Journal of Surgery
Download PDF
Case Report
*Address for Correspondence: Dr. Jory Simpson MD, FRCSC, St. Michael’s Hospital, University of Toronto and CIBC Breast Centre, 30 Bond Street, Suite 3 003, Toronto ON M5B1W8, Canada, E-mail: simpsonjo@smh.ca
Citation: Simpson JS, George R. An Unusual Presentation of a 15-Year-Old Adolescence with Invasive Breast Cancer. J Surgery. 2013;1(1): 4.
Copyright © 2013 Simpson JS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 1, Issue: 1
Submission: 12 July 2013 | Accepted: 22 August 2013 | Published: 26 August 2013
Reviewed & Approved by: Dr. Ku Sang Kim, Department of Surgery, Ajou University School of Medicine, South Korea
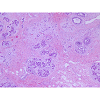
At this point she was referred for a second surgical opinion. Her breast mass was now 7 cm on clinical exam, indicating a strong propensity for rapid growth. After reviewing her case at a multidisciplinary conference she underwent a surgical excisional biopsy 9 months after her initial presentation (Figures 5 and 6). The final pathology confirmed multiple foci of invasive tubular carcinoma with a maximum dimension of 4.5 mm. It was Nottingham grade 1/3, lymphovascular invasion was identified and hormone receptors were positive and negative for the Her2/neu receptor. In addition, grade 2, ductal carcinoma in situ (DCIS) was identified with a maximum extent of 13 cm. With regards to her surgical margins the distance to the nearest margin of invasive carcinoma was 0.9 mm and DCIS was present at the posterior and lateral margin.
Expedited genetic testing was performed for BRCA mutations and Li-Fraumeni Syndrome and was negative. She returned to the operating room for a unilateral skin and nipple-sparing mastectomy with immediate reconstruction with Alloderm and an implant. In addition, a sentinel lymph node biopsy was performed. Her final pathology identified multiple foci of residual invasive tubular carcinoma and DCIS, no evidence of metastatic disease to 2 lymph nodes and no disease at the surgical margins.
An Unusual Presentation of a 15-Year-Old Adolescence with Invasive Breast Cancer
Simpson JS1,2*, and George R1,2
- 1St. Michael’s Hospital, University of Toronto, Toronto, Canada
- 2CIBC Breast Centre, Toronto, Canada
*Address for Correspondence: Dr. Jory Simpson MD, FRCSC, St. Michael’s Hospital, University of Toronto and CIBC Breast Centre, 30 Bond Street, Suite 3 003, Toronto ON M5B1W8, Canada, E-mail: simpsonjo@smh.ca
Citation: Simpson JS, George R. An Unusual Presentation of a 15-Year-Old Adolescence with Invasive Breast Cancer. J Surgery. 2013;1(1): 4.
Copyright © 2013 Simpson JS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 1, Issue: 1
Submission: 12 July 2013 | Accepted: 22 August 2013 | Published: 26 August 2013
Reviewed & Approved by: Dr. Ku Sang Kim, Department of Surgery, Ajou University School of Medicine, South Korea
Case Presentation
A 15 year-old girl of Bangladesh decent presented with a 2-month history of a left breast mass associated with pain and spontaneous bloody nipple discharge. She was otherwise healthy and on no regular medications. With regards to risk factors for breast cancer she reached menarche at 12 years of age, she was a nulligravida, lacked a history of thoracic radiation exposure and family history of breast or ovarian cancer.Physical examination identified breast thickening around the 12 O’clock region but no discrete masses. An ultrasound showed at the palpable area of concern, an area of dense breast tissue with dilated ducts but no discrete masses (Figure 1). She was reassured and follow up was arranged for 3 months. At follow up the palpable area in the central upper breast had increased in size and was now a defined mass roughly 4 cm in size. An MRI showed asymmetric progressive non-mass like enhancement of the left upper breast with irregular tubular enhancement and an indeterminate mass at 2 O’clock position correlating with the dilated duct seen on ultrasound (Figure 2). A mammogram, done only in medial-lateral-oblique (MLO) view to minimize radiation exposure, identified global asymmetry in the superior portion of the left breast without any suspicious calcifications or distortions (Figures 3 and 4). She subsequently underwent an ultrasound guided core biopsy with 3 core samples. The final pathology showed intraductal epithelial proliferation with increased cellularity and oedema of the surrounding stroma possibly resulting from a duct rupture. In addition, a papillary lesion with focal atypia of uncertain significance was also identified. There was no evidence of juvenile papillomatosis, in situ or invasive breast carcinoma. A second pathologist at an outside institution confirmed this report.
