Journal of Surgery
Download PDF
Research Article
Anatomic Relationship between the Spinal Accessory Nerve and the Internal Jugular Vein in the Upper Neck during Neck Dissection: A Prospective Study
Rajan Govinda M1*, Bajarang PS1, Shyam TC1, Deepak P1, Sudeep M1, Paras RA1, Nimesh L2, and Durga N2
1Department of Otorhinolaryngology, B. P. Koirala Institute of Health Sciences, Dharan, Nepal.
2Department of Surgery, B. P. Koirala Institute of Health Sciences, Dharan, Nepal
2Department of Surgery, B. P. Koirala Institute of Health Sciences, Dharan, Nepal
*Address for Correspondence:Rajan Govinda Mulmi, Department of Otorhinolaryngology, B. P. Koirala Institute of Health Sciences, Dharan, Nepal. E-mail: rajan_mulmi@yahoo.com
Submission:21 December, 2023
Accepted:08 February, 2024
Published:12 February, 2024
Copyright:©2024 Rajan Govinda M, et al. Powell BS, et al. This is
an open-access article distributed under the Creative Commons Attribution
License, which permits unrestricted use, distribution, and reproduction in
any medium provided the original work is properly cited.
Keywords:Anatomy; Internal Jugular Vein; Spinal Accessory Nerve;
Anatomical Relationship; Prospective Study
Abstract
Objectives:To find the intraoperative relationship between the
spinal accessory nerve (SAN) and the internal jugular vein (IJV) in the
upper neck, at the level of the superior border of the posterior belly of
the digastric muscle.
Methods: A prospective study was carried out in the Department of Otorhinolaryngology and Head and Neck Surgery, B. P. Koirala Institute of Health Sciences, Dharan from December 2019 to November 2020.
Results:Thirty-nine patients were enrolled in the study who met the inclusion criteria. The mean age of the patient was 49.59 years with an SD of ±12.571 years. The age of the patients ranged from 17 to 70 years. The most common age group was 46 to 60 years (46.16%). The maximum number of patients were male which accounted for 32 (82.05%) and 7 (17.94%) were female. Unilateral neck dissections were done for 31 (79.48%) and bilateral neck dissections were done for 8 (20.51%) cases. The most common diagnosis for which neck dissections were carried out was carcinoma of the oral cavity (29 cases, 74.35%) followed by branchial cysts (4 cases, 10.25%), parotid neoplasms (4 cases, 10.25%) and thyroid neoplasms (2 cases, 5.12%).The SAN was positioned lateral to the IJV at the superior margin of the posterior belly of the digastric muscle in 35 (74.46%) of neck dissections, medial to the IJV at this level in nine cases (19.14%) and the SAN traveled directly through the IJV in three cases (6.38%).
Conclusion:The posterior belly of the digastric muscle is the most common location at which the SAN is encountered.
Methods: A prospective study was carried out in the Department of Otorhinolaryngology and Head and Neck Surgery, B. P. Koirala Institute of Health Sciences, Dharan from December 2019 to November 2020.
Results:Thirty-nine patients were enrolled in the study who met the inclusion criteria. The mean age of the patient was 49.59 years with an SD of ±12.571 years. The age of the patients ranged from 17 to 70 years. The most common age group was 46 to 60 years (46.16%). The maximum number of patients were male which accounted for 32 (82.05%) and 7 (17.94%) were female. Unilateral neck dissections were done for 31 (79.48%) and bilateral neck dissections were done for 8 (20.51%) cases. The most common diagnosis for which neck dissections were carried out was carcinoma of the oral cavity (29 cases, 74.35%) followed by branchial cysts (4 cases, 10.25%), parotid neoplasms (4 cases, 10.25%) and thyroid neoplasms (2 cases, 5.12%).The SAN was positioned lateral to the IJV at the superior margin of the posterior belly of the digastric muscle in 35 (74.46%) of neck dissections, medial to the IJV at this level in nine cases (19.14%) and the SAN traveled directly through the IJV in three cases (6.38%).
Conclusion:The posterior belly of the digastric muscle is the most common location at which the SAN is encountered.
Introduction
The spinal accessory nerve (SAN) is the eleventh cranial nerve.
