Journal of Surgery
Download PDF
Research Article
Recurrence after Resection: Pilot Study Post Ovarian Sparing Cystectomy for Benign Mature Ovarian Teratomas in Pediatrics
Snyder KB1*, Stewart RA2, Moon L3, Yu Z4, and Hunter CJ1
1Department of Pediatric Surgery, the University of Oklahoma, 800
Research Parkway, Oklahoma City, USA.
2College of Medicine, The University of Oklahoma, 800 Stanton L Young Blvd, Oklahoma City, USA.
3Department of Obstetrics and Gynecology, The University of Oklahoma, 800 Research Parkway, Oklahoma City, USA.
4Department of Pediatric Pathology, The University of Oklahoma, 800 Research Parkway, Oklahoma City, USA
2College of Medicine, The University of Oklahoma, 800 Stanton L Young Blvd, Oklahoma City, USA.
3Department of Obstetrics and Gynecology, The University of Oklahoma, 800 Research Parkway, Oklahoma City, USA.
4Department of Pediatric Pathology, The University of Oklahoma, 800 Research Parkway, Oklahoma City, USA
*Address for Correspondence: Katherine Brooke Snyder, Department of Pediatric Surgery, the
University of Oklahoma, 800 Research Parkway, Oklahoma City, USA E-mail Id: katherine-snyder@ouhsc.edu
Submission: 08 January 2024
Accepted: 05 February 2024
Published: 09 February 2024
Copyright: © 2024 Snyder KB, et al. Powell BS, et al. This is an open
access article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any
medium provided the original work is properly cited.
Abstract
Ovarian teratomas are relatively rare in children with the most
common ovarian tumor being a benign mature teratoma. There is
a significant knowledge gap regarding appropriate follow up after
ovarian sparing operation for monitoring for recurrence. Our study
aimed to delineate current follow up practices at our institution and
to evaluate recurrence rates under these guidelines to better develop
consistent follow up intervals for this patient population. A retrospective
chart review was conducted on all patients age 17 and younger who
presented for benign mature ovarian teratomas to assess follow up
practices and recurrence rates at our institution. This will serve as a
pilot study towards establishing standardized guidelines for this patient
population.
Introduction
Ovarian masses are relatively rare in children, with approximately,
2.4-2.6/100,000 cases per year with about malignant ovarian tumors
only compromising 1% of all childhood cancers [1,2]. The most
common ovarian tumor is a benign mature teratoma, which comprises
over 50% of all ovarian neoplasms [1,3,4]. In addition to being
benign, these tumors are typically slow growing, so if asymptomatic
they are generally treated expectantly [3]. However, many patients
present with symptoms such as abdominal pain, nausea, vomiting,
or even a palpable mass [3]. Surgical treatment is generally required
if the patient becomes symptomatic, it is greater than 5cm, or the
growth rate is greater than 2cm per year as these findings increase the
possibility of torsion [3]. Until recently, surgical treatment for ovarian
teratomas involved an oophorectomy, however, currently, surgical
management in children and adolescents involves ovarian sparing
cystectomy via laparoscopy or laparotomy [5]. The use of ovarian
sparing surgery is supported by literature supporting the importance
of preserving fertility and evidence that for benign ovarian masses
the risk of ipsilateral recurrence is lower than the risk of contralateral
metachronous malignancy [1]. However, literature on the recurrence
rate of these teratomas is lacking; there are some studies showing a
recurrence rate of 10% within one-year post operation [6]. With the
increase in ovarian sparing operations, there is now a heightened
concern for possible recurrence on both ipsilateral and contralateral
ovaries. Regardless of this, the current recommendation is to consider
ovarian sparing surgery in localized mature ovarian teratomas
meeting criteria of no evidence of lymphadenopathy, no metastasis,
normal levels of tumor markers, and absence of calcifications
on radiological findings [1]. A follow up strategy has not yet been
standardized for this particular procedure given that the recurrence
rate is not well established. Our study aims to evaluate recurrence and
follow up after ovarian sparing cystectomies to create a standardized
follow up interval.
