Journal of Surgery
Download PDF
Commentary
Some Aspects of the Surgical and Endoscopic Treatment of Tuberculosis in Russia
Jargin SV*
Department of Pathology, People’s Friendship University of Russia,
Russian Federation, Russia
*Address for Correspondence:Jargin SV, Department of Pathology, People’s Friendship University of
Russia, Clementovski per 6-82, 115184 Moscow, Russia, Tel: 7 495
9516788; Email: sjargin@mail.ru
Submission: 20-03-2021;
Accepted: 22-04-2021;
Published: 26-04-2021
Copyright: © 2021 Jargin SV. This is an open access article distributed
under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided
the original work is properly cited.
Abstract
After the introduction of efficient drug therapy, the surgical
treatment of tuberculosis (Tb) has been partly abandoned in many
parts of the world. The priority of Russia in the field of Tb surgery was
pointed out. An overview of literature on the surgical treatment and
bronchoscopy in Tb is provided here. Despite the lack of reliable
clinical trial data on efficacy and safety of adjunctive surgical therapy,
some countries of the former Soviet Union continue to perform
numerous lung resections. Tuberculoma has been one of the most
frequent indications for lung surgery in Tb patients, which is generally
at variance with the international practice. Besides, the use of
bronchoscopy in Tb is briefly overviewed. In conclusion, some papers
containing questionable recommendations have remained without
due commentaries, so that a persistence of suboptimal practices or
reversion to them is not excluded.
Keywords
Tuberculosis; Surgery; Lung resection; Bronchoscopy; Russia
Introduction
After the introduction of efficient drug therapy in the 1950-1960s,
the surgical treatment of tuberculosis (Tb) has been partly abandoned
in many parts of the world. The role of surgery remains controversial
[1,2]. The priority of Russia in the field of Tb surgery was pointed
out [3,4]. This achievement has been largely associated with the name
of Mikhail Perelman. In 1998 he became director of the Institute for
Phthisiopulmonology at the I.M. Sechenov Moscow Medical Academy
and chief phthisiologist of the Health Ministry; in the following year
he became editor in chief of Tuberk. Bolezn. Legk. (Tuberculosis
and Lung Diseases), the leading Russian specialist journal. It was
the time when World Health Organization (WHO) promoted the
directly observed treatment, short course (DOTS) program in Russia.
Perelman called this WHO program absurd, insisting that Tb should
be treated surgically [5].
Materials and Methods
This article is a commentary based on the mini-review
predominantly of Russian-language professional literature that is
insufficiently known and partly unavailable outside the former Soviet
Union (SU). Where necessary, comparisons with the foreign literature
are made. The search of international literature was performed using
PubMed. Russian-language professional publications were searched in
the Internet and the electronic database eLibrary.Ru. Apart from the
analysis of literature, this commentary is based on the observations
by the author, who entered the I.M. Sechenov Medical University
(named Institute at that time) in 1973, later practiced at the same and
other academic and clinical institutions in Moscow.
