish Medical Center, Seattle, WA, USA
*Address for Correspondence: Evan Ong, MD, MS, FACS, Department of Surgery, Swedish Medical Center, 1221 Madison St., Arnold Pavilion, Suite 1401 and 1411, Seattle, WA 98104, USA, Tel: 206-386-6700; Fax: 206-386-6706; E-mail: Evan.Ong@swedish.org
Citation: Rose J, Ong E. Irreversible Electroporation as a Treatment for Pancreatic Neuroendocrine Tumors. J Surgery. 2014; S(2): 5.
Copyright © 2014 Rose J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Special Issue: 2
Submission: 22 September 2014 | Accepted: 10 October 2014 | Published: 15 October 2014
Editors:Dr. Marlon A Guerrero, Assistant Professor of Surgery, University of Arizona, USADr. James A Warneke, Associate Professor of Surgery, University of Arizona, USA
Abstract
There is limited information using irreversible electroporation to treat pancreatic tumors. We report a case of a 78-year-old male who underwent irreversible electroporation of a pancreatic neuroendocrine tumor.Introduction
With a growing elderly population and an increase in the number of patients living with many co-morbidities, it is crucial to incorporate new technologies to advance the care of our patients. One area of interest is minimally invasive tumor ablation. Currently utilized techniques include chemical ablation, focused ultrasound ablation, interstitial laser coagulation, and radiofrequency ablation (RFA). Chemical ablation involves injecting a sclerosing agent (typically ethanol) into a tumor. However, it is difficult to control the treatment area because of chemical dissipation, local blood flow, and is limited by ethanol toxicity. Focused ultrasound uses high frequency ultrasound waves to heat and coagulate the tissue, while RFA uses an alternating current to coagulate tissues. Interstitial laser coagulation uses heat to denature proteins. All of these technologies can be introduced in a minimally invasive fashion to treat tumors, but it is very difficult to prevent the destruction of critical structures when heat is being used to destroy tissues at vital areas [1].A recent development in tissue ablation is irreversible electroporation (IRE). Electroporation uses electrical pulses to increase membrane permeability, using non-thermal high voltage direct electrical current to create a limitless number of nanopores in cell membranes. If this is done irreversibly, the cell membranes open up and cannot close, leading to cell death by apoptosis. Local blood flow does not affect the electric field and vital structures such as ducts and vessels are spared from thermal damage. IRE therefore allows the extent of tissue damage to be controlled. The probes for IRE can be used to treat tumors in a minimally invasive fashion [1-3]. Another advantage to IRE is the short treatment time; an average IRE session uses 90 pulses, each about 100 microseconds, taking less than a minute. When several treatment sessions are used, total treatment time is typically around 5 minutes, compared to other ablative techniques that use 15 to 60 minutes. An additional gain with IRE is the ability to control the treatment zone, which makes this technology usable near critical structures (blood vessels, bile ducts, ureter, pancreatic duct, etc.) [2,3]. This was initially tested in vivo in porcine models to be sure that IRE did not damage these vital structures [4].
The ability to control ablated margins is especially important when treating tumors of the pancreas. The pancreas is located near and contains several delicate structures: the portal vein, the superior mesenteric artery and vein, the common bile duct, and the pancreatic duct. One of the reasons pancreatic tumors have not been treated with ablation is that ablative methods have lead to tissue necrosis, pancreatic duct leak, and pancreatitis, which is not the case with IRE [5].
Our group envisions this technology to be applicable to all types of pancreatic tumors regardless of histological type. We report a case below in which we use IRE to accentuate margin control after robotic enucleation of a neuroendocrine tumor.