The accessory nerve has two roots- a cranial part and a spinal part.
The cranial part arises from the nucleus ambiguous and also from
the dorsal nucleus of the vagus nerve. The cranial part leaves the
medulla oblongata as four or five rootlets which unite together and
then join the spinal part of the accessory nerve just as it enters the
jugular foramen (JF). It is only united with the spinal part for a short
course before uniting with the inferior ganglion of the vagus nerve.
So, these cranial fibers will then pass to the recurrent laryngeal and
pharyngeal branches of the vagus nerve, ultimately destined for the
muscles of the soft palate (except tensor veli palatini). [1] The spinal
roots arise from the spinal nucleus found in the ventral grey column
extending down to the first five cervical vertebral levels. These fibers
then emerge from the spinal cord and then ascend lateral to the spinal
cord through the foramen magnum posterior to the vertebral arteries.
Then it passes to the JF where it receives some fibers from the cranial
root. The SAN exits the JF with the ninth and tenth cranial nerves as
well as the internal jugular vein (IJV) [2-4].
It then courses inferiorly passing medial to the styloid process and
also found medial to the posterior belly of the digastric (PBD) muscle.
[1] The nerve travels for a distance of 3 to 4 cm on the levator scapulae,
then penetrates the deep surface of the sternocleidomastoid (SCM)
muscle. Branches are sent to the SCM muscle that it innervates. [5]
Ever since neck dissection (ND) was first described by George
Crile in 1906, [6-8] it has played an important role in the management
of metastatic nodal disease in head and neck cancer. [6] Radical
neck dissections (RND) involve the sacrifice of the SAN and result
in restricted shoulder abduction and postoperative pain. [9] This
shoulder morbidity has been a major impact on the movement
away from RND and towards functional neck dissections (FND).
FND was introduced with the preservation of IJV and/or SAN in
1963.[10] Modified radical neck dissections (MRND) and selective
neck dissections (SND) have emerged which intended to minimize
dysfunction by preserving the SAN without compromising oncologic
results. Moreover, an SND often aims to further reduce risk to the
SAN by avoiding a level V dissection altogether. [11-12] When
shoulder dysfunction occurs in the absence of a level V dissection, the
likely culprit is an injury at the level II region. [13] In a level II neck
dissection, the SAN is commonly identified initially at the anterior
border of the SCM. It is then skeletonized anterosuperiorly [14] and
followed deep to the PBD muscle, and it is here that injury most likely
can occur. The risk of injury may be minimized with a thorough
understanding of the SAN anatomy and its relationship with the IJV.
Specifically, the nerve can pass lateral (superficial) or medial (deep) to
the IJV, or it can pass directly through it.[11,15,16]
Thus, this variability between the SAN and the IJV is widely
accepted in the published literature and anatomy textbooks. [15,16]
Hence, the goal of the study was to intra operatively observe the
course of the SAN in relation to the IJV at the superior border of the
PBD muscle to determine its frequency at each of the three possible
positions.[11] These relations and positions are, however, not
observed in the Nepalese population. Knowledge of these variations
is important in locating the SAN and avoiding its inadvertent injury
during neck procedures such as node biopsies, SAN blocks, and
radical neck surgeries [17,18] to avoid the morbidity associated with
SAN injury. Therefore, the primary objective of the study is to find the
intraoperative relationship between the SAN and the IJV in the upper
neck, at the level of superior border of PBD muscle. The secondary
objectives were to observe the frequency of SAN passing lateral to
IJV, the frequency of SAN passing medial to IJV, and to observe the
frequency of SAN passing directly through IJV.
Materials and Methods
Study Population:
This is a prospective study enrolling patients from the Department
of Otorhinolaryngology-Head and Neck Surgery fulfilling the
inclusion criteria. The study duration was from December 2019 to
November 2020.The study population involved all the patients who underwent
unilateral or bilateral level II neck dissection for the treatment or
diagnosis of head and neck pathology and procedure where the
relationship between SAN and IJV could be assessed.
All the cases fulfilling the inclusion criteria were included in this
study. Non-probability convenient sampling was done and all the
consecutive samples were included.