Results
From 1973 through 1987, 285,000 patients with pulmonary
Tb were operated on in the former Soviet Union (SU), in 1987 – 26,000, while 85% of the operations were lung resections [6]. In
the period 1986-1988, 17,000-18,000 operations for pulmonary Tb
were performed in Russia yearly only in specialized tuberculosis
hospitals [3]. In 2003, 10,479 surgeries were performed in Russia for
respiratory Tb, which was deemed “extremely insufficient” [7]. In
2006, 12,286 operations were carried out for pulmonary Tb including
9300 (75.7%) lobectomies and other resections as well as 399 (3.2%)
pneumonectomies [4]. According to another report, the forms of
Tb most frequently treated by resections and pneumonectomies
were cavitary Tb (52.2%) and tuberculoma (43.9%) [8].The abovenamed
surgeries were performed and recommended also for patients
with inactive post-tuberculous fibrosis including cases with sparse
symptoms [9]. At the same time, surgeries were performed in the active
phase of Tb. In some provinces (Kemerovo, Chelyabinsk, Mordovia),
25-40% of patients with destructive Tb were operated on [10]. At the
time of initial Tb diagnosis, an operation was deemed reasonable in 15-
20% of patients [3]. According to another paper by the same authors,
indications for surgery were found in 20-30% of patients at the initial
diagnosis and/or among cases of active Tb [11].In Yekaterinburg
and surrounding province (2006-2008), indications for surgery were
determined in 1784 from 4402 (40.5%) patients with pulmonary
Tb while 1079 (24.5%) were operated on. Among reasons of the
comparatively “low” surgery rate were the patients’ non-compliance
and unavailability [12]. In the international literature, corresponding
figures are generally lower e.g. <5% of pulmonary Tb patients were
supposed to require surgery [13]. The same percentage is given in the
reviews [14,15]. The topic of Tb surgery may become more relevant
due to the multidrug resistance. According to a current estimate from
Russia, the need for surgery has increased from 5% to 15% over the
last twenty years [16]. However, the recent systematic review and
metaanalysis concluded that, compared with chemotherapy alone, the
survival benefit of pulmonary resection combined with chemotherapy
is not significant, although the quality of data was deemed “relatively
poor” [17]. According to another metaanalysis, partial lung resection,
but not pneumonectomy, was associated with improved treatment
success in multidrug-resistant Tb. It was not excluded, however, that
“healthier” patients were preferentially chosen for surgery, leading
to a bias. The confounding by indication, as patients most likely to
benefit are selected for the treatment, has been a limitation in many studies [1]. Despite the lack of reliable clinical trial data on efficacy
and safety of adjunctive surgical treatment, some countries of the
former SU continued to perform a high number of lung resections
[18]. A summary of indications from the World Health Organization
(WHO) publication compiled under participation of Russian experts
Drs. Dmitriy Giller (cited below), Boris Kazenniy and Denis Krasnov
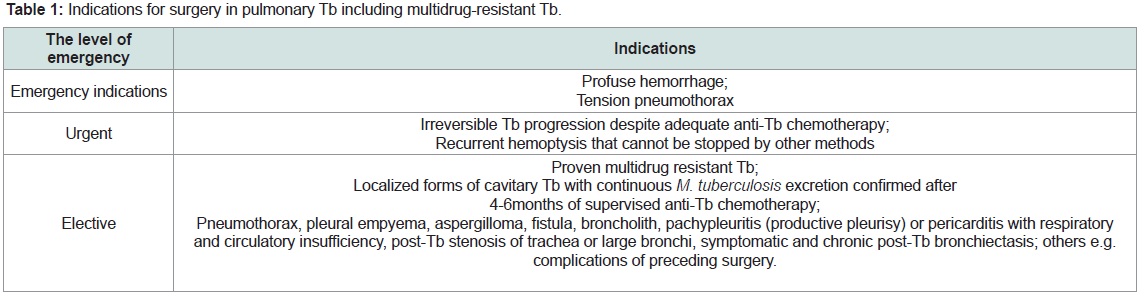
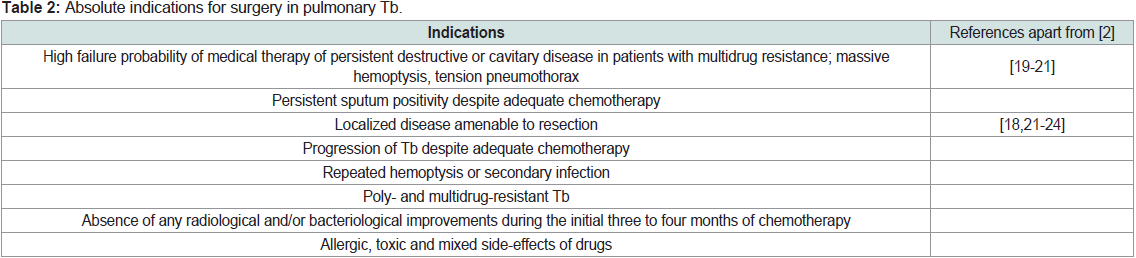
is presented here Table 1,2 [2].