Methods
A retrospective chart review was conducted on all patients age
17 and younger who presented for benign mature ovarian teratomas
that underwent resection. Data was collected between July 2012 to
July 2022 utilizing pathology findings post operatively on all patients.
Extensive chart review was performed reviewing radiologic findings,
operative findings, and final pathology results. Patients were excluded
from the study if the final pathology did not reveal a benign mature
teratoma or if a complete or partial oophorectomy was performed.
Following this, clinic follow up intervals that were offered were
evaluated through chart review. Any recurrence rates were noted.
Results
A total of 50 patients were evaluated after undergoing an operation
for an ovarian mass. After exclusion criteria, 36 patients met criteria
for analysis. Of the 36 patients that underwent an operation, 12 of
these patient’s pathology returned as benign mature teratoma after an
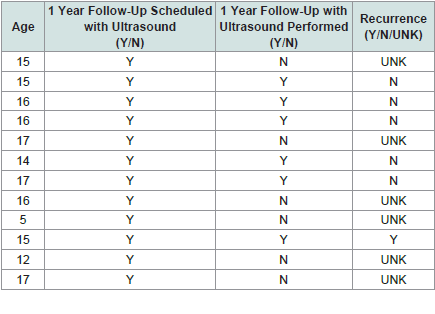
ovarian sparing cystectomy [Table 1] .
Table 1: Age and follow-up schedule with performance of ultrasound and follow
up appointment showing recurrence rates.
Patients ranged from age 5-17, with the average age being 14.5
years of age. All patients were offered one-month post-operative
follow up and one year follow up with an ultrasound performed at
one year. Six out of 12 patients did not show up for their one-year
ultrasound follow-ups. One patient returned for her one year follow
up and was found to have recurrence of bilateral ovarian cysts on
ultrasound. She underwent laparoscopic bilateral cystectomy and was
confirmed to have recurrence of benign mature teratomas.
Discussion
This retrospective cohort study provides pilot data from pediatric
and adolescent patients on recurrence rates and follow-up practices
upon undergoing ovarian-sparing surgery for benign mature ovarian
teratomas. 12 of the 36 patients (33%) who underwent an ovariansparing
cystectomy in this study had final pathology demonstrating
benign mature teratoma. There is one known recurrence out of the
12 patients (8%).
Only half of the patients (6 out of 12) returned for the one-year
ultrasound follow-up. Given that even a single recurrence detected
(which happened to be 17% of those that continued with the one-year
follow-up) via ultrasound occurred among this new cohort, it is
critical to maintain close surveillance in the first year after surgery to
monitor for recurrence. It might prove valuable to conduct further,
larger-scale and multi-institutional studies to better understand
and ascertain recurrence rates for benign mature ovarian teratomas
and ideal surveillance protocols after an ovarian-sparing teratoma
resection. Our study does provide support for a one-year followup
with ultrasound to check for both ipsilateral and contralateral
recurrences. Even so, long-term data on later recurrences is lacking.
A standardized follow-up interval has yet to be studied in this
population, with studies citing less than one year follow up and other
studies citing over 4.5 years follow up on average [6,7].
Given the retrospective nature of our study done at one institution,
there are limitations. Primarily, our sample size was small, making
statistical power a difficult feat. The follow-up was inconsistent given
that only half of the patients continued with the recommended
monitoring protocols. Additional studies, potentially at multiple
institutions, including data on the clinical characteristics of the
teratomas, the surgical treatments and approaches implemented,
and the health and genetic backgrounds of the patient population
will provide more valuable insight on possible additional and
confounding variables involved in the occurrence, recurrence, and
treatment of benign mature ovarian teratomas and will likely provide
more accurate and appropriate monitoring protocols.
Conclusion
In conclusion, our study provides pilot data that supports a one-year
ultrasound follow-up for patients with benign mature ovarian
teratomas that undergo ovarian-sparing surgery. Although not
perfect, such surgery has proven to be an appropriate approach for
the removal of these teratomas to attempt to preserve ovarian tissue
and fertility potential in young patients. Well-established longerterm
monitoring protocols have yet to be examined in greater depth.
Larger prospective multicenter analyses are required to establish
more accurate recurrence rates and subsequently more standardized
monitoring protocols following resection of benign mature ovarian
teratomas