Case Report
Our patient is a functional 78-year-old gentleman with a past history of a pacemaker, atrial fibrillation requiring anticoagulation, hypercholesterolemia, hypertension, arthritis, and a prior cholecystectomy who presented to our clinic with an incidental finding of a 2.0 by 1.7 cm hypoechoic lesion on the body of the pancreas on CT scan (Figure 1). His initial imaging did not have IV contrast, and was a poor study to characterize the lesion, but his pacemaker precluded further imaging with an MRI. He underwent an endoscopic ultrasound with a fine needle aspiration and was found to have a neuroendocrine tumor. We discussed the possibility of either performing a laparoscopic distal pancreatectomy versus a laparoscopic enucleation of the lesion. The patient was adamant that he did not want any type of resection, as he did not want any alteration of his quality of life. Therefore, we offered him a laparoscopic irreversible electroporation (IRE) of his lesion. He underwent the procedure using the NanoKnife (AngioDynamics, Latham, NY) and recovered without complications.We followed this patient with routine CT scans and chromogranin-A levels. His lesion recurred on imaging (Figure 2) and with an elevated chromoganin-A level of 328. IRE had not completely destroyed the lesion, and it needed to be excised. At this point, he was amenable to an enucleation. 10 months after his initial surgery, we took him back to the operating room and performed a robotic assisted laparoscopic pancreatic enucleation with IRE for margin accentuation. We were able to excise the mass in its entirety. His pathology revealed a mixed serous cystadenoma with a well-differentiated neuroendocrine tumor (Figure 3). He had evidence of giant cells (Figure 4) and macrophages (Figure 5) consistent with apoptosis secondary to ablation of his initial lesion. To our knowledge, this is the first case report showing the pathologic findings of apoptosis in an operative specimen after treatment with IRE. He did well in the postoperative period and was discharged on post-operative day 4.
Discussion
Our patient was an elderly gentleman with multiple medical problems. He was unwilling to undergo a formal resection (distal pancreatectomy), as he did not want to risk the complications. Despite surgical advances, pancreatic resections are still complicated by a high morbidity (rates up to 45%) and mortality (<1%). Many perceive distal pancreatectomy to be less morbid than a pancreaticoduodenectomy, however, distal pancreatectomy can have leak rates around 25%, leading to both pancreatic fistulas and abscesses [6,7]. Another potential serious complication after distal pancreatectomy is insulin dependent diabetes, which happens to about 8% of patients in the immediate post operative period and can be as high as 46% within 2 years [7,8]. Although they occur less frequently, other complications of distal pancreatectomy include hemorrhage and death [7]. In contrast, enucleation preserves the majority of the pancreatic parenchyma, and avoids the risk of endocrine and exocrine dysfunction. Leak rates with this procedure depend on the size of the tumor and proximity of the tumor to the pancreatic duct. Considering the improved morbidity rates, enucleation is the preferred operation for benign tumors [9].Considering our patient’s medical history and his wishes, we wanted to be able to treat his tumor in a minimally invasive fashion. Despite the fact that his initial tumor was not fully ablated by IRE the first time, he still had a tumor with a fairly benign course. Pancreatic neuroendocrine tumors (PNETs) are much more readily resectable and have a much more favorable survival compare to other pancreatic tumors (about 60% five year survival). Because they have an indolent course, we felt that his tumor could effectively be treated with enucleation [10]. Since the initial treatment did not fully ablate his tumor, we felt that the best option was to use IRE to accentuate the margins after enucleation for better local control.
IRE is a technology using electricity to open the pores in cells to induce apoptosis, but unlike other ablative techniques, the operator is able to control the extent of ablation and preserve vital structures (the pancreatic duct in our patient) [1,2]. IRE was first tested in humans by Pech et al. and reported in 2010. They hypothesized that the technology would benefit patients with renal cell carcinoma. RFA has been used for this purpose, but there are reports of recurrences, ureteral stricture, and kidney loss. They performed IRE on 6 test patients, none of whom suffered complications as measured by laboratory or EKG changes. This was an early safety study, and the group suggested further study to determine histologic and long-term effects [11].
