Journal of Pediatrics & Child Care
Download PDF
Research Article
A Human Factors Approach for Event Analysis in a Pediatric Intensive Care Unit
Kanji F1, Nawathe P2 and Cohen T3*
1Clinical Research Coordinator, Cedars-Sinai Medical Center, Department of Surgery, Los Angeles, CA, USA
2Associate Professor, Pediatrics, Medical Director of Simulation, Pediatrics, Associate Director of Congenital Cardiac Intensive Care Unit, Cedars-Sinai Medical Center, Department of Pediatrics, Los Angeles, USA
3Director, Surgical Safety and Human Factors Research, Research Scientist II, and Associate Professor, Cedars-Sinai Medical Center, Department of Surgery, Los Angeles, USA
2Associate Professor, Pediatrics, Medical Director of Simulation, Pediatrics, Associate Director of Congenital Cardiac Intensive Care Unit, Cedars-Sinai Medical Center, Department of Pediatrics, Los Angeles, USA
3Director, Surgical Safety and Human Factors Research, Research Scientist II, and Associate Professor, Cedars-Sinai Medical Center, Department of Surgery, Los Angeles, USA
*Address for Correspondence: Tara Cohen, Director, Surgical Safety and Human Factors Research, Research Scientist II, and Associate Professor, Cedars-Sinai Medical Center, Department of Surgery, Los
Angeles, USA, E-mail Id: Tara.cohen@cshs.org
Submission: 24 August, 2023
Accepted: 20 September 2023
Published: 25 September 2023
Accepted: 20 September 2023
Published: 25 September 2023
Copyright: © 2023 Kanji F, et al. This is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: HFACS-Healthcare; Adverse Events; Pediatric Intensive Care; Human Factors
Abstract
Background: Medical management in the pediatric intensive care
unit involves an increased risk of adverse events and near misses due
to the complexity of the environment and patient acuity. Therefore,
the feasibility of the Human Factors Analysis and Classification System
for Healthcare was explored to identify underlying factors contributing
towards adverse events and near misses in the pediatric intensive care
unit.
Methods: Adverse events and near misses reported within the
pediatric intensive care unit over five years were obtained from
a nonprofit, tertiary care, academic medical center in Southern
California. Researchers applied the Human Factors Analysis and
Classification System for Healthcare framework to identify contributing
factors.
Results: Using the Human Factors Analysis and Classification
System for Healthcare framework, two trained human factors experts
analyzed 272 events to identify contributing factors within the event
narratives, resulting in identification of 340 causal factors. The top three
contributing factors identified within the reports included skill-based
errors (n=90, 26.47%), coordination breakdowns (n=70, 20.59%), and
tools/technology breakdowns (n=49, 14.41%).
Conclusions: Adverse events and near misses in the pediatric
intensive care unit can be addressed and improved with targeted
human factors interventions by identifying areas of systemic weakness
for the development of targeted patient safety interventions. The
application of the Human Factors Analysis and Classification System
for Healthcare framework to event reporting narratives bridges a gap
in the understanding of safety events translating into a framework for
clinical quality improvement.
Abbreviations: AE, adverse event; CF, contributing factor; HFACS-Healthcare,
Human Factors Analysis and Classification System for Healthcare; MIP, medication infusion pump; NM, near-miss; PICU, pediatric intensive care unit.
Introduction
The pediatric intensive care unit (PICU) is a complex, high-acuity
environment with increased potential for adverse events (AE). AE
are unintended injuries that may result in temporary or permanent
disability, death, or prolonged hospital stay
[1]. Patients in the PICU
setting often experience increased illness severity, more invasive
interventions, and multiple interactions at the human-technology
interface [2,3]. A 2010 study [4] found that as many as 62% of
PICU patients experienced at least one AE during their stay, where
10% were classified as life-threatening or permanent, and 45% were
deemed preventable. A recent single centered study from Europe in
2020 found that of 842 patients admitted to the PICU, 142 (16.86%)
experienced at least one AE during their stay, where 91.2% were
considered preventable [5].
