Journal of Pharmaceutics & Pharmacology
Download PDF
Review Article
Repurposing of Adamantanes with Transmitter Receptor Antagonist Properties for the Prevention/Treatment of COVID-19
Brenner SR1*, and Butterworth RF2
1Department of Neurology, Saint Louis University, USA
2Department of Medicine, University of Montreal, Canada
*Address for Correspondence: Brenner SR, Department of Neurology, Saint Louis University, (retired) St. Louis, Missouri, USA; E-mail: sbren20979@aol.com
Submission: 08 October 2020;
Accepted: 12 November 2020;
Published: 24 November 2020
Copyright: 2020 Brenner SR. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Members of the adamantane family of agents in general and two
such members, amantadine and memantine, in particular, have
established beneficial actions across a wide range of infectious
diseases including those caused by coronaviruses. Increasing
evidence suggests that the protective effects of these agents is the
result of actions on neurotransmitter systems namely the NMDA
receptor subclass of the glutamatergic system and by the α7-nACh
subclass of nicotinic cholinergic receptor. The potent NMDA receptor
antagonist, memantine, prevents motor disabilities and reduces
replication of the neuroinvasive/neurotropic human respiratory virus
HCoV-OC43 dose-dependently. Moreover, the lysosomotrophic
adamantanes amantadine and memantine also limit viral replication.
Known lysomotrophic agents such as ammonium chloride inhibit
cellular entry of SARS-CoV-2 on laboratory testing. Inhibiting clathrinmediated
endocytosis (cellular entry) of the SARS-CoV-2/ACE2
complex by amantadine or rimantadine may block viral entry into
vulnerable cellular populations, and also reduce platelet activating
factor-priming of Polymorphonuclear [PMN] cells, potentially lessening
PMN cell-mediated tissue damage and excess Neutrophil Extracellular
Traps [NETs] seen in advanced cases of COVID-19. Rimantadine has
inhibitory effects of SARS-CoV-1, a closely-related virus to SARS-CoV-2,
which may indicate the need for further evaluation as a treatment
for COVID-19. Amantadine increases Dopamine [DA] release and
blocks its reuptake, increasing its action on DA receptors on T cells
thus activating resting effector T cells and suppressing regulator T cells,
which may have a beneficial immunomodulating function in infectious
diseases. Proposed adverse effects of smoking on COVID-19 outcomes
are attributed to the effects of nicotine via the α7-nACh receptor
located on bronchial and alveolar epithelial cells. As an antagonist of
this receptor, memantine has the potential to prevent the entry of SARSCoV-
2 into these cells. Independent case reports provide evidence
of protective effects of amantadine and/or memantine against
COVID-19. Additional epidemiologic studies however indicate a lower
incidence of smoking in hospitalized patients, stimulating investigations
of nicotine-related aspects, and amino acid sequence analysis
indicate homologous sequences with those of neurotoxins seen in
snake venoms blocking the α7-nAChR suggesting that COVID-19 may
be a disease of the nicotinic cholinergic system; α7-nAChR is involved
in the cholinergic anti-inflammatory pathway or reflex. COVID-19 is a
biphasic disease, the initial aspect involved with the initial infection and
viral replication which stimulates a prominent innate immune response.
This then transitions to the adaptive immune response with suppression
of infection and recovery, while the innate response is suppressed via
the cholinergic anti-inflammatory pathway. Severe disease may occur
when the initial innate immune response continues, the cholinergic
anti-inflammatory pathway being arrested by the neurotoxin inherent
in the viral amino acid sequence, causing a runaway innate immune
response. Memantine, being an inhibitor of α7-nACHR, could possibly
make COVID-19 worse should it be α7-nACHR inhibitor. Tilorone,
a lysosomotrophic agent and α7-nACHR agonist could also have
potential as a treatment for COVID-19. Further studies are necessary
to determine whether repurposing of adamantanes is beneficial in
COVID-19, and for further investigations of pharmacological and
pathophysiological properties of SARS-CoV-2.