Apparently, the WHO document was influenced by the Russian
experts, which is recognizable especially from Table 2 [2]. There
is an opinion that indications for surgery in Tb are rarely absolute
[14]. As for contraindications, they largely depend on the process
extension, preservation of the cardiopulmonary function and the
general state of heath [19,21,23]. The following contraindications for
elective surgery of pulmonary Tb (including multidrug-resistant Tb)
are listed in the WHO publication [2]: Extensive cavitary lesions of
both lungs; forced expiratory volume in 1 sec <1.5 L for lobectomy
and < 2.0 L for pneumonectomy; pulmonary-heart failure III-IV
(functional classification of the New York Heart Association); body
mass index up to 40-50% of the normal range; active bronchial Tb;
severe co-morbidity [2]. Tuberculoma (>2 cm, also in children) has
been generally regarded as an indication for surgery by Giller and
associates [25,26]. The same experts designated fibrocavitary Tb as
an absolute indication for surgery [26]. Tuberculomas >1 cm were
routinely operated on also without preceding anti-Tb therapy [27-29],
which is generally at variance with the international practice [18,30].
There has been an opinion since the 1950s that potential instability
of tuberculoma does not generally justify thoracic surgery and that
asymptomatic patients with an unchanging solid focus do not require
treatment. Tuberculoma as an indication for pulmonary resection
was seen differently from other forms of Tb where surgical risks could
in some cases be justified by a poorer prognosis [31]. Nonetheless,
tuberculoma was the most frequent indication for lung surgery in
Tb patients at the Moscow I.M. Sechenov Medical Academy (44.2%) [4], while at other institutions this percentage reached 50-80% [30].
In particular, tuberculoma has been the most frequent indication for
surgery among adolescent Tb patients [25]. Children were routinely
operated for tuberculomas, non-specific inflammatory, fibrotic
lesions and bronchiectasis [32]; more references are in the preceding
review [33]. Bilateral resections were performed in various Tb forms
including solitary tuberculomas on both sides [34-36]. A study from
the above-mentioned Institute for Phthisiopulmonology reported 771
lung surgeries, including 168 pneumonectomies, 181 lobectomies and
bilobectomies, 180 smaller resections, performed in 700 Tb patients
with drug resistance, up to 4 operations pro patient. Postoperative
complications were observed in 100 cases (12.9%), fatal cases - 12
(1.5%) [37]. Another example from the same institution: among 60
operated Tb patients (16 pneumonectomies, 24 lobectomies and
smaller resections) the complication rate was 37%, mortality – 5%;
18.3% were discharged from the hospital with persisting complications
[38].
Resections were performed for tuberculoma, infiltrative and
cavitary Tb without preceding medical treatment or within one
month after the diagnosis i.e. when the drug therapy could have
been efficient [28,39]. In diabetics, it was recommended to operate
tuberculoma after 2-5 months of medical therapy [40]. The authors
operated asymptomatic patients and recorded the 15.73% rate of
postoperative complications [41]. Apparently, complication rates
have been sometimes underestimated due to limited follow-ups.
Lung operations for Tb were performed and recommended also for
aged patients with comorbidities [42-44]. Sokolov found indications
for surgery in 210 from 289 (72.6%) aged Tb patients (50-73 years
old) and operated on 180 (62.2%) of them, 144 operations being lung
resections. Among the latter 144 patients, 93 (66.4%) had cavitary
disease and 43 (30.8%) – tuberculoma. Reactivation of Tb early
after surgery was noted in 8.6% of cases, fistula - 27.2 %, atelectasis
or incomplete lung re-expansion - 20%, pneumonia - 5.7%, pleural empyema - 3.6%, other complications - 12.9%; 8 (5.7%) patients
died after the surgery [44]. Tuberculoma was the most common
indication, and lobectomy – the most frequent modality in elderly
Tb patients, whereas epidemiological considerations i.e. potential
contagiousness was listed among arguments in favor of the surgical
treatment [43]. Statements of this kind can be found also in recent
papers e.g.: “Surgery in patients with tuberculomas is recommended
to reduce their infectiousness” [16]. In the author’s opinion, it is
unethical to subject a patient to a thoracic surgery just because he
or she is potentially contagious. In any case, the patient must be
comprehensively informed about potential benefits and risks so
that he or she could make an independent decision according to the
principle of informed consent.