AEs occur within a complex socio-technical healthcare system,
in which systems components (humans, tools/technology, tasks,
environments, organizations) [6] interact in ways that may contribute
to AEs. One strategy for improving patient safety and reducing
the likelihood of AEs involves exploring contributing factors (CF)
associated with these incidents, leading to targeted solutions and
improved patient safety [7,8].
The reporting of near misses and unsafe conditions, by healthcare
professionals who are directly or indirectly involved in the event, is
vital for identifying and addressing latent safety issues to prevent AEs
[9]. Near-miss (NM) events (unplanned events that did not result
in injury, illness or damage, but had the potential to do so) present
an opportunity to identify and correct flaws that jeopardize patient
safety [10]. A continuum of cascade effects exists from apparently
trivial incidents to near misses and full-blown adverse events [10,11].
Consequently, the same patterns of causes of failure and their relations
precede both adverse events and near misses. Incident reporting can
provide interesting insights into the current state of the healthcare
system; however, limitations exist with current incident reporting
processes, including broad criteria for what to report, a general focus
on quantity of quality of data, biased reports from the perspective of
one person, the need for pragmatic and flexible taxonomies to classify
patient safety problems, reporting pathways often involving reporting
to supervisors, limiting what information is disclosed, and a lack of
feedback [12].
These limitations constrain incident reporting from being used
as a reliable epidemiological tool to measure the frequency of events
and whether interventions are effective in improving patient safety
[13]. The value of incident report data quickly diminishes without
the application of a reliable, systemic framework to investigate and
generalize CF reported across multiple events [7].
In prior work, researchers utilized the human factors analysis and
classification system for healthcare (HFACS-healthcare) to analyze
systems factors that may have contributed to surgery-related incidents
across a hospital system [7]. The HFACS framework was developed
based James Reason’s Swiss-cheese model of accident causation and is
organized by four tiers [7, 14]: 1) organizational influences; 2) unsafe
supervision; 3) preconditions for unsafe acts; and 4) unsafe acts
[7,14,15]. The HFACS framework was expanded upon to better fit
specific healthcare-focused needs resulting in the HFACS-Healthcare
framework [7]. The aim of this study was to investigate the feasibility
of using the HFACS-healthcare framework to analyze previously
reported events in a PICU over five years to identify underlying work system
factors related to the reported events.
Material and Methods
Data Collection:
Following Institutional Review Board (STUDY00001911)
approval, PICU event reports were collected from a nonprofit, tertiary
care academic medical center in Los Angeles, California, between
January 2016, and April 2021. The medical center’s 12-bed pediatric
intensive care unit (PICU) is combined with the congenital cardiac
intensive care unit and admits patients with medical and surgical
needs including congenital cardiac surgery, neurosurgery, orthopedic
surgery, and renal transplantation.The institution utilizes an anonymous electronic incident
reporting system to promote patient safety and improve patient
care [7]. The incident reporting system is available to all hospital
personnel to document near misses, good catches, and safety events
that affect patients, visitors, and staff. Upon submitting an incident
report, users provide information on the demographics surrounding
the event, a narrative review, and assess severity according to the
National Coordinating Council for Medication Error Reporting and
Prevention (NCC MERP) classification [16]. Data obtained for this
study included the event number, event type, specific event type,
person affected, medical record number, patient age, event date,
department, location of the event, level of harm, and a narrative
describing the event details.