Keywords
COVID-19; Coronavirus; Adamatanes; Amantadine; Memantine; SARS-CoV-2; Re-purposing, NMDA receptor antagonist;
α7-nAChR; Viral replication; Lysosomotropic; ACE-2
Introduction
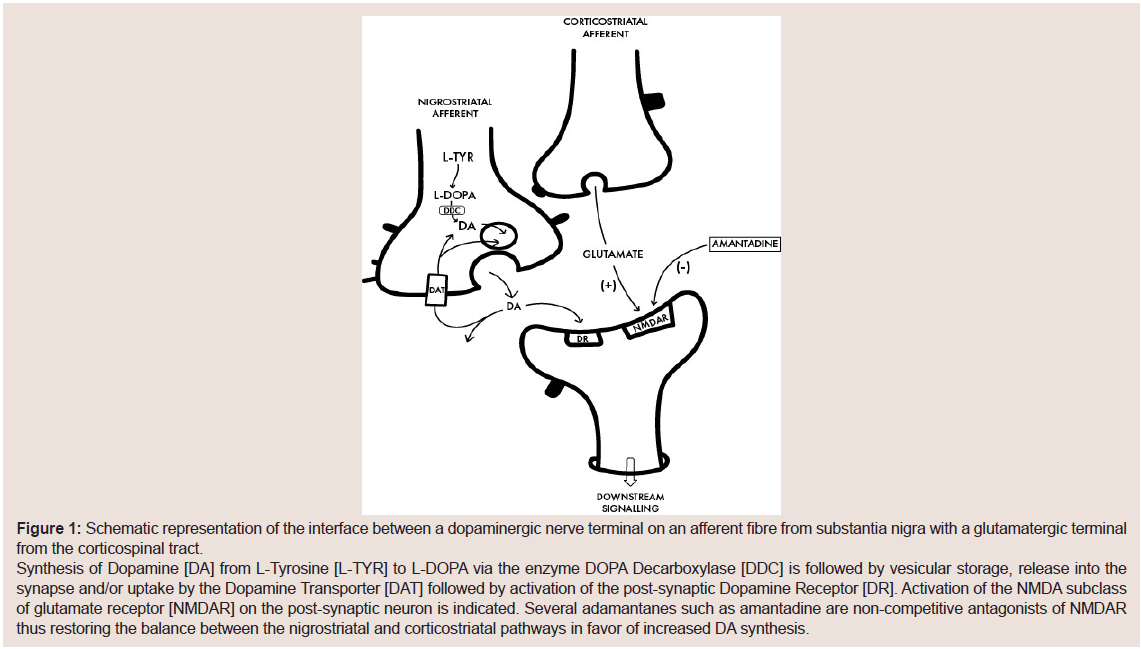
Several members of the adamantane family of agents manifest
potent non-competitive antagonist properties at the NMDA subclass
of glutamate receptors that are effective for decreasing excess
glutamatergic activity in the CNS that may, if unchecked, result in
the phenomenon known as excitotoxicity that is widely recognized
to be responsible for a range of neurological disorders including the
epilepsies as well as the common neurodegenerative Alzheimer’s
Disease [AD] and Parkinson’s Disease [PD] [1,2]. For example, the
adamantane derivative and potent NMDA antagonist amantadine
is widely employed for the treatment of the disturbances of motor
function in PD and for the control of L-Dopa-induced dyskinesias
in PD patients [2]. The mechanism of action involves its action as
a non-competitive antagonist of the NMDA receptor the net result
of which is to redress the imbalance between afferent dopaminergic
projections from substantia nigra with those of corticospinal
glutamatergic inputs as shown in a simplified schematic manner in
Figure 1. Amantadine, is also increasingly being prescribed for the
treatment of traumatic brain injury and its associated cognitive and
behavioral complications effects that have been also ascribed to its
NMDA receptor antagonist properties [3]. Another adamantane related
NMDA antagonist, memantine, is currently employed for the
management and treatment of AD [4] (Figure 1).
Dopamine [DA], with increased release and concomitant
blockade of re-uptake by amantadine, besides being a principal
neurotransmitter, is also a ‘neuroimmunotransmitter’, having
multiple effects on most if not all immune cells and activator of
resting effector T cells through DA receptors. DA activation of
resting effector T cells and suppression of regulatory T cells may be
beneficial in immunotherapy of infectious diseases as well as cancer
and medications having a dopaminergic effect on T cells include
amantadine, as well as L-dopa, bromocriptine, haloperidol, reserpine,
pergolide, pimozide and others [5].