Bilateral resections were performed in various Tb forms including
solitary tuberculomas on both sides or tuberculoma and cancer [34-36,45-47]. Indications for a second lung surgery were found in 20-
37% of previously operated Tb patients [48]. Postoperative relapses
of Tb were regarded as indications for repeated surgeries up to
“concluding pneumonectomy” and resections of the remaining lung
after pneumonectomy [35,46]. For example, repeated resections on
both sides with a subsequent pneumonectomy were performed in
one patient along with 52 bronchoscopies [49]. Lung resection or
pneumonectomy was deemed permissible even in cases of severe
respiratory insufficiency [45,46,50,51]. Bilateral resections or
pneumonectomy plus contralateral “economic” (sparing) resection
were regarded to be indicated for patients with a Tb lesion on one
side and non-specific inflammatory and/or fibrotic lesion on the other
side [52].
Several words should be said about bronchoscopy (Bs) that has
been applied in all forms of Tb in children and adults also when Tb
was suspected (references are in the preceding article [53]; it was
recommended for young patients with “hyperergic” (high degree of
hypersensitivity) tuberculin tests or within the diagnostic algorithm
for suspected Tb in smear-negative cases [54,55]. After a detection of
M. tuberculosis, an urgent hospitalization and examination including
Bs is currently recommended [55]. Primary Tb was regarded as an
indication for Bs in children [56]. Bs was designated as one of the main
diagnostic methods for focal non-destructive Tb [57]. In destructive
(cavitary) Tb, repeated therapeutic Bs (1-2 weekly during 2-4 months)
were recommended by the Ministry of Health [58]. Bs was used as
a screening tool for Tb in patients with general malaise, both with
positive and negative tuberculin tests [59]. Some researchers used
Bs as a second step of screening for Tb in children [60]. Therapeutic
Bs and bronchoscopic monitoring has been applied in pulmonary
Tb also with non-specific bronchial lesions [61-63]. For example,
22,469 Bs were performed in 5195 patients, including 1766 (34%)
older than 65 years, at the Tb hospital No. 3 in Moscow (705-1225
beds at different times) from 1994 through 2013 [64]. In particular,
some military doctors performed many Bs e.g. 1478 procedures in 977
young (19.5 ± 0.1 years old) as well as in other patients diagnosed with
community-acquired pneumonia [65-68].
Outside the former SU, Bs has not been routinely performed
in all Tb patients [69]. There is an opinion that in children Bs is
usually unnecessary, although the procedure may be useful in
diagnosing endobronchial TB [70,71]. Bs does not usually improve the microbiological diagnosis being not more sensitive for the culture
than properly obtained gastric aspirates [70,72-75]. Endoscopic
biopsy is a reliable sampling method for endobronchial Tb as well as
for hilar and mediastinal lymph nodes. Bs is generally regarded to be
indicated for patients with persistent cough, haemoptysis and signs of
bronchostenosis such as wheezing and stridor [69]. Bs is performed
before surgery in Tb patients to rule out endobronchial disease at the
proposed site of the bronchial stump [14]. As endobronchial Tb may
mimic neoplasms, Bs plays an important role to rule out cancer. In
this connection, Bs is complementary to computed tomography (CT),
which evaluates the bronchial involvement and luminal patency.
In particular, the multiple detector CT with post-processing tools
such as virtual bronchoscopy is an efficient diagnostic method for
central airway lesions [76]. Reportedly, CT depicted the cause of
bleeding more frequently than Bs (77% vs. 8%, p < 0.001), whereas
the two methods were comparable for identifying the site of bleeding
[77]. Some data suggested that CT can replace Bs e.g. as the firstline
procedure for the screening patients with massive hemoptysis.
Replacing Bs with induced sputum testing removes the risks from
bronchoscopy including that of nosocomial infection [78]. Of note,
endoscopy is among the risk factors of nosocomial infections e.g.
viral hepatitis [79], especially in conditions of suboptimal procedural
quality assurance. Not surprisingly, the incidence of viral hepatitis
(predominantly B) was reported to be 5 times higher in Tb patients
than in the general population of Russia [80]. Outbreaks of infections
including Tb occurred after fiberoptic instruments were used [81-83]. Reportedly, Mycobacteria were the greatest obstacle to the
infection control in Bs units [83]. It has been suggested that Bs may
spread infection within the lung, from one patient to another, and
- by triggering coughing - cause airborne infection of other people
[84]. The use of Bs with questionable indications has been reviewed
previously [53].
