Journal of Pediatrics & Child Care
Download PDF
Research Article
Clinicians’ Perspectives on the use of Amoxicillin-Clavulanic Acid for Pediatric Respiratory Infections in India Settings
Manjula S* and Krishna Kumar M
Department of Medical Services, Micro Labs Limited, Bangalore, Karnataka, India
*Address for Correspondence:Manjula S, Department of Medical Services, Micro Labs
Limited, Bangalore, Karnataka, India E-mail Id: drmanjulas@gmail.com
Submission: 20 May, 2025
Accepted: 27 June, 2025
Published: 30 June, 2025
Copyright: © 2025 Manjula S, et al. This is an open access
article distributed under the Creative Commons Attr-ibution
License, which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is
properly cited.
Keywords:Antibiotic; Respiratory Infections; Pneumonia; Otitis media;
Amoxicillin-clavulanic acid
Abstract
Objective: To investigate clinicians’ perspectives regarding
the usage of antibiotics for pediatric respiratory tract infections,
with a particular emphasis on amoxicillin and clavulanic acid use in
pneumonia and otitis media.
Methodology: The cross-sectional study employed a multiitem questionnaire to collect data from clinicians across India on their antibiotic use for pediatric patients with respiratory infections, preferences for dosage regimens, duration of treatment, and factors affecting patient compliance. Descriptive statistics were used to analyze the survey data. Categorical variables were presented as percentages to provide a clear understanding of response distributions. Results: The study included 568 clinicians, and 94% of them favored co-amoxiclav for acute otitis media in outpatient settings, while 90% preferred it for treating pediatric pneumonia. Around 36% of respondents prescribed high-dose amoxicillin (600 mg) with clavulanic acid (42.9 mg) for various infections, including respiratory, ear, sinus, urinary tract, and skin infections. Among otitis media cases, 32.75% of experts reported using amoxicillin-clavulanate in 61-80% of patients, and 30.81% prescribed the high-dose formulation to 26-50% of those with recurrent cases. A 7-day course was preferred by 47.89% of experts for recurrent otitis media. Antibiotic resistance was cited by 45.60% of clinicians as the most common complication of incomplete treatment.
Conclusion: This study highlights clinicians’ preference for amoxicillin clavulanate in treating pediatric respiratory infections, especially pneumonia and otitis media in Indian settings. The highdose formulation is commonly used for a 7-day course. Clinicians also recognize antibiotic resistance as the primary risk of incomplete treatment in children.
Methodology: The cross-sectional study employed a multiitem questionnaire to collect data from clinicians across India on their antibiotic use for pediatric patients with respiratory infections, preferences for dosage regimens, duration of treatment, and factors affecting patient compliance. Descriptive statistics were used to analyze the survey data. Categorical variables were presented as percentages to provide a clear understanding of response distributions. Results: The study included 568 clinicians, and 94% of them favored co-amoxiclav for acute otitis media in outpatient settings, while 90% preferred it for treating pediatric pneumonia. Around 36% of respondents prescribed high-dose amoxicillin (600 mg) with clavulanic acid (42.9 mg) for various infections, including respiratory, ear, sinus, urinary tract, and skin infections. Among otitis media cases, 32.75% of experts reported using amoxicillin-clavulanate in 61-80% of patients, and 30.81% prescribed the high-dose formulation to 26-50% of those with recurrent cases. A 7-day course was preferred by 47.89% of experts for recurrent otitis media. Antibiotic resistance was cited by 45.60% of clinicians as the most common complication of incomplete treatment.
Conclusion: This study highlights clinicians’ preference for amoxicillin clavulanate in treating pediatric respiratory infections, especially pneumonia and otitis media in Indian settings. The highdose formulation is commonly used for a 7-day course. Clinicians also recognize antibiotic resistance as the primary risk of incomplete treatment in children.