A group from Memorial Sloan Kettering thought that IRE would be ideal to treat those with hepatic lesions not amenable to RFA because they were located near major vascular structures. They treated 28 patients, with a total of 65 tumors. There were two complications: an intraoperative arrhythmia and a portal vein thrombosis, and no mortalities. One tumor had sustained disease and 3 had recurred in 6 months. This study showed early safety and efficacy of using IRE to treat perivascular liver tumors [12].
Considering the delicate nature of the pancreas, IRE is a useful technology to ablate lesions, without damage to the pancreatic duct or neighboring vasculature. A pilot study was conducted on 4 pigs by KP Charpentier and associates. They anesthetized 4 swine models and placed monopolar IRE electrodes 10-15 mm apart in the pancreas abutting the SMV and duodenum, as confirmed by ultrasound. Pulses of 100 volts per centimeter were delivered between electrodes in 100 microsecond pulses. 90 pulses were delivered per ablation in groups of 10, with 250 microsecond pauses in between groups. They measured pre-op, 2 day, and 5-day amylase, lipase, bilirubin, AST and ALT on their subjects. The pigs were euthanized for histologic evaluation at designated intervals. At 2 hours there was evidence of hemorrhage and necrosis. At 2 days there was well-demarcated ablation zones without damage to the ducts and vessels. At 2 weeks there was fibrosis in the ablation zones. None of the animals demonstrated clinical or laboratory evidence of pancreatitis, and since the duct remained intact there were no leaks. This animal pilot showed that this was a safe technology for use on pancreatic tissue [13].
Bower et al. also tested IRE in their swine lab. They anesthetized 6 pigs and performed ablations using both bipolar and monopolar electrodes within 1 mm of both the SMA and portal vein, which were located using ultrasound guidance. They delivered 90 pulses in groups of 10 (pulse duration 100 microseconds and interval of 250 microseconds). After the procedure daily lab studies were performed including assessment of liver function, amylase, lipase, cholesterol, complete blood count, blood urea nitrogen, and creatinine. Two pigs were euthanized at 3 days, 7 days, and 14 days post procedure. Overall, the pigs did well clinically. Histology on the specimens showed adequate ablation without damage to the vasculature. The pathology also confirmed that cell death was secondary to apoptosis, not necrosis. The results of the porcine model show that this technology is safe for use on pancreatic tissue [5].
Martin and colleagues utilized IRE in patients with locally advanced pancreatic adenocarcinoma. They performed a prospective multicenter study of IRE on patients with encasement of the celiac axis, SMA, or both. Patients either underwent surgical resection with IRE for margin accentuation or IRE alone. They obtained follow up imaging at 2 weeks and then at 3-month intervals to look for recurrence along with CA 19-9 levels. 27 patients were enrolled and treated, with 1 mortality and 3 other morbidities. There was no evidence of disease recurrence at 90 days. They conclude that it is a feasible modality for treatment and are planning to study the effects on long term and disease free survival [14].
Martin et al. also performed a prospective study of patients who underwent IRE for locally advanced pancreatic cancer in combination with chemotherapy and chemoradiation and compared them to a cohort of similar patients who underwent only chemotherapy and chemoradiation therapy during the same time period. They concluded that patients who underwent IRE in addition to standard therapy had better local palliation and improved overall survival [15].
Keane and colleagues performed an extensive literature review of ablative technology for the treatment of locally advanced pancreatic cancer. They felt that since few patients with pancreatic cancer are able to have curative resections and the response to chemotherapy is poor, new ablative technologies utilizing minimally invasive techniques and image guidance might be helpful to these patients. Early attempts at ablating pancreatic tumors were met with high morbidity and mortality. This group concluded that newer technologies or modifications to current technology were feasible and were able to cause ablation with decreased risks to the patient. Specific to IRE they described other studies showing that IRE was effective in ablating tumors (two patients underwent negative margin resections after IRE ablation) without compromising the peripancreatic vasculature or causing significant morbidity or mortality [16].