The surfactant (Sf) therapy of pulmonary diseases (Tb, acute
respiratory distress syndrome, pneumonia etc.), excluding neonatal
respiratory distress syndrome (RDS) with primary surfactant
deficiency, and bronchoscopy as the delivery method have been
discussed previously [85-88]. Sf-BL from bovine lungs has been
developed and permitted for clinical use in Russia. The manufacturing
method is described in the patent [89] (partly translated in
[85,86],
where it is noted that Sf-BL contains ~2% of protein. Endobronchial
instillations of xenogeneic proteins may cause immune reactions and
transmission of infection [90]. In older patients, a more pronounced
immune response can be expected than in premature infants with
RDS. Endobronchial instillations of porcine Sf were accompanied
by an augmentation of eosinophilic inflammation in patients with
bronchial asthma [91]. Rosenberg et al. used St-BL in asthma,
bronchitis, pneumonia, chronic obstructive pulmonary diseases and
Tb (more references are in the review and patent [89,92], as well as
in COVID-19 [93], where immune and inflammatory reactions might
contribute to the “cytokine storm” and collagen synthesis. Bs was used
as the delivery method of Sf [92,94-101] with a biopsy of lung tissue
in [95]; other studies used inhalations. Apart from inhalations, Bs was
used within the framework of Sf research in Tb patients [101,102].
Sf-BL was recommended by a Letter of the Health Ministry for the
treatment of viral (A/H1N1 influenza) pneumonia [103]. This Letter
refers to the manufacturer’s instruction No. 003383/01-230710, where it is stated that the optimal method of the Sf delivery is Bs with an
instillation into individual segmental bronchi [104]. No comparable
recommendations have been found in the literature. Until recently,
Oleg Rosenberg had been director of the manufacturing firm Biosurf
(https://biosurf.ru/). No conflicts of interest have been declared in
his publications. Rosenberg applied misquoting in his papers on Sf,
specified in detail previously [87,88]. Some studies from Russia have
reported that inhalations of Sf improve effectiveness of the anti-Tb
therapy, significantly accelerating healing, dissolution of specific
infiltrations and closing of caverns, while M. tuberculosis disappeared
from sputum at an early date [89,102,105-107]. No similar reports
have been found in the international literature. Finally, intravenous
injections of stem cells to Tb patients should be mentioned together
with the warning against unjustified use of Bs for such purposes as it
has previously been done concerning intracoronary injections of cells
obtained from the abortion material [108-112].
The treatment of patients suffering both of Tb and alcoholism needs
a special comment. According to official instructions, indications for
surgery were broader in alcoholics than in other Tb patients [113]. In
case of alcoholism, the surgical treatment was recommended earlier
i.e. after a shorter period of medical therapy [29]. Among other
things, vocal cord injuries were observed after repeated Bs sometimes
performed in conditions of suboptimal procedural quality assurance.
It was noticed that vigorous apomorphine-induced vomiting as
emetic or aversive therapy of alcoholism provoked hemoptysis [114].
The following treatments were applied to alcoholics: prolonged
intravenous infusions, sorbent hemoperfusion, endobronchial and
endolymphatic drug delivery, pyrotherapy with sulfozine (oil solution
of sulphur for intramuscular injections), endoscopic and surgical
biopsies, sometimes without clear indications also for research [115-118]. Infusions for the purpose of detoxification were generally
recommended for patients with alcohol dependence and alcoholism
including moderately severe withdrawal syndrome [119-122]. The
prescribed duration of detoxifying treatment was 10-12 days [119].
This included intravenous drip infusions of solutions: sodium and
calcium chloride, sodium thiosulfate, magnesium sulfate, glucose,
dextran etc. (7-10 infusions daily, alternating with intramuscular
injections). The latter is at variance with the international literature.
Alcohol and its metabolites are eliminated spontaneously while
rehydration can be normally achieved per os. Intravenous glucose and
magnesium are generally not recommended for patients with alcohol
withdrawal syndrome [123,124]. Excessive infusions of magnesiumcontaining
solutions are associated with adverse effects also in treated
alcoholics [125]. Moreover, the detoxifying treatment of alcoholics
included intramuscular injections of 10-15 ml of 25% magnesium
sulfate solution together with 10 ml 40% glucose, 10 ml of 10% calcium
chloride and 10 ml 30% sodium thiosulfate solutions, subcutaneous
infusions of up to one liter of isotonic saline etc. [119,126,127] In
conditions of suboptimal procedural quality assurance, repeated
infusions, endovascular and endoscopic manipulations can lead to the
transmission of viral hepatitis, which was known to occur to treated
alcoholic patients.