Introduction
Acute respiratory tract infections (RTIs) are a major cause of
childhood illness and mortality worldwide.[1]According to the
Global Burden of Disease 2019 study, the highest incidence rate is
observed in children under 5 years of age, reaching three hundred
thousand cases per 100,000 population. Beyond the typical symptoms,
upper RTIs can lead to severe complications such as pneumonia, otitis
media, glomerulonephritis, and myocarditis, significantly increasing
healthcare costs and posing a financial burden on society.[2]
Recent data indicate that acute RTIs, particularly lower respiratory
tract infections, result in nearly 1.9 million childhood deaths annually,
with approximately 20% of these deaths occurring in India.[3,4]
Acute otitis media (AOM) is the second most common childhood
illness and a leading cause of pediatric consultations, accounting for
approximately 13.6 million visits worldwide each year. The highest
incidence occurs in those aged 1 to 4 years, with 61 new cases per
100 children annually. According to the World Health Organization
(WHO), otitis media is the leading cause of hearing impairment,
affecting 42 million individuals over the age of three worldwide.[2,5]
Co-amoxiclav is primarily prescribed for the treatment of
community-acquired RTIs in routine settings. As a β-lactam antibiotic,
it exerts a bactericidal effect by inhibiting bacterial peptidoglycan cell
wall synthesis, effectively targeting both Gram-positive and Gram negative
bacteria. The addition of clavulanate, a beta-lactamase
inhibitor, enhances its efficacy against resistant strains.[6]With its
potent antibacterial activity and favorable pharmacokinetic and
pharmacodynamic profile, co-amoxiclav is effective in treating betalactamase-
producing pathogens. It has demonstrated improved
outcomes in persistent or recurrent infections where initial antibiotic
therapy has failed. Its well-established safety profile and availability in
suspension formulations also make it a suitable choice for pediatric
patients.[7]
This study aims to explore current clinical perspectives among
Indian clinicians regarding antibiotics usage for pediatric respiratory
infections, with a focus on amoxicillin-clavulanate use in pneumonia
and otitis media. By examining practitioners’ preferences,
perceptions, and challenges in antibiotic prescribing, the survey seeks
to identify potential areas for improvement in pediatric infectious
disease management within Indian healthcare settings.
Methods
We carried out a cross-sectional study among clinicians across
various Indian healthcare settings from June 2024 to December 2024.
The study was conducted after receiving approval from Bangalore
Ethics, an Independent Ethics Committee, which was recognized
by the Indian Regulatory Authority, the Drug Controller General of
India.
An invitation was sent to leading clinicians in managing
infections in the month of March 2024 for participation in this Indian
survey. About 568 clinicians from major cities of all Indian states,
representing the geographical distribution, shared their willingness
to participate and provide necessary data. The questionnaire booklet
titled ENCORE (Experts Opinion on Complication of Incomplete
Therapy in treating respiratory tract infections) was sent to clinicians
who were interested to participate. The ENCORE study questionnaire
explored the prevalence of pneumonia and otitis media, antibiotic
preferences, dosing regimens, treatment duration, and factors
influencing antibiotic selection. Challenges related to patient
compliance and medication packaging were also evaluated. Clinicians
had the option to skip any questions they preferred not to answer.
They were instructed to complete the questionnaire independently,
without consulting their colleagues. Written informed consent was
obtained from all participants before the study commenced.
Statistical Analysis:
Descriptive statistics were used to analyze the survey data, with
categorical variables presented as percentages to illustrate response
distributions. Frequencies and percentages were calculated for each
survey item, and all tables were generated using Microsoft Excel
(version 2409, build 16.0.18025.20030).Results
The study included 568 clinicians, with nearly 40% reporting
that 11–25% of children with RTIs develop pneumonia in their
practice. Approximately 67% indicated they usually prescribe
antibiotics for 7–10 days in children with pneumonia. Most clinicians
(43.13%) considered multiple factors, including infection severity,
site, patient age, allergy history, and treatment cost when selecting
an antibiotic regimen. According to 55% of respondents, the most
common reason for incomplete antibiotic therapy in children is an
insufficient quantity of the drug in the bottle to complete the full
course. Nearly 21% identified dosing frequency as the primary reason
for missed antibiotic doses in children. Additionally, 48% of experts
reported that the most common external factor influencing antibiotic
course completion is the bottle running out before the full course is
completed.
The majority of clinicians (75.88%) reported that a larger bottle
offers multiple benefits, including a lower chance of recurrence,
reduced risk of incomplete therapy, decreased antibiotic resistance,
and lower overall treatment costs. Approximately 69% of respondents
stated that fruit flavor is the most acceptable choice in pediatric
practice. Nearly half of the experts (48.59%) reported that schoolaged
children (5–12 years) are most susceptible to incomplete coamoxiclav
therapy for RTIs. According to 42% of clinicians, taste
and palatability are the most important factors influencing antibiotic
compliance in children. Most clinicians (60.39%) preferred the higher
dose of 45/6.4 mg/kg/day for treating pediatric bacterial infections.
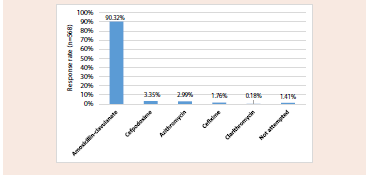
A significant majority (90.32%) preferred amoxicillin-clavulanate for
treating pediatric pneumonia [Figure 1].
The majority of clinicians (40.49%) reported that 11–20% of
children in their daily clinical practice have AOM. According to
55% of respondents, school-aged children (5–12 years) are the most
commonly affected age group for resistant otitis media in their practice.
