Journal of Pharmaceutics & Pharmacology
Download PDF
Review Article
Current Medication Trendsand Global Impact on Neurodegenerative Disorders
Harikesh Maurya* and Sudhir Kumar
- Department of Pharmacology, Hygia Institute of Pharmaceutical Education and Research, Lucknow, India
*Address for Correspondence: Harikesh Maurya, Department of Pharmacology, Hygia Institute of Pharmaceutical Education and Research, Lucknow, India, Email: mauryaharikesh2@gmail.com
Citation: Maurya H, Kumar S. Current Medication Trends and Global Impact on Neurodegenerative Disorders. J Pharmaceu Pharmacol. 2018; 6(1): 9.
Copyright: © 2018 Maurya H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Pharmaceutics & Pharmacology | ISSN: 2327-204X | Volume: 6, Issue: 1
Submission: 30 July, 2018| Accepted: 03 September, 2018 | Published: 12 September, 2018
Abstract
Neurodegenerative disorders are the medical condition characterized by destruction in neuronal cells, abruption of neuronal activity and distinct involvement of the functional movement. The main neuronal disorders like Parkinson and Alzheimer disease are caused by environmental and genetic influences associated with accumulation of abnormal protein aggregation, which leads to inflammation as well as oxidative stress in the central nervous system. The AYUSH medication system considerably accepted by health-care professionals played a critical role since a decade to manage the elevated factors and continuously improving lifestyle for good survival of the patients. In which allopathic and ayurvedic medications have been precisely introduced for the management of disorders and regain of neuronal function. Unani and Siddha medicines have been widely used since ancient time and found as significantly reliving the sign and symptoms of neurodegenerative disorders, while yoga plays a perfect role for the management of these disorders. Regular yoga practice may relax the mind and calms the brain; reduces headache, fatigue and cures insomnia; increases blood circulation and maintain proper supply of oxygen to the lungs and detoxifies the internal organs. Thus, yoga plays a promising role in the improvement of mental health, releases stress, fatigue, depression and tension and also stimulating blood circulation in the brain. Finally it was concluded that, the AYUSH medication system ighly accepted for reliving the neuronal complications and managing all elevated parameters in patients suffering from neuronal disorders.
Keywords
Neurodegenerative disorders; Parkinson; Alzheimer; Depression; AYUSH medication system
Abbreviations
AD: Alzheimer’s Disease; AChE: Acetyl Cholinesterase; ALS: Amyotrophic Lateral Sclerosis; ATP: Adenosine Triphosphate; AYUSH: Ayurveda Yoga Unani Siddha Homoeopathy; BChE: Butyrylcholinesterase; BBB: Blood Brain Barrier; CNS: Central Nervous System; NDDs: Neurodegeneration Disorders; PD: Parkinson’s Disease; HD: Huntington’s Disease; MS: Multiple Sclerosis; RRMS: Relapsing Remitting Multiple Sclerosis; SPMS: Secondary Progressive Multiple Sclerosis; PPMR: Primary Progressive Multiple Sclerosis; PRMS: Progressive Relapsing Multiple Sclerosis; ROS: Reactive Oxidative Stress; TCA: Tricarboxylic Acid; ETC: Electron Transport Chain; NMDA: N-Methyl-D-Aspartate; MAOB: Monoamine Oxidase B; NSAID: Non Steroidal Anti-inflammatory Drug; MRI: Magnetic Resonance Imaging
Introduction
Neurodegenerative diseases are the brain disorders with selective loss of neuronal activity, degeneration of neuronal cells and distinct involvement of the functional systems as defined in clinical presentation [1]. The most common disorders of nervous system caused by environmental and genetic influences are Parkinson’s disease and Alzheimer’s disease, which have been recognized by accumulation of abnormal protein aggregate leads to inflammation and oxidative stress in the central nervous system [2,3]. The biological mechanisms associated with neurodegenerative disorders are oxidative stress, aggregates of proteins in neurons, depletion or inadequate synthesis of neurotransmitters, degradation of neurotransmitters in the synaptic cleft due to the higher activity of enzymes, abnormal ubiquitination, mitochondrial dysfunction, and excitotoxicity of neurons as well as disarrangement or damages of the Blood Brain Barrier (BBB) [4]. The human ailments associated with neurodegenerative disorders are given as follows;
Alzheimer’s disease
One of the most common neurodegenerative disorders is Alzheimer’s disease (AD), which shows loss of memory, alterations in mood and behavior, often accompany most frequent cause of dementia, disorientation and aphasia. The hippocampus and cerebral cortex are preferentially and severely affected in AD [5]. Pathologically, senile or neuritic plaques (composed of amyloid-β with peptide aggregates) and neurofibrillary tangles (filamentous bundles comprised of hyper phosphorylated tau proteins) are the main characteristic lesions in affected tissues. Tau protein is normally involved in nutrient transport along neuronal axons [6]. The prevalence of AD in the people age of ≥85 years is about 30% and the incidence rates rising upon 6-8% per year. It was also observed that the onset is rarely raises about 0.5% per year for the age group of 55-70 year population; except in familial cases, which comprises roughly 5-10% [7].
Parkinson’s disease
The second most common neurodegenerative disorders is Parkinson’s disease (PD), associated with movement disorder like tremors, rigidity, bradykinesia and postural instability in both rest as well as working situations [8]. The mechanisms involved in PD are loss of dopamine-producing neurons of the mid-brain substantia nigra, abnormal protein aggregation with deficient clearance of aggregates, impaired mitochondrial function, oxidative stress, inflammation, bnecrosis and accelerated apoptosis [9]. Other pathologic condition like intracellular deposits of aggregated i.e. α synuclein, ubiquitin have found in many surviving neuronal populations [10,11]. The prevalence of PD may reach 2% in persons aged ≥65 years whichrelatively rare with age ≤50 years and rise sharply throughoutthe eighth decade of life. The epidemiologic surveys, mainly in western countries, indicate a small (20-30%) excess risk in men. Theworldwide annual surveys reported the incidence rates of 0.01-0.05%in most countries [12].