Established anti-viral properties of the adamantanes:
Inhibition of viral replication has been demonstrated for a
number of adamantanes. For example, both amantadine and rimantadine have been shown to be active against the influenza A
virus [6]; tromantadine is active against the Herpes Simplex virus and
the adamantine derivative bananin manifests activity against SARS
coronavirus HCoV-1 where it was shown to be a potent inhibitor of
the helicase activities and to limit replication of the virus [7,8].Amantadine did not show detectable inhibition of SARS-CoV-1
in a fRHK4 cell line, however rimantadine did show detectable
inhibitory activity by neutralization tests with 9 isolates of the
coronavirus along with leukocytic interferon-alpha, interferon-beta-
1a, ribavirin, lopinavir, and baicalin [9]. When tested in a Vero-E6
cell line, rimandatine, along with glycyrrhizin, leukocytic interferonalpha
and interferon-beta were more active, with activity at 72 h.
Rimantadine was also active in a plaque reduction assay, however it
wasn’t as effective as interferons, activity reduced after 72 h and it was
concluded that it was unlikely to have significant in vivo activity [9].
Memantine relieves the neuronal impairment and damage caused
by the neurotropic Japanese Encephalitis Virus (JEV) where survival
times in JEV-infected mice were significantly prolonged, inflammatory
cell infiltrates and intravascular cuffing were significantly reduced
and mouse brain JEV content was reduced [10]. Memantine is also
able to prevent neuronal cell death due to ZIKA virus infection by
blocking NMDA receptors but had no effect on viral replication [11].
Adamantanes and human coronaviruses: experimental studies:
Human Coronaviruses [HCovs] are respiratory pathogens with
potent neuroinvasive properties. The HCoV-OC43 strain can infect
human neural cells resulting in activation of neuroinflammatory
and neurodegenerative mechanisms and this strain of HCOv is
neurovirulent in susceptible mice leading to encephalitis [12].
Moreover, a viral mutant with a single point mutation in the viral
surface S protein induces severe hind-limb paralysis that appears to
involve glutamate excitotoxicity via NMDA receptors in susceptible
animals. Treatment with memantine resulted in improvements in
clinical scores related to paralysis and other motor disabilities. In
addition, memantine attenuated body weight losses and mortality
rates and led to reduction in HCoV-OC43 viral replication rates in
the CNS in a dose-dependent manner [13].In order to further elucidate the mechanism of action responsible
for this antiviral action of memantine, use was made of two well
established cell lines namely i] mouse primary CNS cell cultures
[known to express NMDA receptors] and ii] a human epithelial cell
line commonly employed to amplify HCoV-OC43 [that does not
express NMDA receptors]. Memantine was found to reduce viral
replication rates in both cell types leading to the suggestion that the
antiviral action of memantine against this strain of coronavirus were
not solely dependent on the antagonism of NMDA receptors [14].
Moreover, the authors proposed that, given the fact that memantine
produced a significant anti-viral activity following primary infection
of susceptible host cells was indicative of the notion that inhibition of
viral replication had occurred following viral attachment to the host
cell receptor as had been shown for other adamantine derivatives
[4,6,7].
Adamantanes for COVID-19: evidence to date:
It has been suggested that the Acute Respiratory Distress
Syndrome [ARDS] in COVID-19 may be the consequence of the migration of SARS-CoV-2 trans-synaptically from the lungs and
nasal epithelium to the medullary cardio-respiratory center via the
peripheral nervous system from the lungs and through the cribriform
plate from the nasal epithelium [14]. Loss of sense of smell and taste
are common features of COVID-19 and are probably associated with
the CNS. The virus may be neurotrophic with the latent period from
infection to development of complications being the result of virus
propagation from the lungs and nasal epithelium to the CNS. It has
been proposed that memantine could be considered as a potential
treatment for COVID-19 by virtue of its ability to interfere with the
NMDA receptor leading to inhibition of excess glutamate release in
the medullary brainstem, a potential neurotoxic effect from depletion
of ACE2 contributing to ARDS [15].Other proposed mechanisms whereby amantadine appears to
result in inhibition of coronavirus replication include interaction of
the agent with the viral E protein and by disruption of lysosomal gene
expression [16,17]. Moreover, being itself a lysosomotropic agent
[18], memantine could conceivably mimic the effects of amantadine.