The inclusion criteria included those patients undergoing
unilateral or bilateral level II neck dissection for head and neck
pathology and procedure where the relationship between SAN and
IJV could be assessed and those who consented to surgery. Neck
dissection not involving level II, patients undergoing revision surgery,
and intraoperative location of the SAN at the level of the digastrics
muscle which could not be ascertained were excluded.
Sample Size Estimation:
This Study Considers 95% Ci And 80% Power To Estimate
Sample Size. According To The Literature Review Taylor Et. Al [19,20],
It Was Found That Spinal Accessory Nerve Passed Through
Internal Jugular Vein In Only 2% Of Cases Which Is The Minimum
Prevalence.According To Previous Records Of The Medical Record Section, It
Was Found That Only 24 Cases Had Undergone Neck Dissections For
Head And Neck Pathologies In The Department Of Otolaryngology.
Therefore, The Final Sample Size Estimation Formula Was Used To
Estimate The Sample Size As Follows. (Cdc Atlanta Who Usa Epi Info
2007). The Sample Size Is 24, And A Total Of 24 Cases Were Enrolled
For This Study.
Ethical Clearance:
Ethical Clearance was obtained from the Institutional Review
Committee, B.P. Koirala Institute of Health Sciences.Study Method:
A prospective study was done where all the patients diagnosed
with Head and Neck pathology after history, general and systemic
examination, Ear Nose Throat (ENT), and Head and Neck
examination and confirmed via cytopathology and/or histopathology
report and undergoing unilateral or bilateral neck dissection were
included in this study.A cross-sectional method was done and the patient was allocated
to one of the following groups:SAN lateral(superficial/ventral) to IJV
(Group A), SAN medial(deep/dorsal) to IJV (Group B), and SAN
passing directly through IJV (Group C).
A subject enrollment form was filled and the eligible patient
was offered detailed printed information about the proposed study.
Patients agreeing to take part in the study were requested to sign the
consent form. After signing the consent, the patient was recruited
for the study.
Enrollment of Patients:
Patients without any discrimination of sex, race, religion,
and geography that fulfill the inclusion criteria mentioned above
were eligible for the clinical study. A prior informed written and
understood consent was taken from each patient after explaining in
detail the procedures, possible complications, and outcomes.A detailed clinical history, thorough general, physical, ENT, and
Head and Neck examinations were carried out and the findings were
recorded in the predesigned Proforma. Pre-operative investigations
along with a CT scan of the neck from the base of the skull to the
upper mediastinum were performed.
Steps of operation
Selective Neck Dissection:
Anesthesia, positioning, and draping:The operation was done
under general anesthesia. The patient was placed in a supine position
with the neck extended and the head turned to the opposite side.Operative steps:
The neck was opened via a horizontal incision placed in a skin
crease just below the level of the hyoid bone. The incision was
made through the skin, subcutaneous fat, and platysma muscle
and identified the external jugular vein and greater auricular nerve
overlying the SCM. Next, the superior skin flap was elevated with
cautery in a subplatysmal plane until the submandibular salivary
gland is identified. Electrocautery or a scalpel was used to raise an
inferiorly based subplatysmal flap, exposing anteriorly up to the
omohyoid and inferiorly, the lateral surface of the SCM almost to
the clavicle. Lymph nodes were resected from the submental triangle
(Level Ia) with electro-cautery up to the hyoid bone.Next Level Ib of the neck was addressed. The fascia (capsule)
overlying the submandibular gland was incised midway over the
gland and was dissected from the gland in a superior direction in a
subcapsular plane to avoid injury to the marginal mandibular nerve.
The marginal mandibular nerve crossed the facial artery and vein.
The facial artery and vein are identified by blunt dissection with a
fine hemostat. Next attention was directed to the fat and lymph nodes
tucked anteriorly between the anterior belly of the digastric and
mylohyoid muscle.
Facial vessels for facial lymph nodes were palpated; if present,
they were dissected free using fine hemostats, the care is taken not to
traumatize the marginal mandibular nerve. The facial artery and vein
were then ligated and divided close to the submandibular gland so as
not to injure the marginal mandibular nerve. This frees up the gland
superiorly, which can then be reflected away from the mandible.