Despite these prior studies, we believe our case has the first pathologic evidence of ablation of a pancreatic neuroendocrine tumor with IRE. After treatment with IRE, cell death occurs by apoptosis and necrosis. On hematoxylin and eosin (H&E) stain there is an area of hemorrhage and necrosis at areas of treatment. Features of apoptosis can also be evident, this is demonstrated with calcification, macrophages, and giant cells on our own histologic specimens (Figures 3-5). Others have shown apoptosis by visualizing pyknosis and karyorrhexis or with BAX and TUNEL assays [2]. On H&E staining there is clear margination between treated and untreated zones, proving that you can control the zone of treatment [17]. Both the bile ducts and vessels remain intact on IRE treated specimens [13].
Conclusion
We believe that IRE is a safe method for ablation of pancreatic neuroendocrine tumors. It allows minimally invasive treatment, while keeping the pancreatic duct and vasculature intact.References
- Davalos RV, Mir IL, Rubinksy B (2005) Tissue ablation with irreversible electroporation. Ann Biomed Eng 33: 223-231.
- Lee EW, Thai S, Kee ST (2010) Irreversible electroporation: a novel image-guided cancer therapy. Gut Liver 4: S99-S104.
- Rubinsky B (2007) Irreversible electroporation in medicine. Technol Cancer Res Treat 6: 255-260.
- Lee EW, Loh CT, Kee ST (2007) Imaging guided percutaneous irreversible electroporation: ultrasound and immunohistological correlation. Technol Cancer Res Treat 6: 287-294.
- Bower M, Sherwood L, Li Y, Martin R (2011) Irreversible electroporation of the pancreas: definitive local therapy without systemic effects. J Surg Oncol 104: 22-28.
- Fahy BN, Frey CF, Ho HS, Beckett L, Bold RJ (2002) Morbidity, mortality, and technical factors of distal pancreatectomy. Am J Surg 183: 237-241.
- Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, et al. (1999) Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg 229: 693-698.
- Hutchins RR, Hart RS, Pacifico M, Bradley NJ, Williamson RC (2002) Long-term results of distal pancreatectomy for chronic pancreatitis in 90 patients. Ann Surg 236: 612-618.
- Crippa C, Bassi C, Salvia F, Falconi M, Butturini G, et al. (2007) Enucleation of pancreatic neoplasms. Br J Surg 94: 1254-1259.
- Bilimoria KY, Talamonti MS, Tomlinson JS, Stewart AK, Winchester DP, et al. (2008) Prognostic score predicting survival after resection of pancreatic neuroendocrine tumors: analysis of 3851 patients. Ann Surg 247: 490-500.
- Pech M, Janitzky A, Wendler JJ, Strang C, Blaschke S, et al. (2011) Irreversible electroporation of renal cell carcinoma: a first-in-man phase I clinical study. Cardiovasc Intervent Radiol 34: 132-138.
- Kingham TP, Karkar AM, D’Angelica MI, Allen PJ, DeMatteo RP, et al. (2012) Ablation of perivascular hepatic malignant tumors with irreversible electroporation. J Am Coll Surg 215: 379-387.
- Charpentier KP, Wolf F, Nobel L, Winn B, Resnick M, et al. (2010) Irreversible electroporation of the pancreas in swine: a pilot study. HPB (Oxford) 12: 348-351.
- Martin RC 2nd, McFarland K, Ellis S, Velanovich V (2012) Irreversible electroporation therapy in the management of locally advanced pancreatic adenocarcinoma. J Am Coll Surg 215: 361-369.
- Martin RC 2nd, McFarland K, Ellis S, Velanovich V (2013) Irreversible electroporation in locally advanced pancreatic cancer: potential improved overall survival. Ann Surg Oncol 20: S443-449.
- Keane MG, Bramis K, Pereira SP, Fusai GK (2014) Systematic review of novel ablative methods in locally advanced pancreatic cancer. World J Gastroenterol 20: 2267-2278.
- Edd JF, Horowitz L, Davalos RV, Mir LM, Rubinsky B (2006) In vivo results of a new focal tissue ablation technique: irreversible electroporation. IEEE Trans Biomed Eng 53: 1409-1415.