Along this same line of reasoning, a recent short report described the
results of studies suggesting that the E protein, an essential protein of
coronaviruses including SARS-CoV-2, is a potential ion channel and
that memantine is a potent E protein inhibitor with the potential to
curb viral virulence and abate COVID-19 [19].
SARS-CoV-2 virus entry into cells is inhibited by ammonium
chloride, which elevates endosomal pH blocking Cathepsin B and L.
[20]. Besides a laboratory study investigating lysosomal dynamics and
SARS-CoV-2, an epidemiologic study also may be applicable, since
widespread consumption of ammonium chloride, (NH4Cl, salmiak)
a known lysotrophic agent, enriched confectioneries, primarily in
Northern European countries (primarily Scandinavian), may, along
with bacillus Calmette-Guérin (BCG) immunization, be associated
with a significantly associated lower rates of COVID-19 related
deaths [21].
SARS-CoV-2 enters cells via clathrin-mediated endocytosis,
which is inhibited by amantadine, and rimantadine [22,23]. Excess
neutrophil extracellular traps, formed by neutrophils in response
to COVID-19 infection may cause the severe multi-organ effects in
multiple systems involving vasculature, immunity and coagulation
[24]. Platelet activating factor induces the release of neutrophil
extracellular traps [25]. Platelet priming of neutrophils likely
requires clathrin-mediated endocytosis of the platelet activating
factor receptor, and amantadine, along with a more potent inhibitor,
rimantadine, inhibits clathrin-mediated endocytosis, which inhibits
platelet activated factor priming of neutrophils [25]. Amantadine or
rimantadine may be able to reduce polymorphonuclear mediated
tissue damage in humans [26], and possibly reduce the production
of excess neutrophil extracellular traps through reduced priming of
neutrophils.
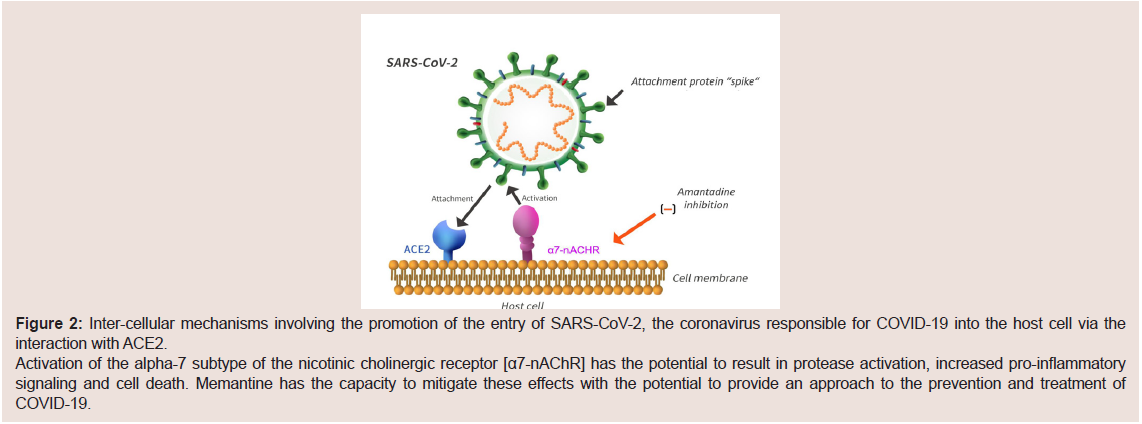
The nicotinic cholinergic receptor and COVID-19:
Results of a recent systematic review of the evidence suggest that
smoking is associated with an increase in progression and adverse
outcome of the disease in patients with COVID-19 and that current
smokers along with patients with COPD had increased airway
epithelial cell expression of the viral entry receptor ACE-2 [27]. A
robust mechanistic explanation was proposed involving nicotine exposure as the likely mediator acting specifically through the
alpha-7 subtype of nicotinic cholinergic receptor [α7-nAChR] that is
localized widely in airway cells such as bronchial epithelial cells, type
II alveolar epithelial cells and in interstitial lung fibroblasts in addition
to various cells of the CNS. Increased expression of ACE2 receptors is
mediated by the stimulation of α7-nAChR and any receptor agonist
would have the potential to promote the entry of SARS-CoV-2 into
the respiratory epithelium via ACE2 [28,29] (Figure 2).Therefore, it is likely that antagonists of α7-nAChR could have
the potential, by virtue of their ability to decrease ACE2 receptor
expression in respiratory epithelium and prevent SARS-CoV-2
invasion of pulmonary epithelial cells. Searches for such agents are
currently ongoing and, interestingly, memantine, in addition to its
well-established action as a non-competitive antagonist of NMDA
receptors, is a very potent antagonist of α7-nAChR [30]. It also exerts
protective anti-inflammatory effects by suppression of cytokine
expression as shown in an experimental model of lung injury [31].