Huntington’s diseases
Huntington disease (HD) is a typical neurodegenerative disorder of the CNS distinguished by surplus choreatic movements, dementia, behavioral, emotional and psychiatric disturbances [13,14]. Symptoms usually begin between the ages of 35-50 years, although the onset may occur at any time from childhood to old age. Death may occur an average of 15-20 years after appearance of first symptoms, while some patients dying earlier surviving for 30-40 years, due to falls or developed suicidal tendency [15].
Amyotrophic lateral sclerosis
Is a disease of the motor neurons in the cerebral cortex and the anterior horns of the spinal cord. ALS is generally a rapid fatal condition within 2-3 years of onset usually occurs in the middlelater years of life. The major pathogenic mechanism in the neuronal death is considered to be excitotoxicity mediated by glutamate and elevated calcium ion [16]. As a consequence of neuronal cell death, neuronal muscle atrophy occurs, resulting in diminished muscle strength in bulk, fasciculation’s, and hyper-reflexia. Effects on respiratory muscles can lead to pulmonary infection, and eventually amyotrophy leads to paralysis and death [17]. The incidence is very rare approximately 0.001-0.002% per year, and appears to be slightly more common in men, while with the familial ALS accounting for about 10% of whole cases [18].
Multiple sclerosis
MS is an autoimmune and inflammatory demyelinating disease of the central nervous system, affecting 0.03-0.6% of population. As per National Multiple Sclerosis Society, around 2.1 million people affected worldwide [19].Relapsing-Remitting MS (RRMS): This is the most common form of multiple sclerosis. Around 85% people suffered withMS are initially diagnosed with RRMS. The RRMS suffered people with temporary periods called relapses, flare-up or exacerbations, when new symptoms appear [20]. Secondary-Progressive MS (SPMS): When the conditions worsen more steadily over time, with or without occurrenceof relapses and remissions known as SPMS. Most people who are diagnosed with RRMS will have transition to SPMS at some point [21]. Primary-Progressive MS (PPMS): It is uncommon but the incidence is about 10% of people with MS and characterized by slowly worsening symptoms from the beginning with no remissions [20]. Progressive-Relapsing MS (PRMS): It is a rare form of MS only 5% people fall in this category with acute relapses without remissions, and characterized by a steadily worsening disease state from the beginning with or without recovery [20]. Alzheimer: Incidence in India is 1.6 millions, while global incidence is 24 millions; Parkinsonism: Incidence in India is 7-8 millions, while global incidence is 7-10 millions; Dementia: Incidence in India is 4 millions, while global incidence is 50 millions
There are four types of multiple sclerosis are described as follows:
Current Scenario of the human population suffered by neurodegenerative disorders in India and worldwide as per global survey report (UN news center, The Times of India news on WorldAlzheimer’s day and Parkinson’s news today detained in 2017) aregiven as follows;
Symptomes
The symptoms shown in neurodegeneration diseases are loss of memory, bradykinesia, muscular rigidity, rest tremor, postural & pace impairment [22]. Olfactory dysfunction, cognitive impairment, psychiatric symptoms, sleeps disorders, autonomic dysfunction, pain, and fatigue [23,24]. Other symptoms like constipation, depression, mood disorders are the characteristic of this premotor or prodromal phase of the disease [25].
Pathophysiology
The common pathological features of the neurodegenerative disorders are aggregation of mutated or misfolded proteins, gliosis, atrophy and neuronal cell loss. In AD, neuronal cell death is associated with the deposition of extracellular amyloid plaques, consisting of amyloid β peptides and intracellular neurofibrillary tangles. In PD, loss of dopaminergic neurons within the substantia nigra with associated lewy bodies, cytoplasmic aggregates made up predominantly of alpha-synuclein. In HD, predominant atrophyof the striatum, cortex and caudate is particularly affected with significant loss of medium spiny neurons but fewer loss of glial cells.In ALS, neuronal cell death preceded by cellular shrinkage, axonalswelling and mutations in the gene superoxide dismutase involved inthe regulation of free radical formation.
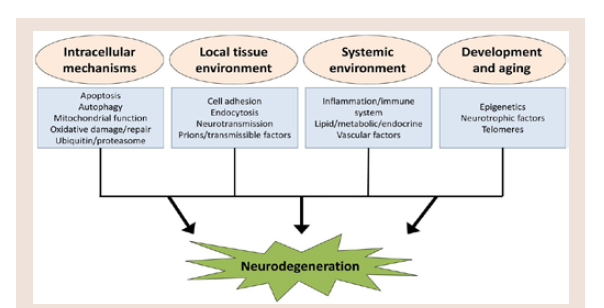
Although the proteins affected in AD, PD, HD, and ALS are different, there are several common mechanisms, including the formation of oligomeric protein aggregates and increased oxidativestress, ultimately lead to neuronal cell death. The pathways and overarching functional groups in this model are highly related and canhave overlapping or interacting components which can collectivelymodulate neurodegenerative processes (Figure 1) [26,27].
Etiology
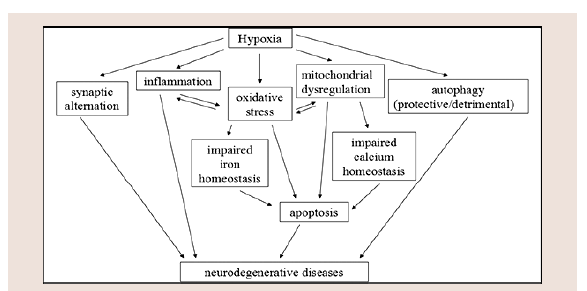
Neurodegenerative disorders are characterized by progressive dysfunction of specific characteristic of neurons and neuronal defeats associated with extra and intra cellular accumulation of misfolded proteins. The main critical processes for abnormal protein dynamics is due to the deficiency of ubiquitin-proteosome-autophagy system, oxidative stress, free radical formation, mitochondrial dysfunction and impaired bioenergetics (Figure 2). The second most process involves in dysfunction of neurotrophins is neuronal inflammation which disrupts the neuronal Golgi apparatus and axonal transport [28].