Around 83% agreed that approximately 26% of children do not
complete their antibiotic course due to one bottle being insufficient.
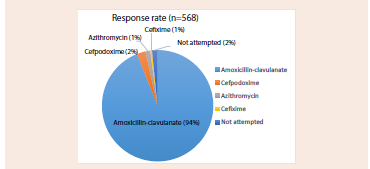
The majority of clinicians (94.01%) preferred amoxicillin-clavulanate
for treating AOM in children in the outpatient department [Figure 2].
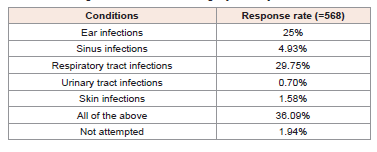
The majority of clinicians (36.09%) reported prescribing high dose
amoxicillin 600 mg and clavulanic acid 42.9 mg for all listed
conditions, including ear infections, sinus infections, RTIs, urinary
tract infections, and skin infections. Additionally, 30% of clinicians
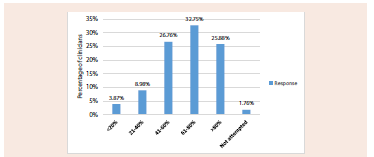
reported using it specifically for RTIs [Table 1]. Nearly 33% reported
using amoxicillin-clavulanate in 61–80% of patients with otitis media
[Figure 3].
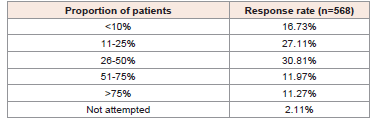
Approximately 31% of experts reported prescribing high-dose
amoxicillin 600 mg + clavulanic acid 42.9 mg to 26–50% of patients
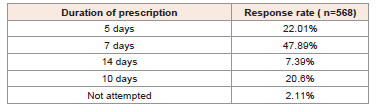
with recurrent otitis media [Table 2]. Most clinicians (47.89%)
reported prescribing this high-dose regimen for 7 days in patients
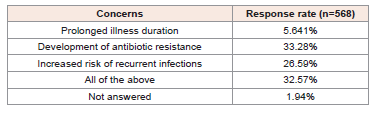
with AOM [Table 3]. The majority of clinicians (33.28%) identified
antibiotic resistance as their primary concern when treating RTIs
with incomplete antibiotic therapy in pediatric patients [Table 4].
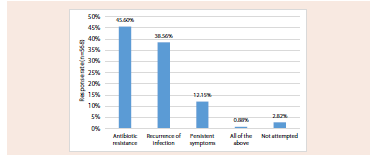
According to 46% of clinicians, antibiotic resistance is the most
common complication of incomplete antibiotic treatment in children.
About 38.5% of clinicians mentioned the recurrence of infection, and
12.15% of them highlighted the persistence of symptoms [Figure 4].
Figure 3:Distribution of responses to the proportion of patients receiving
amoxicillin-clavulanate for otitis media management
Figure 4:Distribution of responses to the most common complication of
incomplete antibiotic treatment in children
Table 1:Distribution of responses to conditions for prescribing high-dose
amoxicillin 600 mg and clavulanic acid 42.9 mg in pediatric patients
Table 2: Distribution of responses to the proportion of patients with recurrent otitis
media prescribed high-dose amoxicillin 600 mg + clavulanic acid 42.9 mg
Table 3:Distribution of responses to duration of high-dose amoxicillin 600 mg +
clavulanic acid 42.9 mg in recurrent otitis media
Discussion
The study provides valuable insights into the current practices
and perceptions of Indian clinicians regarding antibiotic prescription
patterns for pediatric respiratory infections, with particular emphasis
on amoxicillin-clavulanate use in pneumonia and otitis media. The
findings highlight several key aspects of clinical practice and identify
important challenges in ensuring optimal antibiotic therapy for
children.
The current study highlighted clinicians’ preference for
amoxicillin-clavulanate in India for pneumonia treatment, supported
by its long-standing use and inclusion in national and international
CAP guidelines. Studies report its high efficacy against Streptococcus
pneumoniae and Haemophilus influenzae, with susceptibility rates
exceeding 90%.[8] A South India-based study by Moinuddin et al.
found amoxicillin-clavulanate to be the most prescribed antibiotic
for pediatric pneumonia (43.8%), with 53% of prescriptions in
consolidation cases. Indian pediatric guidelines recommend betalactams
for non-severe pneumonia and beta-lactamase inhibitors
(e.g., amoxicillin-clavulanate) for severe cases.[9] Similarly, an
Assam-based study reported that amoxicillin-clavulanate was the
most frequently prescribed antibiotic overall (35% of total antibiotics).