Whether memantine is able to meaningfully alter ACE2 expression
and prevent SARS-CoV-2 entry into the airway epithelium must
surely be an important next step that is well worth further evaluation
at pace (Figure 2).
There is interplay between inflammatory and anti-inflammatory
mediators and α7-nAChR has been referred to as the antiinflammatory
reflex, mediated through the vagal nerve. This nicotinic
receptor subunit is essential for inhibiting cytokine synthesis by the
cholinergic anti-inflammatory pathway [31]. The SARS-CoV-2 virus,
while using the ACE-2 receptor for cellular entry, may also interact
with additional receptors. While observations [described above]
of smoking worsening COVID-19, conversely, there have been
clinical observations of lower smoking incidence among hospitalized
COVID-19 patients [32], stimulating further studies of the viral
genome, which identified a “toxin like sequence”, in the receptor
binding domain of the Spike Glycoprotein of SARS-CoV-2 (amino
acids 375-390) which is homologous to a sequence of a neurotoxin
NL2, a neurotoxin contained in Chinese (Taiwan) Cobra venom, one
of the snake venom toxins which interacts with nicotinic acetylcholine
receptors [33,34]. Blocking α7-nACHR through interaction with
the cobra venom-like neurotoxin would permit unrestrained
inflammation, while stimulating or protecting α7-nAChR with
nicotine and/or nicotinic cholinergic agonists could be antiinflammatory
[34]. Memantine’s interaction with α7-nAChR, would
likely have some influence on such SARS-CoV-2 spike glycoprotein/
α7-nAChR interactions, possibly protecting the receptor from viral
spike glycoprotein interaction with the acetylcholine receptor.
Memantine has been investigated with reference to developing
host-directed therapies as adjuncts to traditional antibiotic drugs,
and investigated with reference to promoting the host innate immune
defense system against pathogens, through α7-nAChR primarily
against bacteria, and it was found to stimulate production of
antiseptic protein S100A9, a component of calprotectin, (calprotectin
S100A8/S100A9)), the bactericidal enzyme MPO (myeloperoxidase),
and DNA in PMN’s and accelerates release of depolymerized
chromatin fibers in the extracellular space, suggesting or indicating
the formation of Neutrophil Extracellular Traps (NETS) [35]. This
study was primarily concerning treatment of neonatal meningitis.
However, activation of α7-nAChR by nicotine could be protective against NMDA receptor-activated excitotoxic glutamate activation in
adults, but possibly deleterious in neonates [36]. Viruses can induce
NET formation, entrapping viruses, however disproportionate NET
formation in response to viruses can have deleterious effects [37].
Widespread NET release has also been seen in severe COVID-19
post mortem examinations, which is also likely responsible for the
widespread thrombosis seen in such patients [36].
Severe COVID-19 patients have a burst of circulating
calprotectin that precedes cytokine release syndrome, and emergency
myelopoiesis releases immature and dysplastic myeloid cells [38].
The blockage of α7-nAChR with memantine and SARS-CoV-2
spike protein homologous neurotoxin sequences with α7-nAChR,
may have some similarities, stimulation of S100A9, a component of
calprotectin, and stimulation of the innate immune response, with
NET formation. This may indicate some effect on the innate immune
response, since rapid onset may inhibit the virus in the early phase
of infection. Transcriptome analysis revealed hundreds of genes
upregulated by SARS-CoV-2 in infected human bronchial epithelial
cells and human post mortem samples as prior analysis of neurons
injured by glutamate and normalized by the angiotensin receptor
blocker, Candesartan, indicating similar mechanisms in SARSCoV-
2 infection and neurons injured by glutamate including nuclear
factor kappa-B translocation [39].