Postoperatively she was not offered adjuvant radiation. Her tumor was found to have an intermediate risk of recurrence (14%) based on an Oncotype DX score of 23. She received adjuvant chemotherapy with Taxotere and Cyclophosphamide and endocrine therapy with Tamoxifen.
Discussion
Breast Cancer rarely occurs in young women. Less than 0.1% of all breast cancers occur in women under the age of 20 years as described in this case while 1.9% occurs between the ages of 20 and 34 and 10.6% between 35 and 44 [1]. According to the Surveillance Epidemiology and End Results (SEER) database, between 1975 and 2006 there were no incident cases of breast cancer in situ in females less than 20 years of age [2]. Secretory carcinoma of the breast is however more common in women under 20 years of age and there have been published reports in children as young as 12, 7 and even 6 years old [3-5]. This case is novel in that the pathology was consistent with Invasive tubular carcinoma of the breast. There are unique issues that need to be addressed when treating young women with a diagnosis of breast cancer. This discussion will outline important management strategies from the time of diagnosis to treatment and finally into survivorship.Only 10% of breast cancers are attributable to a germ-line mutation such as BRCA1 or BRCA2 while 20% have a familial component leaving the majority of breast cancer to be sporadic cases. In a study that examined 89 patients under the age of 39 with breast cancer, 8 patients (9%) were discovered to carry a mutation for the BRCA1 or BRCA2 gene [6]. Despite the fact that most breast cancers in young women remain spontaneous it is still important to recognize that breast cancer in young women is associated with rare genetic disorders (Cowden disease and Li-Fraumeni syndrome) and exposure to ionizing radiation during childhood (mantle field irradiation for pediatric Hodgkin lymphoma). Confirming the presence or absence of a genetic mutation may alter not only immediate management but have implications on the risk for other related malignancies in both the patient and their family members.
This case highlights the difficulty at times of diagnosing breast cancer in younger women. MRI is a useful adjunctive modality to mammogram and ultrasound when one is unable to establish the diagnosis of breast cancer. However even MRI has been shown to have a modest false-negative rate as demonstrated by Teifke et al. who reviewed 354 breast malignancies and their associated preoperative MRI findings. They found that 28 (8.4%) of the 334 invasive and 13 (65%) of the 20 intraductal carcinomas were missed with preoperative MR imaging yielding a false-negative rate of 8.4% for invasive breast cancer and even higher for DCIS [7]. In a patient with a negative mammogram, ultrasound and MRI an enlarging palpable abnormality on clinical exam should not preclude a biopsy as highlighted by this case.
With advances in imaging and biopsy techniques the majority of women who undergo breast surgery today have a preoperative pathological diagnosis as the indication for surgery. This case highlights the fact that despite benign imaging and core biopsy results, a surgical biopsy is at times still warranted based solely on the suspicious finding on clinical exam such as an enlarging mass that was not concordant with imaging and the biopsy pathology. It is of upmost importance when managing diseases of the breast to ensure that your pathology is concordant with your imaging and clinical exam. If any of the 3 modalities remains in question a surgical biopsy is recommended.
The optimal management of young women with breast cancer is not well established given the paucity of literature and evidence in this age group. A population based Danish cohort of 9,285 premenopausal women with breast cancer was examined and a local recurrence incidence of 15.4% after breast conserving surgery among 719 women under the age of 35 was found. This is in comparison to 3% in women between the ages of 45 and 49. There was no difference in survival between the 2 groups [8]. Thus, age alone is not a contraindication to breast conserving surgery (BCS). The decision to proceed with a mastectomy and possibly a contralateral prophylactic mastectomy will be influenced by genetic testing and if possible expedited testing is ideal. A key issue to be discussed with your young patient that may influence a decision to proceed with BCS is the lack of long-term data on the late effects of adjuvant radiation such as cardiac dysfunction and secondary malignancies. This uncertainty contributed to the decision to proceed with a completion mastectomy in the case presented here. A preoperative consultation with a Radiation Oncologist will allow for an informed decision to be made on the ideal surgical management.
Chemotherapy and endocrine therapy remains the mainstay of systemic treatment of hormone receptor positive premenopausal breast cancer. Ovarian ablation in young women has fallen out of favor. The Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) published a meta-analysis of randomized trials on ovarian ablation and found the beneficial effect of ovarian ablation appeared to be large only in the absence of chemotherapy. No advantage was seen when ovarian ablation was added to cytotoxic chemotherapy [9]. Given the fact that adjuvant chemotherapy is widely used in premenopausal breast cancer, ablation of ovaries is not an initial requirement. The EBCTCG also showed in a separate meta-analysis of randomized trials that Tamoxifen for 2-5 years was beneficial in patients less than 40 years of age [10].