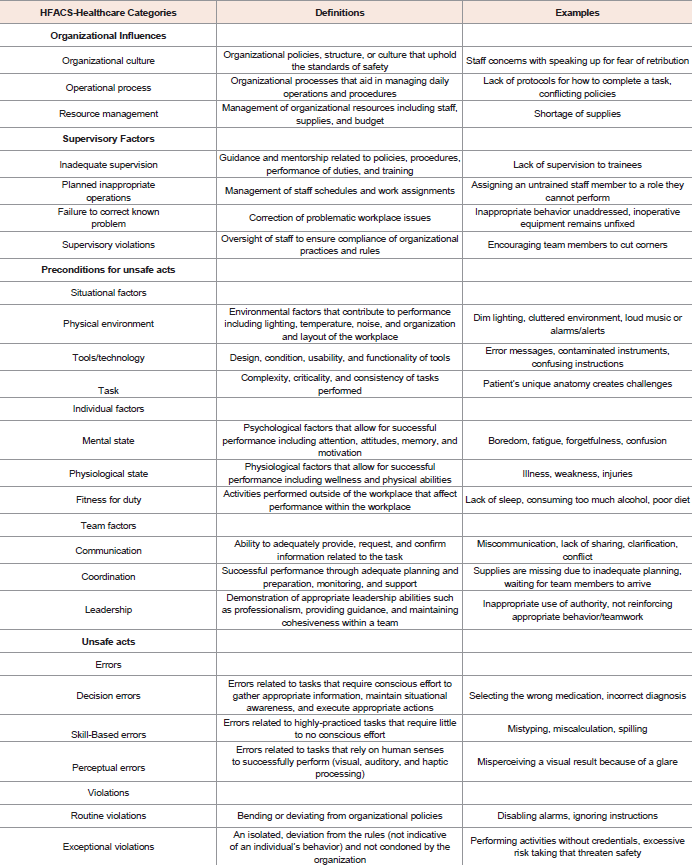
HFACS Classification:
The HFACS-Healthcare classification system was used to classify
identified factors into one of the 21 categories to analyze CFs associated
with each event [Table 1]. Two trained human factors researchers
analyzed the data in two stages as done similarly in other research
[17]: stage one - each rater individually reviewed event narratives to
identify CFs, coming to consensus on the number of CFs within each
event; stage two - researchers individually categorized each CF into
one of the 21 HFACS-Healthcare categories. Interrater reliability was
assessed, and reviewers came to a consensus on any disagreements.Subsequently the narratives within the three most populated
HFACS-Healthcare categories were sub-classified using the methods
above to further understand specific underlying issues contributing to
the incident. The sub-classification was developed using themes that
appeared throughout events within each category.
Data Analysis:
Microsoft Excel was used to analyze the data. Contributing factors
were summed across events and by year and patient demographics
and harm classifications assigned to each AE or NM were calculated
and analyzed.Results
Demographics:
During the study period (January 2, 2016, to April 19, 2021), 1,676
patients were admitted to the PICU and 331 events were reported
across 114 patients. Patient age ranged from under 1 year of age to
17 years of age, with most being under 1 year old (n=139, 41.99%),
followed by 1-3 years of age (n=50, 15.11%), and 13-15 years of age
(n=46, 13.90%).Of the 331 events reported, 288 (87%) included an associated level
of harm. Incidents most often involved the following classifications:
1) “reached patient, no harm” (n=133, 40.18%); 2) “did not reach
patient” (n=46, 13.90%); and 3) “capacity for error (good catch)”
(n=42, 12.69%). The remaining reports with associated level of harm
classifications included: monitor patient, no harm (n = 28, 8.46%);
intervention required, temporary harm (n = 28, 8.46%); death (n = 6,
1.81%); intervention to sustain life (n = 4, 1.21%); and extended stay,
temporary harm (n = 1, 0.30%).