The primary recognized action of memantine is blockade of
NMDA channels, a glutamate receptor subfamily [40]. Memantine
lowers inflammatory markers, however, including nuclear factorkappa
B, indicating it may act on additional receptors besides NMDA
receptors, the insulin receptor and reduction in inflammation
in cellular studies of astrocytes [41]. Memantine may be able to
inhibit viral glutamate induced inflammation and cell death, since
the transcriptome indicates similarities between that induced by
glutamate in experimental cellular laboratory studies and that
obtained from post mortem examination of patient derived material
and viral infected human bronchial epithelial cells.
Memantine or amantadine for prevention of COVID-19: clinical studies to date:
Given the fact that the COVID-19 pandemic has only been a
matter of everyday discussions and preoccupations for less than one
year for the vast part of the world, and given the even more recent
interest in the repurposing of members of the adamantine family of
agents many of which are known to possess antiviral potential, it is
not surprising that there have, to date been no published results of
randomized controlled trials to assess the efficacy of these agents to
say nothing of systematic reviews or meta-analyses of any published
findings. Consequently, much reliance and activity is devoted for
the moment on the reports of individual cases that are, by necessity,
generally uncontrolled and observational in nature. However, results
of three published reports have appeared so far involving a total of
24 patients in which there is subjective evidence of a protective effect
of amantadine or memantine against COVID-19 including patients
with comorbidities or severe neurological disorders [42-45]. In a
group of 15 patients [10 with multiple sclerosis, 5 with Parkinson’s
disease] whilst undergoing treatment with amantadine [100 mg qd]
for several months’ duration, tested positive for COVID-19. SARSCoV-
2 infection was confirmed by RT-PCR in upper and lower
respiratory specimens. All patients had been quarantined for 2 weeks following documented exposure but none of them went on to develop
clinical manifestations of infectious disease [43]. Similar findings were
subsequently independently reported in a patient with type-2 diabetes
and members of his immediate family all of whom tested positive
for COVID-19 and were being treated with amantadine as well as
in a further case of an amantadine-treated patient with Parkinson’s
disease [44,45]. In a related study, treatment with memantine [10
mg bid] was reported to manifest apparently protective effects in a
group of 7 patients with cognitive impairment who tested positive for
COVID-19 [42].
Figure 1: Schematic representation of the interface between a dopaminergic nerve terminal on an afferent fibre from substantia nigra with a glutamatergic terminal from the corticospinal tract. Synthesis of Dopamine [DA] from L-Tyrosine [L-TYR] to L-DOPA via the enzyme DOPA Decarboxylase [DDC] is followed by vesicular storage, release into the synapse and/or uptake by the Dopamine Transporter [DAT] followed by activation of the post-synaptic Dopamine Receptor [DR]. Activation of the NMDA subclass of glutamate receptor [NMDAR] on the post-synaptic neuron is indicated. Several adamantanes such as amantadine are non-competitive antagonists of NMDAR thus restoring the balance between the nigrostriatal and corticostriatal pathways in favor of increased DA synthesis.
A retrospective study of a national database of 5726 patients, 140
of whom subsequently died, did not reveal any statistical difference
in mortality of a group of patients between COVID-19 associated
mortality and ongoing treatment with memantine for dementia,
indicating it’s not likely to have therapeutic effects on patients with
COVID-19, however it did not seem to have any deleterious effects
[45].
It is likely that a vigorous innate immune response initially is
able to arrest viral replication preventing widespread viremia with
multi-system and multi-organ involvement. Later in the course, the
cholinergic anti-inflammatory pathway could suppress or inhibit the
innate immune response. Likely adamantane medications such as
amantadine and memantine could be helpful early in the course of
the illness, during the initial infection phase when a robust innate
immune response is necessary to arrest viral replication as well as
inhibition of viral entry into cells by inhibition of clathrin-mediated
endocytosis. Interestingly, chlorpromazine is a well-known inhibitor
of clathrin-mediated endocytosis, and a study is ongoing on the
repurposing of chlorpromazine for COVID-19: the reCoVery study
[46].
Conclusions
The adamantanes may have a number of effects on COVID-19,
previously seen in patients being treated with adamantanes for a range
of neurological diseases who also became infected with COVID-19.