The interrelated mechanisms leads to programmed cell death are explained as follow;
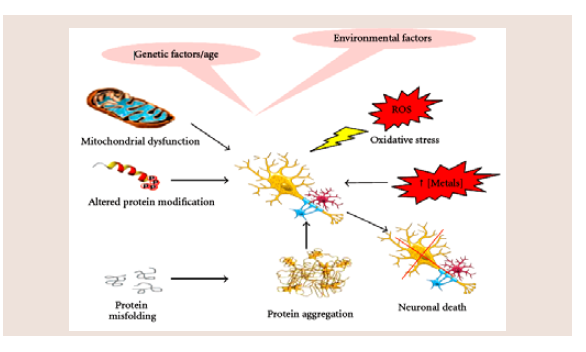
1. Protein aggregation: It plays a variety of pathological characteristic involve in neurodegenerative disorders due to abnormal interactions between intra and extra cellular deposition of self-aggregating misfolded proteins with formation of high-ordered insoluble fibrils [29-34]. The basic neurodegenerative process is the formation of several gene-gene complex and gene-environmental interaction with mutation in the genes encoding protein constituents [35]. Whereas the disintegration of neuronal networks depend on dysfunction and death of neuronal as well as glial cells, which caused by abnormal protein-protein interactions with its lesion that result from the production of vicious circles (Figure 3) [36,37].Abnormal interaction between normal, highly soluble brain proteins alters their characteristics, properties and misfolding gradually converts them into insoluble polymers with the aggregates adopting either highly ordered (cross-pleated sheet structures) or disordered (amorphous) forms [38-40].
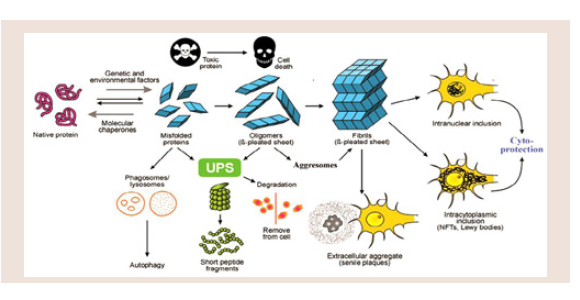
2. Protein misfolding: Protein aggregation resemblin inappropriate folding or misfolding protein leads to structural and functional changes of a normal protein, inducing the formation of protein aggregates through different supramolecular organizations (Figure 4). Abnormal proteins resulting the production errors inherited or acquired amino acid substitutions often cannot fold correctly and will be trapped in misfolded conformations. The pathogenic pathways involve membrane permeabilization through a channel mechanism or hydrophobic interaction of prefibrillary oligomers with different cellular targets [41,42].
Figure 4: Model of protein misfolding and fibrillation leading to deposition of aggregated proteins in cells and extracellular spaces via actions of the UPS, phagosomes and aggresomes, either causing cell death or cytoprotection.
3. Mitochondrial dysfunction and ROS: Mitochondrial dysfunction and oxidative stress play an important role for the development of more common neurodegenerative disorders. The loss of mitochondrial function is associated with an increase in the production of reactive oxygen intermediates and a number of human diseases [43]. Mitochondria use metabolic intermediates generated during the Tricarboxylic Acid (TCA) cycle to produce Adenosine Triphosphate (ATP) during oxidative phosphorylation. Electrons are occasionally captured by oxygen to produce superoxide anion radicals (O-2) during the ETC (electron transport chain). These superoxide radicals are converted in to hydrogen peroxide in the mitochondria through the action of manganese superoxide dismutase. In the mitochondria hydrogen peroxide is broken down to water by the action of glutathione peroxidase or peroxiredoxins. The inhibition of ETC proteins can cause a subsequent increase in ROS resulting in decrease in the mitochondrial membrane potential, loss of ATP, energy collapse and subsequent cell death [44,45].
Diagnosis
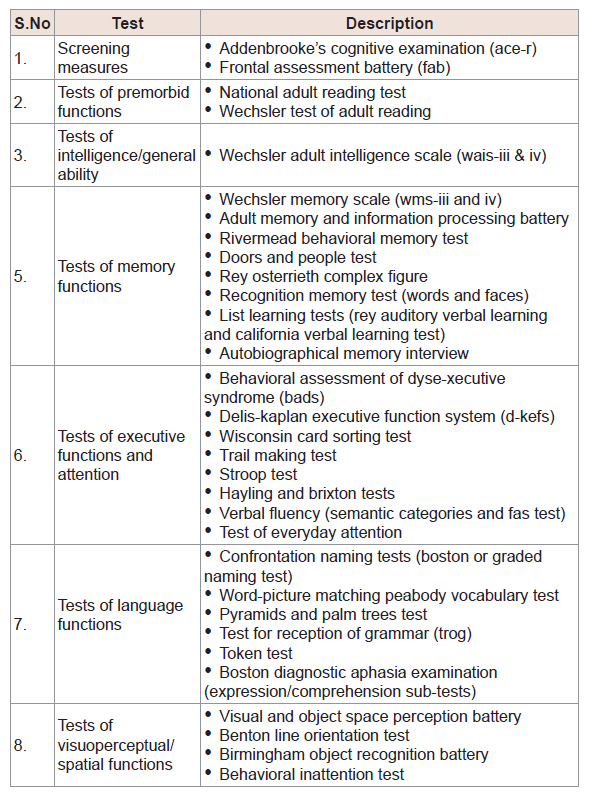
The different types of neuropsychological diagnostic tests are commonly used in clinical evaluation of brain disorders described in (Table 1) [46].