HFACS Classification:
Inter-rater reliability among reviewers was 84.88% before
consensus was made on disagreements. After removing duplicate
entries (n = 13, 3.93%), a total of 272 events (82.18%) could be
analyzed using the HFACS-Healthcare classification system. The 46
(13.90%) events that could not be analyzed did not include enough
information to conduct a systemic analysis and only provided a brief
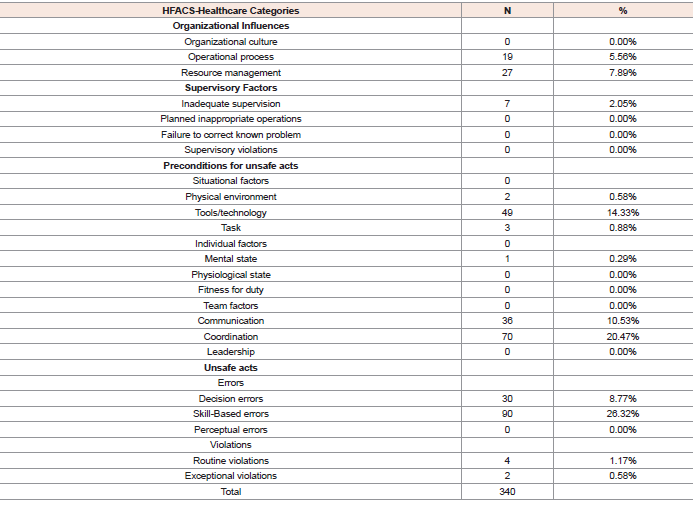
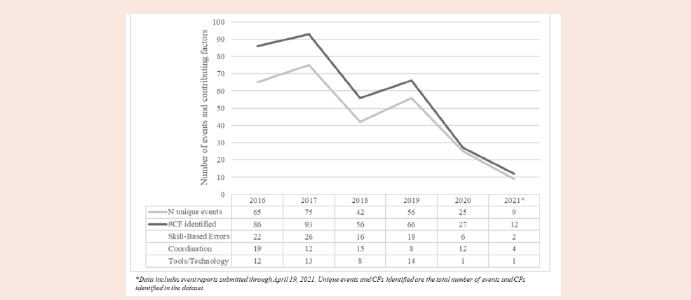
factual description of the event type (e.g., “code blue”).Of the remaining 272 reports, 216 (79.41%) included one CF, 46
(16.91%) included two CFs, 8 (2.94%) reports each included three CFs,
and the remaining 2 (0.73%) event reports included four CFs. Between
2016 and 2021 the number of incidents reported trended down with
a total of 49 events reported in 2016 and 19 reported in 2020. The
CF categories most often cited included skill-based errors (i.e., errors
that occur in highly practiced tasks) (n=90, 26.47%), coordination
breakdowns (i.e., breakdowns within teamwork, planning, assistance,
etc.) (n=70, 20.59%), and breakdowns due to issues with tools and
technology (i.e., usability issues, poor condition, functionality, etc.)
(n=49, 14.41%) [Figure 1][Table 2].
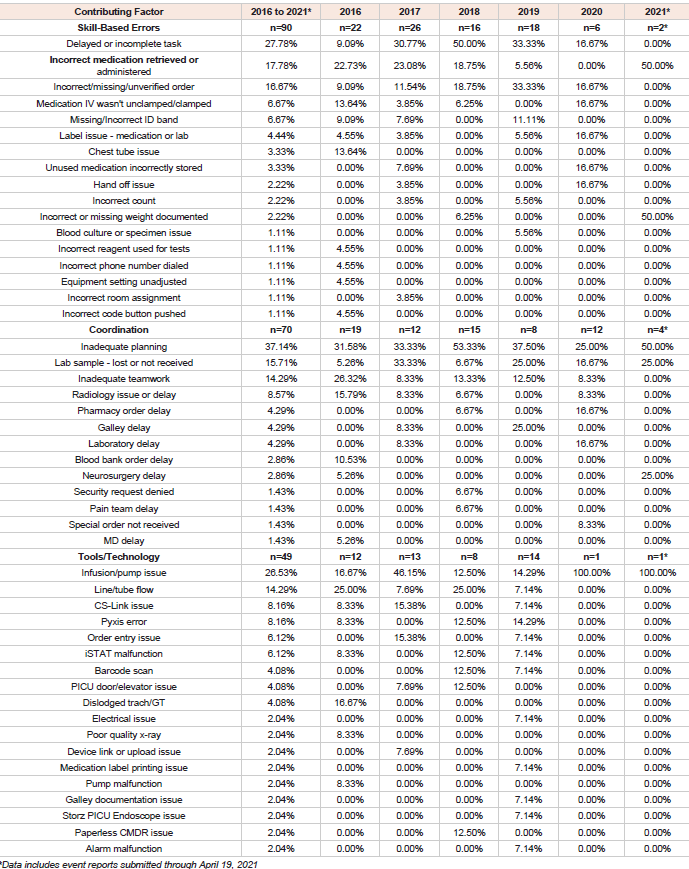
Narratives involving skill-based errors, coordination breakdowns
and tools and technology issues were sub-classified to identify the
underlying issues that contributed to each event. Skill-based errors
involved delayed or incomplete tasks (n=25, 27.78%), retrieving or
administering incorrect medication (n=16, 17.78%), and incorrect,
missing, or unverified orders (n=15, 16.67%). Coordination
breakdowns involved problems with planning (n=26, 37.14%),
coordinating lab samples (n=11, 15.71%), and teamwork (n=10,
14.29%). Finally, tools and technology breakdowns included issues
with infusions and pumps (n=14, 26.53%), the flow of medication
within a line or tube (n=7, 14.29%), pyxis errors (n=4, 8.16%), and
problems with the design of the electronic health record (n=4, 8.16%)
[Table 3].
Table 1: Definitions and associated examples for the Human Factors Analysis and Classification System for health care categories
Discussion
In the present study, researchers assessed the feasibility and
applicability of the HFACS-Healthcare framework to identify CFs
associated with AEs and NMs reported in a PICU over five years.
During the study period, 324 unique events were reported, where
272 provided enough contextual information about the event to be
analyzed using HFACS-Healthcare. Ultimately 340 contributing
factors were identified.
Over the course of the study the total number of events reported