The mylohyoid muscle was retracted anteriorly with a right-angled
retractor. The clearly defined interfascial dissection plane between
the deep aspect of the submandibular gland and the fascia covering
the XIIn is opened with finger dissection. The XIIn was visible in the
floor of the submandibular triangle. Inferior traction on the gland
brings the lingual nerve and the submandibular duct into view. The
submandibular duct was separated from the lingual nerve, ligated,
and divided. The submandibular ganglion, suspended from the
lingual nerve, was clamped, divided, and ligated.The facial artery
was divided and ligatedjust above the posterior belly of digastric. The
external jugular vein was retracted laterally with the SCM muscle
which allowed access to Levels IIa and IIb. The greater auricular nerve
was preserved.The fascia was divided along the lateral aspect of the
posterior belly of the digastric. The posterior belly of digastric was
exposed along its entire length where facial vein crossed.
The XIIn was identified below the greater cornu of the hyoid
bone anterior to where it crossed the external carotid artery. Carefully
dissected along the nerve in a posterior direction and divided all the
veins crossing the nerve to expose the full length of XIIn.
After the nerve had crossed posterior to the external carotid
artery, the SCM branch of the occipital artery was identified that
tethered the XIIn. Dividing this artery releases the XIIn. The nerve
then coursed vertically along the anterior surface of the IJV and hence
leads the surgeon directly to the IJV. Using dissecting scissors or a
hemostat to part the fatty tissue behind the IJV in Level II, the surgeon
next identified the XIn which may course lateral (commonly), medial
(uncommonly), or through (very rarely) the IJV. The upper part
of the SCM was retracted posteriorly to expose Level IIb. With a
hemostat, create a tunnel immediately posterior to the IJV down to
the prevertebral muscles.
The transverse process of the C1 vertebra was palpated
immediately posterior to the XIn and IJV and served as an additional
landmark for the position of these structures in difficult surgical
cases. In order to resect Level IIb, identify the XIn in Level IIb, and
atraumatically dissect it free from the surrounding fat with sharp and
blunt dissection up to where it enters the SCM
The occipital artery passed across to the top of Level IIb; its
branches were cauterized should they be severed while dissecting the
superior part of Level IIb.
To resect Levels II and III, extend the incision along the posterior
edge of the deep aspect of SCM inferiorly through the fatty tissue of
Level III in anterograde direction. The anterograde dissection was
continued with a scalpel or scissors until the ansa cervicalis, and the
carotid sheath containing the common and internal carotid arteries,
Xn and IJV were sequentially exposed. The carotid sheath was incised
along the full course of the vagus nerve, and the neck dissection
specimen was stripped off the IJV while dissecting inside the carotid
sheath. The fat and lymphatics around the anterior aspect of IJV
was continued stripping until the common carotid artery was again
reached. The tributaries of the IJV were divided and ligated with silk
ties.
The final stepwas to complete stripping the neck dissection
specimen off the infrahyoid strap muscles taking care not to injure
the XIIn and its accompanying veins superiorly, and to deliver the
neck dissection specimen. The neck was irrigated with warm water,
the anesthetist was asked to do a Valsalva maneuver so as to elicit
unsecured bleeding vessels and chyle leakage, and a 5mm suction
drain was inserted. The neck was closed in layers with continuous
vicryl to platysma and sutures/staples to the skin.
Postoperative care:
The drain was maintained on continuous suction e.g. low pressure
wall suction, until the drainage volume was <30ml /24hrs.Statistical Analysis:
Data were collected as per the proforma. Data editing and
entry were done on the same day to ensure consistency and quality
of data. The collected data were entered in the Microsoft Excel file.
Data were analyzed using SPSS (Statistical Package for the Social
Sciences) Version 20 for Windows Software. Descriptive statistics
and frequencies were determined for categorical and numerical
variables. Frequency, percentage, mean, and standard deviation were
calculated.Results
The study was carried out in the Department of
Otorhinolaryngology and Head and Neck surgery from December 1,
2019 to November 30, 2020, where fourty seven ND of 39 patients
were performed.
Demoghraphic distribution:
Total of 39 patients that met the inclusion criteria were included
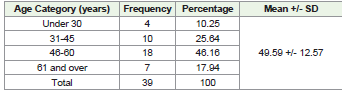
in this study.Age Distribution:
The mean age of patient was 49.59 years with SD of ±12.571 years.