Treatment of neurodegeneration
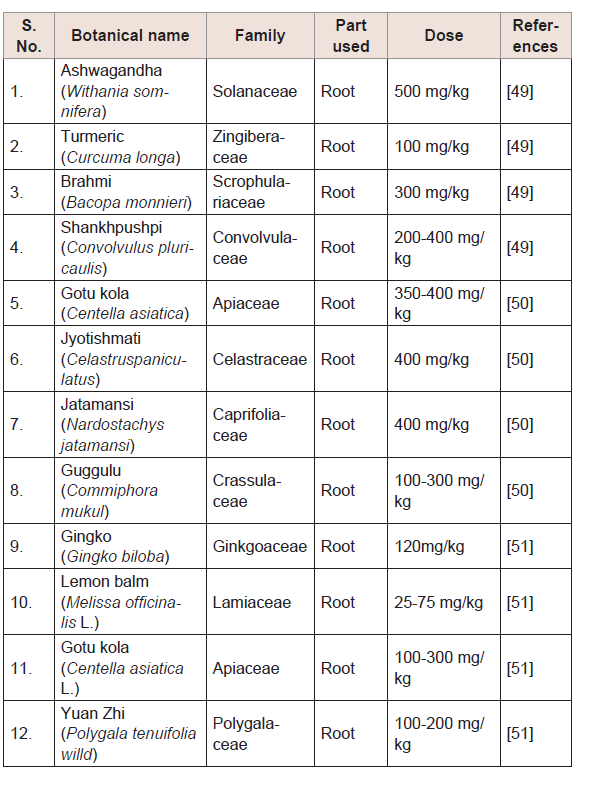
Management through ‘AYUSH’ medication system: The treatment goals for the management of neurodegenerative diseases are to first relieve the symptoms, prevent complications, and interruption with neurons destruction. To control neurodegenerative diseases, must treat the symptoms that disturbing the neuronal functions. Currently a novelistic medication system such as Allopath, Yoga (naturopathy), Unani, Siddha and Herbals (AYUSH) is considered cumulative therapies for the complete prevention of neurodegeneration [47]. This alternative medication system consist of currently available treatment incorporated with medicinal plants possessing active chemical constituent and other systems traditionally used as folker medicine that developed over generations within various societies before the era of modern medicine (Table 2) [48-51].
Table 2:List of selected Ayurvedic (herbal) medicines for the treatment of NDDs [49-51]
Yoga system of management
Yoga is antique traditional sciences which encompass yogistic physical postures (asanas), yogistic breathing practices (pranayama), meditations and relaxation techniques, highly accepted as science rather than religion or philosophy [52]. Yoga considers individual existence in five dimensions and not merely physical. These five dimensions are annamaya kosha (physical body), pranamaya kosha (vital body), manomaya kosha (Psychic body), vijanamaya kosha (intellectual body) and Anandamaya kosha (causal body) [53]. Over a short period of time, non-communicable diseases are the result of an imbalance that starts at manomaya kosha level and percolates down to the annamaya kosha level via pranamaya kosha. Therefore, yogatherapy focuses on bringing balance by all these levels of existence through a variety of techniques [54]. The components such as asanas work at the physical level; pranayama works at a vital energy level, and meditation works at psychological and intellectual levels.
The asanas are referred as poses in yoga. These particular postures help in improving the blood circulation to the vital organs like brain and prevent various types of illness to the human body. In which meditation is the most important facts about yoga and controlled breathing helps in better functioning of the brain. Researchers have observed that 20 minutes of yoga a day will improve speed and accuracy of working memory. Yoga benefits on brain are immense and the following asanas practiced on a daily basis will help in proper functioning of the brain [55].
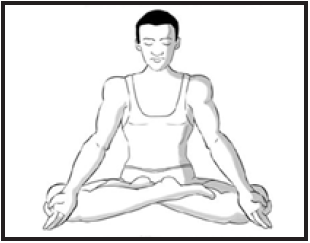
- Padmasana (Lotus pose)
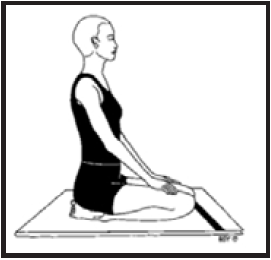
- Vajrasana (Diamond pose)
- Ardha Matsyendrasana (Half spinal twist pose)
- Paschtimottanasana (Seated forward bend)
- Halasana (Plow pose)
- Mayurasana (Peacock pose)
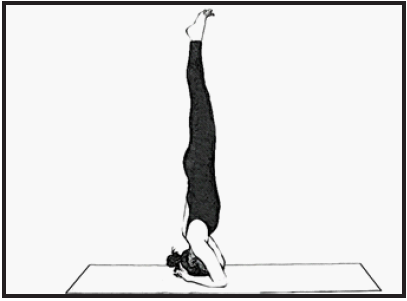
- Sirsasana (Headstand pose)
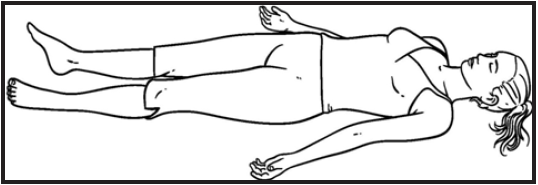
- Shavasana (Corpse pose)
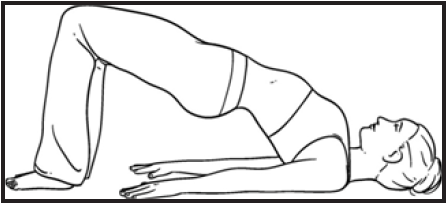
- Sarvangasana (Bridge-bandha pose)
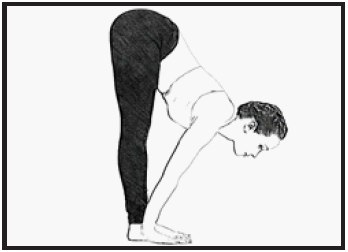
- Uttanasana (Standing forward bend)
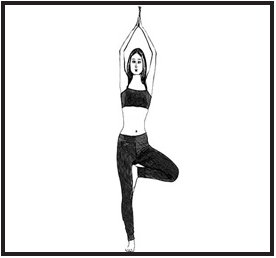
- Vrikshasana (Tree pose)
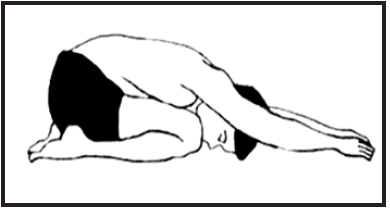
- Shashankasana (Hare pose)
Padmasana: Lotus is considered as a symbol of purity, enlightenment and detachment. Padmasana (lotus pose) is a meditative pose that works best when done in the morning with or without an empty stomach. Hold this intermediate level Hatha-Yoga pose (Padmasana) for at least 1-5 minutes [56].