trended down from 65 events reported in 2016 to 25 events reported
in 2020. While this finding could be indicative that safety in the
healthcare system has improved overtime, it may also speak to factors
influencing incident reporting including fear of retribution, usability
challenges associated with event reporting, and even the COVID-19
pandemic influencing workload during 2020-2021 reducing the time
available to submit incident reports. Thus, the discussion is focused
on the CFs that were identified from this analysis and opportunities
to improve the sociotechnical work system.
Most of the event reports cited one CF, many referenced two or
more CFs. Consider the following example obtained from the study
data:
[“…Trauma patient that had several MDs in the room calling out
medication orders…In the emergent situation of attempting to stabilize
trauma patient no MD could place orders in the MAR resulting in
confusion of rate of medication, no harm to patient… RNs to place
orders under emergent verbal to link drips to the MAR”]
Although the identified error within this narrative is “incorrect
medication rate” when analyzed using HFACS-Healthcare, three CFs
emerge: 1) the patient had many attending and trainee physicians
calling out medication orders (communication); 2) the physicians
were unable to input orders into the medical record while stabilizing
the patient (task); and 3) there was confusion in the rate of medication
(skill-based error). Human factors analysis and aggregation of
incident data provides novel insights into the system’s current state.
The most common CFs identified were skill-based errors,
coordination breakdowns, and issues with tools and technology.
Medication errors related to incorrect, missing, or unverified orders
and the incorrect retrieval or administration of medication were
important contributors within the sub-categories of skill-based
errors. The underlying factors contributing to skill-based errors may
be related to a complex interaction amongst organizational factors
such as inadequate staffing during busy census with high acuity
patients assigned to a single health care provider leading to errors in
task execution or poorly designed equipment and ergonomics leading
to “workarounds” [18] and inefficiency. Prescribing errors in PICUs
have been found to relate to the increased cognitive demand required
for completing tasks associated with prescribing medication [19]. In
a tertiary care center with a mix of adult and pediatric patients, the
providers must navigate through multiple electronic health record
interfaces to complete a medication order leading to a cognitive
disconnect and information overload [20].