The age of the patients ranged from 17 to 70 years. The most common
age group was 46 to 60 years (46.16%) followed by 31 to 45 years
(25.64%) as shown in [Table 1].Gender Distribution:
Among 39 patients, 32 (82.05%) were male and 7 (17.94%) were
female.Neck Dissections:
Total number of neck dissections carried out for different head
and neck pathologies among 39 patients were 47. Among thirty-nine
patients, unilateral neck dissections were done for 31 (79.48%) and
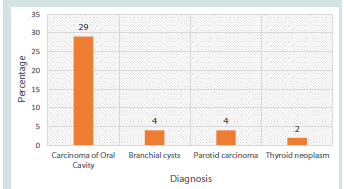
bilateral neck dissections were done for 8 (20.51%) of cases.Diagnosis of different pathologies:
Among thirty-nine neck dissections carried out for different head
and neck pathologies, majority of cases consisted of Neck Dissection
done for oncological diagnosis and treatment i.e. 29 cases (74.35%).
And, remainder of cases were neck dissection done for various other
surgeries including, 4 (10.25%) cases for branchial cysts, 4 (10.25%)
cases for parotid neoplasms and 2 (5.12%) cases for thyroid neoplasms
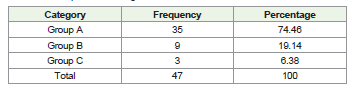
as shown in [Figure 1].Intraoperative Findings:
Most commonly the SAN was found positioned lateral to the IJV
at the superior margin of the posterior belly of digastric muscle in 35
(74.46%) of neck dissections and designated as Group A. The SAN
was positioned medial to the IJV at this level in nine cases (19.14%)
and designated as Group B, and the SAN travelled directly through
the IJV in three case (6.38%) and designated as Group C.It was found that there was only one variability between the sides
in the subjects who underwent a bilateral neck dissection, in which on
one side the SAN was lateral to the IJV and on the other side the SAN
was medial to the IJV.
Discussion
The SAN is the eleventh cranial nerve. It has a motor nerve
(somatic nerve) innervating two muscles – the SCM and trapezius.
It has two components – a spinal part and a cranial part. The cranial
part of accessory nerve is from the vagus nerve, but not all individuals
have a cranial root.[21] The spinal part arises from the first five or
six cervical spinal nerves. The spinal portion then ascends through
the foramen magnum passing laterally to join with the cranial root.
As the two nerves join, they then pass through the JF, along with the
glossopharyngeal and vagus nerves. The cranial part then passes to
the superior ganglion of the vagus nerve and distributed primarily in
the branches of the vagus. The spinal portion then goes on to supply
the SCM and trapezius in the neck. [1]
Richard W. Nason et. al performed an observational study “The
Anatomy of the Accessory Nerve and Cervical Lymph Node Biopsy”.
There should be detail knowledge of the courses of the nerve and its
anatomic relations in avoiding injury. Useful anatomical landmarks
were the proximal IJV in the anterior triangle and Erb’s point in the
posterior triangle. The transverse process of the atlas can be easily
palpated in the upper anterior triangle between the tip of the mastoid
and ramus of the mandible. The proximal IJV lies immediately
anterior to this point and is the key to identifying the proximal course
of the accessory nerve. The SAN runs from the foramen jugulare to the
border of trapezius. It is vulnerable to injury in surgical procedures
involving either the anterior the posterior cervical triangles. Injury to
the accessory nerve is reported to be the most frequent complication
of surgical procedures in the posterior triangle of the neck. [5,22]
Hinsley et. al did an observational cross-sectional study on
“Anatomic relationship between the Spinal Accessory Nerve and
Internal Jugular Vein in the upper neck” and found that out of 116
ND, 112(96%) were found lateral to IJV at the level of PBD muscle
and 3(3%) was positioned medial and 1(1%) travelled directly
through the IJV. A lateral position high in the neck creates increased
exposure of nerve in this area and can endanger it during level II ND.