One of the major concerns of patients and physicians following completion of adjuvant treatment is the risk of temporary or permanent amenorrhea resulting in infertility or early onset menopause. This devastating threat needs to be addressed early prior to commencing treatment, as some women will want to explore fertility interventions. The ultimate risk of amenorrhea is mostly related to the patient’s age and the combination of treatments she receives as older premenopausal women who receive chemotherapy and endocrine therapy have the highest probability of onset of menopause during the first year after diagnosis [11]. In this case, our patient elected not to undergo a fertility consultation after a discussion with her family.
In conclusion, diagnosing and managing breast cancer in young women is challenging and requires a multidisciplinary approach. No two cases are identical and care needs to be individualized to ensure an optimal oncologic as well as psychosocial outcome. It is extremely uncommon for breast cancer to present in a 15-year-old female. This case highlights many of the principles required when managing difficult diagnostic challenges and addresses some important differences in managing premenopausal breast cancer.
Four Key Summary Points
1- A “triple test” requires concordance between your physical examination, radiologic examination and needle biopsy. When there is a discrepancy between any of the aspects of evaluation a surgical biopsy should be performed.2- Despite the fact that breast cancer is uncommon in young women, its presence must always be ruled out.
3- The same treatment principles that apply to post menopausal breast cancer apply to premenopausal women however it is important to be cognizant of the long-term adverse outcomes of many of the adjuvant treatments.
4- Early engagement of a multidisciplinary team is essential when treating young women with breast cancer.
Differential Diagnosis of Breast Mass in Female Adolescents
Fibrocystic ChangesFibroadenoma
Phyllodes tumor (propensity for rapid growth)
Intraductal Papilloma
Mammary duct ectasia
Breast Trauma
Breast Infection
Primary Breast Cancer
Secondary Malignancy
Resources for Young Women with Breast Cancer
Rethink Breast Cancer (National)Rethinkbreastcancer.com
Contact: 1-866-738-4465
Young Adult Cancer Canada (YACC) (National)
Youngadultcancer.ca
Contact: 1-877-571-7325
Willow, Breast Cancer Support Canada (National)
Willow.org
Contact: 1-888-778-3100
Cancer Chat Canada (National)
Cancerchatcanada.ca
Contact: 1-800-663-3333
Acknowledgements
I would like to acknowledge all the nurses and staff at the CIBC Breast Centre at St. Michael’s Hospital for their compassion and care in this challenging case.References
- (2006) Stat bite: Breast cancer in young U.S. women. J Natl Cancer Inst 98: 1762.
- Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, et al. (2007) SEER Cancer Statistics Review, 1975-2005, National Institute, Bethesda, MD.
- Tadesse A, Tesfaye W, Hailemariam B (2012) Breast carcinoma in a 7-years-old girl. Ethiop Med J 50: 89-94.
- Nonomura A, Kimura A, Mizukami Y, Nakamura S, Ohmura K, et al. (1995) Secretory carcinoma of the breast associated with juvenile papillomatosis in a 12-year-old girl. A case report. Acta Cytol 39: 569-576.
- Murphy JJ, Morzaria S, Gow KW, Magee JF (2000) Breast Cancer in a 6-Year-Old Child. J Pediatr Surg 35: 765-767.
- Golshan M, Miron A, Nixon AJ, Garber JE, Cash EP, et al. (2006) The prevalence of germline BRCA1 and BRCA 2 mutations in young women with breast cancer undergoing breast-conservation therapy. Am J Surg 192: 58-62.
- Teifke A, Hlawatsch A, Beier T, Werner Vomweg T, Schadmand S, el al. (2002) Undetected malignances of the breast: dynamic contrast-enhanced MR imaging at 1.0 T. Radiology 224: 881-888.
- Kroman N, Holtveg H, Wohlfahrt J, Jensen MB, Mouridsen HT, et al. (2004) Effect of breast-conserving therapy versus radical mastectomy on prognosis for young women with breast carcinoma. Cancer 100: 688-693.
- (1996) Ovarian ablation in early breast cancer: overview of the randomized trials. Early Breast Cancer Trialists’ Collaborative Group. Lancet 348: 1189-1196.
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trials. Lancet 365: 1687-1717.
- Goodwin PJ, Ennis M, Pritchard KI, Trudeau M, Hood N (1999) Risk of menopause during the first year after breast cancer diagnosis. J Clin Oncol 17: 2365-2370.