Benefits:Padmasana relaxes the mind and calms the brain; awakens the chakras in the body and increases consciousness.
Vajrasana:Diamond pose is a kneeling exercise, usually accompanied by breathing aerobics. Practicing the Vajrasana facilitates the body to develop into as strong as a diamond. Only Vajrasana have to be practiced after a meal for at least 5-10 minutes disparate other yogasanas.
Benefits:Vajrasana aids proper digestion and with regular practice it eliminates constipation and combats acidity. The pose helps the body to relax and increases blood circulation and also improves the flexibility of the lower body and tones the muscles.
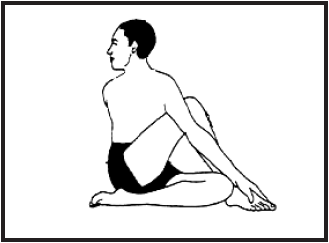
Ardha Matsyendrasana: The half lord of the fishes pose is named after the sage Matsyendranath i.e. half spinal twist with numerous variations. Practice this asana either early in the morning on an empty stomach or 4-6 hours after a meal in the evening for at least 30-60 seconds.
Source: https://i.pinimg.com/736x/d8/20/d3/d820d32f42443e1760d4ac96a7dabff9--yoga-for-beginners-twist.jpg
Benefits: Ardha Matsyendrasana relieves stiffness in the back and improves digestion. This pose increases the supply of oxygen to the lungs and detoxifies the internal organs and also purifies the blood which improves its circulation.
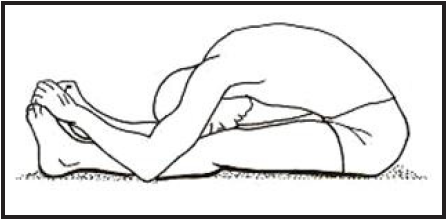
Paschtimottanasana: The Seated forward bend is a classic Hatha- Yoga pose and very simple in performing Paschtimottanasana. This asana gives the body a good stretch and concentrates on the back.Practice this pose in the morning on an empty stomach and clean bowels, also do it in the evening after 4-6 hours from the last meal. During practice, hold this basic Hatha-Yoga pose for 30-60 seconds.
Benefits:Paschtimottanasana relieves mild depression and stress, gives a good stretch to shoulders, and activates the neurons. This asana reduces headache, fatigue; cures insomnia and maintain high blood pressure.
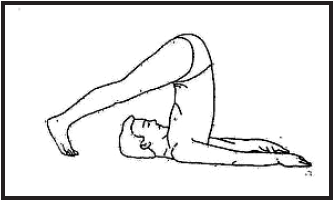
Halasana:The Plow pose uncovers the hidden capabilities of the body. The plow is a farming instrument used in many Asian countries that churns the soil in preparation for sowing seeds. Practice the pose in the morning on an empty stomach or in the evening with a gap of 4-6 hours from the last meal and hold the pose for 30-60 seconds during practice.
Source: http://4.bp.blogspot.com/-Q5MPUF0J6hY/Ux3Xr0HIKSI/AAAAAAAAAwk/1z1cn5Z1hRs/s1600/Halasana.jpg
Benefits:This pose releases the strain in the back and enhances the posture to reduce stress and calms the brain.
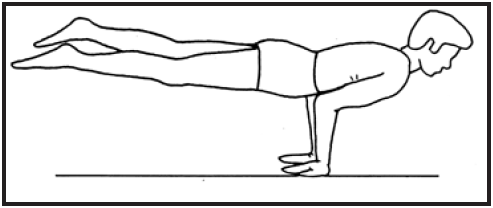
Mayurasana:The Peacock pose resembles a peacock when it walks around with its feathers down. It is best to practice this pose in the morning on an empty stomach as the body has the energy generated from digesting the meal of the previous night and hold this pose for 30-60 seconds during practice.
Benefits:Mayurasana improves concentration and coordination between the mind and the body.
Sirsasana: The headstand is the king of all yoga poses. It requires complete inversion of the body and good upper body strength. Sirsasana needs a series of preparatory exercises over a period to do the asana. At some stage in practicing this asana. It is necessary that the stomach is empty and bowels clean to. Better try to hold the pose for at least 1-5 minutes.
Benefits:Sirsasana instantly calms the body and also stimulates the pituitary gland, strengthens the lungs, improves digestion, cures asthma etc. It stimulates excess blood flow to the brain which reduces the stress and recovers neuronal activity.
Shavasana:The ‘corpse’ pose look like relaxed sleeping pose. It is very simple and everyone can do this asana with lots of concentration on each part of the body. Better try to practice this asana for at least 10-15 minutes [57].
Benefits:Shavasana relaxes the whole body, which beneficial in patient suffering from neurological problem, releases stress, fatigue, depression and tension. It develops excellent concentration, cures insomnia, calms the mind; improve mental health and also stimulating blood circulation in the brain.
Sarvangasana:The Bridge yoga pose is a great front hip joints opener, which strengthens spine, opens the chest, and improves spinal flexibility in addition to stimulating the thyroid. The practice become excellent while the stomach is empty with clean bowels and better tries to hold the pose for at least 2-5 minutes [59].
Benefits:It helps to alleviate stress and mild depression, provide calms to the brain and central nervous system. It also reduces headache, fatigue, anxiety and insomnia [59].