Immune T cells, and essentially all immune cells express DA
receptors which are instrumental in activation. T cell activation
would be important in the immune response in COVID-19. DA
levels are altered in diseases such as PD and also may be decreased
in aging, which is one of the primary risk factors for severe disease
in COVID-19. Amantadine is known to increase the synthesis of DA
(Figure 1).
COVID-19 may also increase glutamate and inflammation, as
has been inferred in transcriptome analysis. Memantine, being an
NMDA receptor antagonist has the capacity to reduce glutamateinduced
inflammation and cell death.
Being lysomotrophic agents, adamantanes such as amantadine,
rimantadine and memantine appear to have the potential to manifest
direct inhibitory effects on viral development. For example, the
lysomotrophic agent, ammonium chloride, appears to have a strong
inhibitory effect on SARS-CoV-2 entry into experimental cell lines
by blocking the endosomal cysteine proteases, cathepsin B and L and
the transmembrane protease serine TMPRSS2 is also involved in viral
spike protein processing for binding to ACE2 enabling the virus to
enter vulnerable cells [20].
Amantadine and rimantadine may be able to inhibit viral entry
due to clathrin-mediated endocytosis, which is the method SARSCoV-
2 utilizes for cellular entry, and also reduce polymorphonuclear
[PMN] priming by platelets, possibly reducing cellular injury and inflammation, since much of the tissue destruction in viral infection
is due to tissue destroying factors released by PMN cells.
Figure 2: Inter-cellular mechanisms involving the promotion of the entry of SARS-CoV-2, the coronavirus responsible for COVID-19 into the host cell via the interaction with ACE2.
Activation of the alpha-7 subtype of the nicotinic cholinergic receptor [α7-nAChR] has the potential to result in protease activation, increased pro-inflammatory signaling and cell death. Memantine has the capacity to mitigate these effects with the potential to provide an approach to the prevention and treatment of
COVID-19.
Besides blocking NMDA receptors, memantine is also a potent
inhibitor of α7-nACHR which is important in the regulation of
inflammation and possibly in inducing the inflammatory response,
including NETs, which are released in excessive amounts in severe
cases of COVID-19.
As a cautionary note, considering the possible nicotinic
relationship of COVID-19, medicines which inhibit the α7-nAChR,
such as memantine, could in theory worsen or propagate cytokine
storm and have deleterious effects on treatment of COVID-19. This
issue requires further investigation.
Tilorone, a known interferon inducer and selective α7-nAChR
agonist could be of value in reducing inflammation through the
anti-inflammatory reflex [47], since severe inflammation or immune
system overshoot, resulting in “cytokine storm”, is a crisis event in
COVID-19. Tilorone also acts as a lysosomotrophic agent in cell
culture system of fibroblasts, increasing pH in acid compartments
of cells [48,49], so could act in multiple pathways, since it is known
to induce interferon and is a prospect as a wide spectrum antiviral
agent. Tilorone is among the 10 medicines recommended for
repurposing for COVID-19 in the CovidX Network algorithm for
drug repurposing recommendation [50,51].
Enhancing the initial innate immune response, inhibiting viral
entry, likely through clathrin- mediated endocytosis through the
plasma membrane, inhibiting viral development in the endosomal/
lysosomal system, and replication in the cytoplasm, are processes
which may be inhibited by medications. Adamantanes such as
amantadine, rimantadine and memantine could be repurposed with
the potential to interfere with some aspects of these features of viral
infection. Rimantadine was noted to have some degree of SARSCoV-
1 inhibitory effect on laboratory cell lines [9], which could
translate into an inhibitory effect on the SARS-CoV-2 as well, since
they are closely-related viruses. They may be compared with other
medications such Tilorone, which have a lysosomotrophic effect, and
even food items such as ammonium chloride (salmiak) in confections
such as liquorices with up to 7.99% food grade ammonium chloride
enjoyed on a daily basis, primarily in the Nordic countries, which appear to have a reduced death rate for COVID-19 [20]. Controlled
clinical trials to further evaluate these interesting observations are
now urgently required in order to confirm and amplify the evidence
base in favour of the value of repurposing of adamantanes for the
prevention and treatment of COVID-19.