Therefore, a complete understanding of Anatomy of SAN in upper
neck will potentially reduce the potential risk of iatrogenic injury of
the SAN and the IJV. [11]
According to the study “Intraoperative relationship of the spinal
accessory nerve to the internal jugular vein: Variation from cadaver
studies” done by Christine B. Taylor found out that out of 207 ND,
198(95.7%) were lateral/superficial to IJV at the level of upper border
of PBD muscle, 6(2.8) passed medial/deep, 2(0.9%) traversed through
the vein and 1(0.48%) divided travelling both lateral and medial to
the IJV. The anatomic course of the SAN remains area of debate
in cadaveric studies where the nerve passed medial to IJV more
frequently than laterally. The study concluded that this might be due
to intraoperative collapse of the IJV in cadaveric studies leading to
false identification of nerve medial to the IJV. Other possibility could
be that the nerves are often traced to the skull bases during cadaver
dissections, and the SAN exits the skull base in the JF medial to the
IJV. Thus this study has mentioned the location of SAN at the level of
PBD muscle. It is important to note that a minimal number of patients
will have aberrant anatomy and understanding such variation will
allow for safe preservation of the nerve.[19]
A case study done by Dhawan et. al on ‘A Rare anatomical
relationship of Spinal Accessory Nerve to Internal jugular vein’ noted
to have a unique relationship of SAN and IJV. At the upper ND (level
II), the SAN was observed to pass directly through the IJV. A patient
with squamous cell carcinoma (SCC) of right retromolar region of the
mandible and undergoing staging ND was noted to have this unique
relationship. Although most of the studies report a higher incidence
of lateral relation of SAN to IJV compared with medial relation, there
is a lot of variation in the incidence of lateral and medial relation in
different studies with a rare data of SAN emerging directly through
the IJV. A variable relation makes it prone to injury during level II
dissection with resultant morbidity. Therefore, one must be aware
and have knowledge of these anatomical variations to minimize this
risk of injury to the SAN and IJV. [23]
D. Levy et. al conducted a prospective study “Relations of the
accessory nerve with the internal jugular vein: surgical implications
in cervical lymph node clearances”. The study included 91 patients
operated for conservative cervical lymph node clearance between
December 1993 to October 1999. During the 91 surgical procedures
(123 nodal clearances), in 122 cases the nerve passed in front and
lateral to the IJV and in only one case the nerve passed medial and
the behind the IJV. So, when the nerve is lateral to the IJV it is usually
protected but, when it is medial and posterior to the IJV, it may be
damaged by the surgeon. [24]
N C. Ozturk et. al published a case report “Fenestration of Internal
jugular vein and relation to Spinal accessory nerve: Case report and
review of literature”. The study reported a unilateral fenestration of
the IJV on right side, and the SAN passed through the fenestrated
vein, pierced the carotid sheath, and then reached the SCM. Venous
fenestration is a rarely seen entity in the neck. Fenestrations and
complete divisions of the vasculature have been described in many
of the craniocervical arteries, but venous fenestrations are rarely
described. There was confusion between the terms: duplication and
fenestration in literature which are typically used interchangeably.
Such variations should be kept in mind during various surgical
dissections and radiological interventions in the neck. [25]
Suarez [8]introduced FND with the preservation of the IJV and/
or the SAN in 1963, following which various modifications to RND
have been proposed and demonstrated in several studies.[10]There
are many studies that describe the anatomical landmarks and their
variations to aid safe identification of the SAN, but majority of these
descriptions specially focus on the landmarks in the posterior triangle
of the neck.[15] There are relatively few literature that focuses on the
course of the nerve with relation to its surrounding structures in the
upper neck.[6] A complete understanding of the SAN anatomy in
the superior neck at the level of posterior belly of digastric muscle,
especially how it relates to the IJV, has been previously absent in the
Nepalese population.
After the establishment of ND procedures, in the management
of head and neck cancers, it has become important to know the
anatomical relationship between the SAN and the IJV in the upper
part of the neck because during almost every ND procedure, it is
always mandatory to remove level II lymph nodes for oncological
clearance.[23] Preservation of the SAN during ND and lymph node
biopsy is justifiable whenever possible to prevent shoulder disability.