Uttanasana:This type of asana for brain requires standing straight, then bending and placing the hands outside feet, keeping the back and kneeing straight. This is better in the morning; if not possible practice it in the evening after 4-6 hours from the last meal and hold this pose for at least 2-5 minutes [60].
Benefits:It helps in release stress, anxiety, depression, and fatigue; provides calm to the mind and soothes the nerves. Relieves tension in the spine, neck, and back activates the abdominal muscles and also reduced symptoms of headaches, insomnia etc. [60].
Vrikshasana:This yoga ensures benefit to the brain; stand straight and bend the right leg so that it is placed on the left thigh with its toes downwards. Raise the hands above to head as in the prayer position. Better try to practice this asana for at least 2-5 minutes [61].
Benefits:It gives tranquility to the mind thus good for those who are facing the problem of depression and anxiety. It increases stamina, concentration, immunity and develops esteem and self-confidence. It calms and relaxes the central nervous system and stretches the entire body from toes to fingers.
Shashankasana:This is one of the excellent yoga asana for brain; in this horse pose start with sitting on the heels put back and neck straight. Bend the body over the thighs so that the forehead will touch the mat. [62]
Benefits:It produces calm, relaxed of mind and increasing the memory power if practice this asana regularly [62].
Unani medication system
In Unani system of medicine, the uses of natural sources are continued at an appropriate quantity for influencing the properties of medicine (Table 3). The common differences of unani medication system surrounded by other medication system are drugs name, doses, prescription pattern and uses in comparison to Ayurveda & Siddha medication systems [63].
Table 3:List of appropriate Unani medicines used for the treatment of NDDs [64]
Siddha medication system
It is one of the oldest medication systems of south India, where the use of herbal medicines is arranged for the alleviation of any type of ailments in human being (Table 4). Currently, this medication system proves a rapid improvement over meticulous disease with negligible side effects.
Table 4:List of appropriate Siddha medicines used for the treatment of NDDs [65]
Allopathic medication system
It is one of the most advanced systems of medical practice with modern medicine, which takes care of a disease using chemicals, produces different effects during treatment. Some appropriate and common medicines or chemical agents who exploit to resolve these complications are given in (Table 5).
Table 5:List of Allopathic medicines used for the treatment of NDDs [66-68].
Discussion
The special collection showcase of this review article facilitates the impact on understanding the mechanisms of neurodegenerative disorders. The present article spans different diseases, from commonest disorders such as Parkinson’s and Alzheimer’s disease to rare neurological disorders. AYUSH system is a reputed medication system for its various pharmacological effects favorable for human health [69]. Besides the potent neuroprotective potential, a number of studies described the significant therapeutic effect of the herbal plant against numerous CNS disorders. Biological effects of herbal plants have been generally attributed to the major protective effect science ancient time. The neuroprotective effect of the plant has been suggested from the findings that have dissimilar mechanisms, most of which have referred to positive influences on oxidative stress and other assessment parameters [70]. The modulatory role of alternative medication processes would not only lead to the discovery of novel neuroprotective goal to treat CNS disorders but also help to understand complex pathophysiology of neurodegenerative diseases [71].
There are various allopathic drugs available in the global market used for the management of neurodegenerative disorders and might be reliable for modification in neuronal function. Meanwhile the patients have little compliance against these drugs after prolong exposures like insomnia, dinginess, confusion, loss of concentration etc. [72]. A critical diagnosis is essential for preparation of goals to care and management of neuronal patients. The current review converses the overall symptoms, pathophysiology, cellular mechanism behind it, worldwide affected population, complication in management of neurodegenerative disorders and approaches for the most excellent and preferable treatment medication systems i.e. AYUSH for the maintenance of these worsen condition in human population [73].
The researchers facing serious challenges in drug discovery process for neurodegenerative diseases, which becoming extremely expensive and critically incompetent. Approaches based on reverse pharmacology also offer efficient development proposal for newformulations based on herbal products and treatment novel goal.The Ayurvedic system of medicine with Yoga has acquired increasingrecognition in recent years with help of nutritious, standard diet andeffective treatment approaches [74].
Early development of Ayurvedic herbal supplements which prescribed from centuries for neurodegenerative diseases (including dementias) was agreed only by Western countries health care professional as mechanistic studies on AD; however, these mechanistic points of studies addressed to the same mechanisms by the Ayurvedic therapeutics (for example, increase in nerve growth factors, neurotrophic factors, reduction in inflammation and oxidative damage), providing strong support in favor of herbal therapy for NDDs. It was well known that, the authoritative basic knowledge of Ayurveda together with combinatorial sciences continuously improving the ease with Ayurvedic formulations, which can be used in drug discovery agencies and drug development process, providing new functional leads for NDDs and other age associated neurodegenerative diseases [75].
Conclusion
The various areas of study of Yoga practices were reviewed in the present article indicated physiological benefits and its effect on nervous system, immune system, circulatory system, respiratory system, digestive system and endocrine system. Improvement in antioxidant property through Yoga system are extremely utilizes in prevention of neurodegenerative disorders, cardiovascular disorders, psychosomatic disorders, analgesic effect, numerous benefits of Yoga on female population and role of Yoga on rehabilitation. Finally it was observed from the published report that the Yoga can be adopted by a large healthy and diseased population. A significant diagnostic evaluation is essential for best possible care and management of neurodegenerative patients. The current review discuss the most excellent treatment medication systems i.e. “AYUSH” for the management of neurodegenerative condition on the basis of enormous published research proposal. Furthermore peaceful investigation and prevention on neurodegenerations are requiring for management of these challenging task to improvement of patient’s life.
References
- Cornutiu G (2015) The epidemiological scale of Alzheimer’s disease. J Clin Med Res 7: 657-666.
- Aruoma OI, Bahorun T, Jen LS (2003) Neuroprotection by bioactive components in medicinal and food plant extracts. Mutat Res 544: 203-215.
- Behl C (1999) Alzheimer’s disease and oxidative stress: implications for novel therapeutic approaches. Prog Neurobiol 57: 301-323.