Discussion
The outpatient treatment of Tb patients, usual in other countries,
was supposed to be hardly applicable in Russia [128]. According to the governmental Ordinance No. 378 of 16 June 2006, patients with
infectious Tb are not allowed to live in one apartment with other
people. As per the Federal Law No. 77 “Prevention of the spread
of Tb in Russia” of 18 June 2001 (amended 2013), “Patients with
contagious forms of Tb, repeatedly violating the sanitary and antiepidemic
regime, as well as those deliberately evading examinations
for Tb or [emphasis added] the treatment of Tb, are hospitalized into
phtisiological institutions for obligatory examination and treatment
by court decisions.” It is stipulated by the same Law that the principle
of informed consent is not applicable in this connection (Articles
7,9,10). A survey conducted across Russian phtisiological institutions
found >6000 relevant trials in the period 2004-2008 whereas 3163
patients were hospitalized after court decisions [129]. For example, in
the study from Kemerovo province, 463 trials were reported resulting
in 421 decisions of compulsory hospitalization of Tb patients [130].
There are administrative and legal mechanisms e.g. hospitalization of
Tb patients with the help of police and criminal prosecution in case of
non-compliance. Among others, the latter pertains to non-contagious
Tb patients released from prison [131].
The compulsory treatment was endorsed by regulations [115];
more details and references are in the review [118]. Reportedly, in 1994
about 60% patients of one of the “phtisio-narcological” institutions
for compulsory treatment escaped while a half of them were returned
by the police (militia) [132]. The duration of compulsory treatment
in such institutions was around one year or longer [115]. In 1974,
chronic alcoholism was officially declared to be a ground for the
compulsory treatment; the regulation was hardened in 1985, making
the compulsory hospitalization and treatment of chronic alcoholics
independent of anti-social behavior. This practice has been designated
in 1990 as contradictory to the human rights [133]. The system of
compulsory treatment for Tb was partly dismantled during the
1990s; but some experts recommended its restoration and further
development [129,130].
Conclusion
The surgical treatment of Tb is indicated for life-threatening
conditions such as massive hemoptysis from cavitary disease or
bronchiectasis. Adjuvant surgical therapy may be recommended for
selected patients especially with multidrug resistant Tb; however,
indications are rarely absolute [1,14,134]. The role of surgery
remains controversial. Clinical recommendations are not the goal of
this commentary. The message is that patients should not undergo
surgeries and other invasive procedures to comply with instructions
and doctrines fed by motives like personnel training, especially of
military surgeons, endoscopists, etc., without sufficient evidencebased
indications [33]. The approach should be individual based
on the consensus expressed in the recent international literature.
The principle of informed consent must be observed - patients
comprehensively informed on potential benefits and risks to be able
to make an independent decision.
The principle of informed consent has not been uniformly
adhered to in the former SU, which was facilitated by the widespread
paternalistic attitude to patients. Informed consent started only
recently to be mentioned in papers reporting research using invasive
methods e.g. bronchoscopic study of childhood asthma, where the
consent of parents was regarded to be sufficient [135]. Note that the principle of informed consent or assent is applicable also to adolescents
and children [136,137]. Even today, patients are sometimes requested
to sign in advance a form certifying their blanket consent to unnamed
diagnostic and therapeutic procedures. The factors contributing to
the persistence of suboptimal practices included the authoritative
management style, disregard for the rules of scientific polemics,
insufficient use of the foreign literature and absence of many
internationally used handbooks even in central medical libraries
[138,139]. Thanks to the Internet, the foreign literature is used
increasingly, while the practice is adjusted to international standards.
However, some papers containing questionable recommendations
have remained without due commentaries, so that persistence of
suboptimal practices or reversion to them is not excluded. Other
invasive procedures applied with questionable indications have been
reviewed previously [33,53,140,141].
References
21. Dewan R, Pasechnikov A (2013) Tuberculosis (TB) surgery guideline. Médecins Sans Frontières, Paris.