Among pneumonia patients specifically, 17 out of 31 prescriptions
(55%) involved amoxicillin-clavulanate, reinforcing its role as the
preferred antibiotic for this condition.[10]
In the present study, amoxicillin-clavulanate was the preferred
choice for treating AOM in pediatric outpatients (94.01%), with
most clinicians reporting its use in 61-80% of their patients. Chu
et al. demonstrated that high-dose amoxicillin with clavulanate,
as recommended by clinical guidelines, is more effective than
conventional doses in children under 20 kg with bilateral disease.
[11] Dagan et al. further highlighted that high-dose amoxicillin clavulanate
(90/6.4 mg/kg/day) effectively treats pediatric AOM,
particularly in children under 24 months and those with penicillin resistant
Streptococcus pneumoniae.[12] Additionally, a randomized
controlled trial by Marchant et al. found amoxicillin-clavulanate to
be more effective than cefaclor for AOM treatment.[13] Another
study demonstrated that amoxicillin-clavulanate showed superior
clinical and bacteriological effectiveness compared to azithromycin
in children with bacterial AOM, including cases caused by penicillin resistant
Streptococcus pneumonia and beta-lactamase-positive
Haemophilus influenzae.[14]
For recurrent otitis media cases, the majority of the current
clinicians prescribed the high-dose formulation amoxicillin clavulanate
to 26-50% of their patients, typically for a 7-day course.
Similarly, an Italian intersociety Consensus study recommended
amoxicillin-clavulanate for 7–10 days as the preferred treatment
option for recurrent otitis media.[15] This duration aligns with
evolving evidence suggesting that shorter, appropriate-dose antibiotic
courses may be as effective as longer ones while potentially reducing
adverse effects and resistance development.[16]
The high-dose formulation (amoxicillin 600 mg with clavulanic
acid 42.9 mg) was particularly favored, with the majority of study
clinicians reporting its use across multiple conditions, including ear,
sinus, respiratory tract, urinary tract, and skin infections. Twice-daily
administration of amoxicillin at a dose of 600 mg and clavulanic acid
at 42.9 mg per 5 mL appears appropriate for achieving favorable
tolerability and efficacy in treating bacterial infections in children
under three months of age.[17] Lahiry et al. reported that a high
dose of 600 mg amoxicillin plus 42.9 mg clavulanic acid is effective in
treating pediatric bacterial infections.[18]
Antibiotic resistance is a major public health concern,
contributing to high mortality rates among children and newborns.
[19] In the present survey, respondents demonstrated awareness
of antibiotic resistance concerns, with the majority identifying
it as the most common complication of incomplete antibiotic
treatment in children. Furthermore, the majority of them cited the
development of antibiotic resistance as their primary concern when
treating respiratory infections with incomplete antibiotic therapy.
This awareness reflects growing global concern about antimicrobial
resistance and its implications for future treatment efficacy.
The study provides valuable insights into current antibiotic
prescription patterns among Indian clinicians for pediatric
respiratory infections. The findings underscore clinicians’ awareness
of antibiotic resistance as a critical concern, which is essential for
antimicrobial stewardship efforts in India. This research contributes
to the understanding of real-world antibiotic use in pediatric practice
in India, potentially informing targeted interventions to optimize
prescribing patterns. A key strength of this study is the use of a well structured
and validated questionnaire to gather expert insights from
a substantial sample of clinicians. However, certain limitations must
be considered. The survey-based approach may introduce recall bias
and personal preferences that do not always align with evidence based
practice. Additionally, the sample may not fully represent the
diversity of Indian healthcare settings, and the study emphasizes
clinician preferences rather than objectively measured patient
outcomes.
Conclusion
The study underscores clinicians’ preference for amoxicillin clavulanate
in treating pediatric respiratory infections, particularly
pneumonia and otitis media, in Indian settings. The high-dose
formulation is widely favored across multiple conditions, with
treatment typically prescribed for a 7-day course. Clinicians
demonstrated awareness of antibiotic resistance as a significant
concern, emphasizing the need for continued antimicrobial
stewardship to balance effective treatment with resistance prevention.
Acknowledgement
We would like to thank all the clinicians who were actively
participating in this study.
Author contributions
Both authors have contributed equally to the development of the manuscript. Conflicts of interest disclosures: None
Disclosure of compliance with ethical principles The study was conducted after receiving approval from Bangalore Ethics, an Independent Ethics Committee, which was recognized by the Indian Regulatory Authority, Drug Controller General of India.
Both authors have contributed equally to the development of the manuscript. Conflicts of interest disclosures: None
Disclosure of compliance with ethical principles The study was conducted after receiving approval from Bangalore Ethics, an Independent Ethics Committee, which was recognized by the Indian Regulatory Authority, Drug Controller General of India.