- Jenner P, Olanow CW (1998) Understanding cell death in Parkinson’s disease. Ann Neurol 44 (3 Suppl 1): S72-S84.
- Blennow K, de Leon MJ, Zetterberg H (2006) Alzheimer’s disease. Lancet 368: 387-403.
- Hardy J, Selkoe DJ (2002) The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297: 353-356.
- Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni, L, et al. (2005) Global prevalence of dementia: a Delphi consensus study. Lancet 366: 2112-2117.
- Samii A, Nutt JG, Ransom BR (2004) Parkinson’s disease. Lancet 363: 1783-1793.
- Dawson TM, Dawson VL (2003) Molecular pathways of neurodegeneration in Parkinson’s disease. Science 302: 819-822.
- Agid Y (1991) Parkinson’s disease: Pathophysiology. Lancet 337: 1321-1324.
- Wakabayashi K, Tanji K, Mori F, Takahashi H (2007) The Lewy body in Parkinson’s disease: molecules implicated in the formation and degradation of alpha-synuclein aggregates. Neuropathology 27: 494-506.
- Elbaz A, Bower JH, Maraganore DM, McDonnell SK, Peterson BJ, et al. (2002) Risk tables for Parkinsonism and Parkinson’s disease. J Clin Epidemiol 55: 25-31.
- Harper PS (1992) The epidemiology of Huntington’s disease. Hum Genet 89: 365-376.
- Watt D (1990) Huntington’s disease: a disorder of families. In: Folstein SE (Ed.), Johns Hopkins University Press, USA. Psychol Med 20: 728-731.
- Ross CA, Margolis RL, Rosenblatt A, Ranen NG, Becher MW, et al. (1997) Huntington disease and the related disorder, dentatorubral-pallidoluysian atrophy (DRPLA). Medicine (Baltimore) 76: 305-338.
- Sen I, Nalini A, Joshi NB, Joshi PG (2005) Cerebrospinal fluid from amyotrophic lateral sclerosis patients preferentially elevates intracellular calcium and toxicity in motor neurons via AMPA/kainate receptor. J Neurol Sci 235: 45-54.
- Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, et al. (1993) Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature 362: 59-62.
- del Aguila MA, Longstreth WT Jr, McGuire V, Koepsell TD, van Belle G (2003) Prognosis in amyotrophic lateral sclerosis: a population-based study. Neurology 60: 813-819.
- Matute-Blanch C, Montalban X, Comabella M (2017) Multiple sclerosis, and other demyelinating and autoimmune inflammatory diseases of the central nervous system. Handb Clin Neurol 146: 67-84.
- Newsome SD, Aliotta PJ, Bainbridge J, Bennett SE, Cutter G, et al. (2017) A framework of care in multiple sclerosis, Part 2: Symptomatic care and beyond. Int J MS Care 19: 42-56.
- Noyes K, Bajorska A, Chappel A, Schwid SR, Mehta LR, et al. (2011) Cost-effectiveness of disease-modifying therapy for multiple sclerosis: a population-based study. Neurology 77: 355-363.
- Gibb WR, Lees AJ (1988) The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 51: 745-752.
- Khoo TK, Yarnall AJ, Duncan GW, Coleman S, O'Brien JT, et al. (2013) The spectrum of nonmotor symptoms in early Parkinson disease. Neurology 80: 276-281.
- Postuma RB, Aarsland D, Barone P, Burn DJ, Hawkes CH, et al. (2012) Identifying prodromal Parkinson’s disease: pre-motor disorders in Parkinson’s disease. Mov Disord 27: 617-626.
- Noyce AJ, Bestwick JP, Silveira-Moriyama L, Hawkes CH, Giovannoni G, et al. (2012) Meta-analysis of early nonmotor features and risk factors for Parkinson disease. Ann Neurol 72: 893-901.
- Pal R, Larsen JP, Moller SG (2015) The potential of proteomics in understanding neurodegeneration. Int Rev Neurobiol 121: 25-58.
- Yacoubian TA (2017) Neurodegenerative disorders: why do we need new therapies?. In: Adejare A (Ed.) Drug discovery approaches for the treatment of neurodegenerative disorders Alzheimer’s disease. Elsevier, USA, pp. 1-16.
- Blennow K, de Leon MJ, Zetterberg H (2006) Alzheimer’s disease. Lancet 368: 387-403.
- Jellinger KA (2009) Recent advances in our understanding of neurodegeneration. J Neural Transm (Vienna) 116: 1111-1162.
- Skovronsky DM, Lee VM, Trojanowski JQ (2006) Neurodegenerative diseases: new concepts of pathogenesis and their therapeutic implications. Annu Rev Pathol 1: 151-170.
- Golde TE, Miller VM (2009) Proteinopathy-induced neuronal senescence: a hypothesis for brain failure in Alzheimer’s and other neurodegenerative diseases. Alzheimer’s Res Ther 1: 5.
- Uversky VN (2009) Intrinsic disorder in proteins associated with neurodegenerative diseases. Front Biosci (Landmark Ed) 14: 5188-5238.
- Herczenik E, Gebbink MF (2008) Molecular and cellular aspects of protein misfolding and disease. FASEB J 22: 2115-2133.
- Bolshette NB, Thakur KK, Bidkar AP, Trandafir C, Kumar P, et al. (2014) Protein folding and misfolding in the neurodegenerative disorders: a review. Rev Neurol (Paris) 170: 151-161.
- Migliore L, Coppede F (2009) Genetics, environmental factors and the emerging role of epigenetics in neurodegenerative diseases. Mutat Res 667: 82-97.
- Palop JJ, Chin J, Mucke L (2006) A network dysfunction perspective on neurodegenerative diseases. Nature 443: 768-773.
- Seeley WW, Crawford RK, Zhou J, Miller BL, Greicius MD (2009) Neurodegenerative diseases target large-scale human brain networks. Neuron 62: 42-52.
- Ecroyd H, Carver JA (2008) Unraveling the mysteries of protein folding and misfolding. IUBMB Life 60: 769-774.