[3] Iatrogenic injury to the SAN during ND may result in significant
and unavoidable morbidity if the form of shoulder syndrome which is
characterized by shoulder pain, restricted movement and drooping of
shoulder.[6,9,11,23] With the increasing use of SND, iatrogenic injury
to the SAN can be avoided, with a detailed knowledge of the anatomy
and the course of the SAN in the upper neck.[6] In our study, there
were total of 39 patients who underwent ND for various head and
neck pathologies. In doing so, we discovered a preponderance of the
lateral orientation of the SAN relative to the IJV.
Age:
The age of the patients ranged from 17 to 70 years. The mean age
of the patient was 49.59 years with an SD of 12.571 years. The most
common age group that underwent surgery was 46 to 60 years. These
findings are comparable to the study by Yigit et. al where age range of
patients was 18 to 50 years, and the mean age was 38.5 years.[26] But
the findings were different from the studies done by Hone et. al, Lee
et. al and Taylor et. al where mean age were 65.5 years, 31.7 years and
63.4 years respectively, which were relatively higher.[6,7,19]Gender:
Among 39 patients who underwent neck dissections, 32 (82.05%)
were male and 7 (17.94%) were female. Among 39 patients, 29
(74.35%) were male and 10 (25.64) were female in a study conducted
by Yigit et. al.[26] But, a study conducted by Saman et. al also had
female predominance with 55.73% female and 44.26% male among
61 patients.[27]Neck Dissections:
In our study, the total number of neck dissections done for 39
patients were 47, among which 31(79.48%) were unilateral and
8(20.51%) were bilateral. Our study showed similarity with the study
done by Dailiana et. al in which unilateral ND was performed in
17(85%) and bilateral ND was performed in 3(15%) of total 20 patients
that underwent ND.[28] Similarly, in a study done by Hinsley et. al
and Soo et. al which included 86 patients and 23 patients, 56(65.11%)
and 14(60.86%) had Unilateral ND and 30(34.48%) and 9(39.13%)
had bilateral ND respectively.[11,29] But in the contrary, in a study
done by Yigit et. al, 31(79.48%) had bilateral ND and 8(20.51%) had
unilateral ND of total 39 patients.[26]Diagnosis of different pathologies:
Our study included forty-seven ND done for different head
and neck pathologies. These included 29(74.35%) cases done for
oncological diagnosis and treatment, 4(10.25%) cases for branchial
cyst where ND was not done but just relationship of the SAN and
IJV was studied, 4(10.25%) cases for parotid carcinoma and 2(5.12%)
cases for thyroid neoplasm. There was a similar study done by
Nilakantan et. al in 2006, in which ND was done for primaries from
different sites including oral cavity 12(44.44%), oropharynx 2(7.4%),
hypopharynx 4(14.8%), larynx 6(22.22%) and unknown primary
3(11.11%) respectively.[30] Another study done by Taylor et. al had
127 ND done for different cases including oncological treatment
153(70.50%), branchial cyst 10(4.6%), carotid body tumors 5(2.3%),
vagal paragangliomas 2(0.9%) and high carotid artery exposure
2(0.9%).[19]Intraoperative Findings:
In our study, we tried to locate the position of the SAN higher up in
the neck at the level of posterior belly of the digastric muscle. In doing
so we found the predominant lateral location of the SAN relative to
the IJV. The SAN was located lateral to the IJV at the superior margin
of posterior belly of the digastric muscle in 35(74.46%) of ND, medial
to the IJV at this level in 9(19.14%) and the SAN traveled through the
IJV in 3(6.38%) of the cases in a total of 47 ND.In a similar study done by Hinsley et. al, the SAN travelled lateral
to the IJV in 112(96%) of ND, medial to the IJV in 3(3%) and travelled
directly through the IJV in 1(1%) of the total 116 live ND.11 Likewise,
Taylor et. al performed 207 live ND in which, the SAN was positioned
lateral to the IJV in 198(95.7%), medial to the IJV in 6(2.8%), and
directly through the IJV in 2(0.9%) of the cases.[19] In another study
done by Levy et. al in 2001 in which he performed 123 live ND for
nodal clearance, there was overwhelming preponderance of the SAN
lateral to the IJV in 122(99.2%) of the cases.[24]
There are also several cadaveric NDs done to find out the position
of the SAN. In a study done by Krause et. Al, [31] in which he
dissected 94 cadaveric necks and found out that the SAN was located
lateral to the IJV in 72.5% and medial to the IJV in 26.4% of the cases.