Coordination issues identified involved inadequate planning
or inadequate teamwork related to supporting services such as
nutrition, handoffs to the pediatric ward or emergency department,
or communication with the blood bank. The importance of teamwork
within the intensive care unit cannot be overstressed - the ICU has
emerged to be a team sport with patient outcomes being related not
only to individual knowledge, skills, and attitudes, but the collective
wisdom of the entire team [21]. Strategies to improve coordination
issues include the use of checklists, crisis resource management
principles, and teamwork training [22-25].
The third most common challenge cited involved issues with
tools and technology. Medication infusion pump (MIP) errors
were common along with issues concerning the flow within a
line or tube and pyxis errors. The FDA-sponsored Infusion Pump
Summit (2010) identified poor human-machine interface design
as a critical shortcoming of current MIP [26,27]. Clinicians often
find themselves adapting their workflow to the designs of the MIP,
as opposed to having access to MIP that are designed to meet their
needs and workflow. However, several studies have concluded that
implementing smart pumps in units treating critically ill patients had
no impact on the number of severe medication errors prevented
[28-30]. Enabling the interception of infusion programming errors could
be used to improve patient safety to avoid the potential for severe
injury to pediatric patients [31]. Being aware of the CFs involved with
MIP-related AEs or NMs allows for the design of systemic solutions
that may reduce repeat events.
Other work exploring event reporting in pediatric medicine has
included single-site studies focused on PICUs [32-34], multicenter
studies involving children’s hospitals [35] and the Pediatric
Emergency Research Network (PECARN) [36]. Although there are
differences in the methodologies [3,4], objectives [5], study periods, and taxonomies for classification [37,38], the findings presented
here demonstrate similar themes including noncompliance with
established procedures, process failures, and communication failures
[35,36].
This study adds to the existing literature supporting the value
of exploring healthcare-related events with a human factors’ lens.
A human factors approach will explore problems by looking at the
humans within a system, their interactions with one another and
various system components, and redesigns the tasks, interfaces,
and system to make lasting improvements [39]. Exploration of the
underlying CFs by trained individuals is key to the development of
targeted patient safety solutions. Other studies have also found value
in applying human factors methods to critical care patient safety as
it helps us to understand ‘work as done’ in the clinical environment
versus “work as imagined’ [40]. Moreover, these approaches redirect
quality improvement efforts to focus on redesigning systems (e.g.,
environments, tasks, tools and technology, and organization) [6] to
improve human performance. Rather than developing more policies,
channeling resources to compliance of policies as a reaction to AE and
NM (retroactive), investigation into the CFs in a systematic manner
with a system like HFACS-Healthcare (proactive) leads to a better
understanding of poorly designed systems and unmet needs within
the PICU [40].
Limitations
It is important to note that the retrospective data utilized for
analysis originates from a single institution and is not necessarily
generalizable across hospitals or pediatric centers, or units with
different team compositions (trainees, advanced practice providers
etc.). The study site’s unique setting involves a PICU in the pediatric
department located within a tertiary academic institution that is a
non-children’s hospital; hence the case-mix (acuity, type of patients)
could be different from a free-standing children’s hospital.
Additionally, the event data utilized relies heavily on untrained
frontline health care providers to enter events and assign a level of
harm voluntarily. Healthcare providers rarely receive guidance on
what type of information should be included in the report (e.g.,
contributing systemic factors) to make it useful.
Conclusion
Applying the HFACS-Healthcare framework to event reporting in
the PICU may aid in rethinking solutions that may positively impact
provider workflow and patient safety. With further research applying
the HFACS-Healthcare framework to other settings (academic
children’s hospital or the community pediatric intensive care unit),
unique CFs could be explored, prompting the proactive application
of targeted patient safety solutions for the unique environments with
interventions for longitudinal sustainment.
Source of Funding: This research received no specific grant from
funding agencies in the public, commercial, or not-for-profit sectors.