- Lee VM, Trojanowski JQ (2006) Mechanisms of Parkinson’s disease linked to pathological alpha-synuclein: new targets for drug discovery. Neuron 52: 33-38.
- Morris AM, Watzky MA, Finke RG (2009) Protein aggregation kinetics, mechanism, and curve-fitting: a review of the literature. Biochim Biophys Acta 1794: 37
- Hartl FU, Hayer Hartl M (2009) Converging concepts of protein folding in vitro and in vivo. Nat Struct Mol Biol 16: 574-581.
- Jellinger KA (2010) Basic mechanisms of neurodegeneration: a critical update. J Cell Mol Med 14: 457-487.
- Van Houten B, Woshner V, Santos JH (2006) Role of mitochondrial DNA in toxic responses to oxidative stress. DNA Repair (Amst) 5: 145-152.
- Mandavilli BS, Boldogh I, Van Houten B (2005) 3-nitropropionic acid-induced hydrogen peroxide, mitochondrial DNA damage, and cell death are attenuated by Bcl-2 over expression in PC12 cells. Brain Res Mol Brain Res 133: 215-223.
- Santos JH, Hunakova L, Chen Y, Bortner C, Van Houten B (2003) Cell sorting experiments link persistent mitochondrial DNA damage with loss of mitochondrial membrane potential and apoptotic cell death. J Biol Chem 278: 1728-1734.
- Bokde AL, Meaney JF, Sheehy NP, Reilly RB, Abrahams S (2011) Advances in diagnostics for neurodegenerative disorders. In: Hardiman O, Doherty CP (Eds) Neurodegenerative disorders: a clinical guide. Springer, UK, pp. 17-42.
- Khakurel S, Agrawal RK, Hada R (2015) Pattern of glomerular disease in Nepal: a single-center experience. Saudi J Kidney Dis Transplant 26: 833-838.
- Shrivastava SR, Shrivastava PS, Ramasamy J (2015) Mainstreaming of Ayurveda, Yoga, Naturopathy, Unani, Siddha, and Homeopathy with the health care delivery system in India. J Tradit Complement Med 5: 116-118.
- Rao RV, Descamps O, John V, Bredesen DE (2012) Ayurvedic medicinal plants for Alzheimer’s disease: a review. Alzheimers Res Ther 4: 22.
- Rasool M, Malik A, Qureshi MS, Manan A, Pushparaj PN, et al. (2014) Recent updates in the treatment of neurodegenerative disorders using natural compounds. Evid Based Complement Altern Med 2014: 979730.
- Sun ZK, Yang HQ, Chen SD (2013) Traditional Chinese medicine: a promising candidate for the treatment of Alzheimer’s disease. Transl Neurodegener 2: 6.
- Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP (2012) Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses 78: 571-579.
- Berger BG, Owen DR (1988) Stress reduction and mood enhancement in four exercise modes: swimming, body conditioning, hatha yoga and fencing. Res Q Exerc Sport 59: 148-159.
- Innes KE, Bourguignon C, Taylor AG (2005) Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. J Am Board Family Pract 18: 491-519.
- Asha (2014) 12 Yoga asanas for your brain.
- Achanta R (2018) Effective yoga poses to increase your brain power.
- (2014) Shavasana, Savasana yoga (Corpse pose) benefits and steps.
- Nayyar N (2016) Counting health benefits of Setu Bandha Sarvangasana.
- Asha (2014) 12 Yoga asanas for your brain.
- Cynha (2011) The health benefits of Uttanasana (standing forward bend pose).
- Tree pose -Vrikshasana.
- Sitham P. The procedure and benefits of Shashankasana yoga asanas.
- Siddiqui MS, Usmanghani K (2014) Acute kidney injury: treatment with unani medicine-case report. Chin Med 5: 118-122.
- Iqbal MN, Ansari AA, Khan KZ (2012) Approaches for the treatment of Alzheimer’s disease in Unani medicine: a review. J Integr Community Health 1: 25-30.
- Chitra B, Ramaswamy RS (2015) An overview on the role of siddha practices in the prevention and management of age related neurodegenerative disorders with special reference to senile dementia. Indo Am J Pharm Res 5: 1510-1521.
- Fischer F, Matthisson M, Herrling P (2004) List of drugs in development for neurodegenerative diseases. Neurodegener Dis 1: 50-70.
- Bowirrat A, Friedland RP, Farrer L, Baldwin C, Korczyn A (2002) Genetic and environmental risk factors for Alzheimer’s disease in Israeli Arabs. J Mol Neurosci 19: 239-245.
- Chen JF, Xu K, Petzer JP, Staal R, Xu YH, et al. (2001) Neuroprotection by caffeine and A(2A) adenosine receptor inactivation in a model of Parkinson’s disease. J Neurosci 21: RC143.
- Gitler AD, Dhillon P, Shorter J (2017) Neurodegenerative disease: models, mechanisms, and a new hope. Dis Model Mech 10: 499-502.
- Orhan IE (2012) Centella asiatica (L.) urban: from traditional medicine to modern medicine with neuroprotective potential. Evid Based Complementary Altern Med 2012: 946259.
- Hassan MA, Balasubramanian R, Masoud AD, Burkan ZE, Sughir A, et al. (2014) Role of medicinal plants in neurodegenerative diseases with special emphasis to Alzheimer’s disease. Int J Phytopharmacology 5: 454-462.
- Glass CK, Saijo K, Winner B, Marchetto MC, Gage FH (2010) Mechanisms underlying inflammation in neurodegeneration. Cell 140: 918-934.
- Maurya H, Kumar T (2016) A review on comprehensive overview in the management of nephrotic disorders. J Crit Rev 3: 34-43.
- Rajoria K, Singh SK (2017) Therapeutic benefits of Raj Yoga-a review. Indian J Tradit Knowledge 16(Suppl): S88-S95.
- Singh AK, Gupta A, Mishra AK, Gupta V, Bansal P, et al. (2010) Medicinal plant for curing Alzheimer’s disease. Int J Pharma Biol Arch 1: 108-114.