Saman et. al conducted 84 cadaveric ND and found that the SAN was
located lateral to the IJV in 80%, medial, and passed through the IJV
in 1% cases respectively.[27]
There are other several cadaveric ND, which pointed out the
medial predominance of the SAN in relation to the IJV. In a study
conducted by Kierner et. al, the SAN passed ventrally to the IJV in
24(56%) and dorsally to the IJV in 19(44%) of cases of total 43 ND.[15]
Another study in 32 cadavers by Soo et. al, where the SAN travelled
lateral to the IJV in 18(56%) and medial to the IJV in 14(44%).[29]
Similarly, Lee et. al and Amuti et. al conducted a study in 181 and 80
ND, where the SAN was located medial to the IJV in 104(57.4%) and
68(85%), and lateral to the IJV in 72(39.8%) and 12(15%) of the cases
respectively.[6,17]
Few previous studies have reported on the incidence of the SAN
passing through the fenestrated IJV. Hollinshead reported identifying
3.2% during cadaver dissection, Prades et. al reported 4(0.4%) cases of
this anomaly per 1000 ND and Lee et. al encountered this anomaly in
5(2.8%) cases during 181 ND. Hashimoto et al reported this clinical
incidence was 4 (2.1%) per 192 unilateral ND. [10] In our study, the
incidence of the SAN passing through the IJV was 1(3.22%) per 31
ND.
To summarize, there are similarities as well as discrepancies
between our study to other studies. We have mentioned that the
lateral orientation of the SAN is far more common than the medial
orientation. These variations may be due to several factors. Levy et.
al reported the intraoperative collapse of the IJV leading to the false
identification of the SAN medial to the IJV.[24] This finding might
explain the higher incidence of the medial course of the SAN relative
to the IJV in cadaveric studies due to the partial collapse of the IJV.
Also, as our study documented the SAN higher up in the neck, at
the level of superior border of posterior belly of the digastric muscle,
this may account for the differences with other intraoperative ND
studies that may have identified the nerve lower in the neck before it
had crossed over the vein. It should also be noted that the SAN exits
the skull base in the jugular foramen medial to the IJV. So during
cadaveric NDs, the nerve is often traced to the skull base. For these
reasons, the nerve might have been reported to be medial to the IJV
in cadaveric NDs. Surgeons should be careful during routine neck
explorations, as the SAN is likely to be encountered lateral to the IJV
at the level of the posterior belly of digastric muscle.[19] Thus, to
prevent injury to the SAN and the IJV, the surgeons should be clear
about the relation between the nerve and the vein and the level at
which the nerve is being identified.
Conclusion
The posterior belly of the digastric muscle is the most common
location at which the SAN is encountered. The vast majority of the
SANs coursed lateral to the IJV at the level of the posterior belly
of the digastric muscle. Thus, from this information and thorough
knowledge of the SAN anatomy and its intimate and variable
relationship with the IJV, surgeons will be able to minimize the
potential risk of injuring both of these structures during neck
dissections. Given the morbidities associated with iatrogenic injury
to the SAN, surgeons should also be aware of the rare relationship
between these structures.
Ethical Clearance:
Ethical Clearance was obtained from the Institutional Review
Committee, B.P. Koirala Institute of Health Sciences.Availability of Data and Materials:All relevant data are within
the manuscript.
Competing Interests:The authors have declared that no
competing interests exist.
Financial Disclosure:The authors received no specific funding
for this work.
Acknowledgements:None
Acknowledgements:None
Authors Contribution:
Rajan Govinda Mulmi, Bajarang Prasad Sah, Shyam Thapa
Chhetri, Deepak Paudel, Sudeep Mishra, Paras Raj Amatya, Durga
Neupane, Nimesh Lageju: Conception, design of the study, and
acquisition of data. Rajan Govinda Mulmi, Durga Neupane, Nimesh
Lageju: analysis and interpretation of data. Rajan Govinda Mulmi:
drafting the article. Rajan Govinda Mulmi, Durga Neupane, Nimesh
Lageju: revising the article. All authors contributed to the final
approval of the version to be submitted.