Journal of Pediatrics & Child Care
Download PDF
Research Article
Use of Diuretics for Bronchopulmonary Dysplasia Increases Metabolic Bone Disease in Preterm Infants
Bhatia S1,2*, Abraham MJ1,3, Mehdi MQ1,4, Niebuhr B1 and Jain SK1
1Department of Neonatology, Department of Pediatrics, University
of Texas Medical Branch, Galveston, TX USA
2Division of Pediatric Cardiology, Department of Pediatrics,
Children’s Hospital of Michigan, Detroit, MI USA
3Department of Neurology, University of Texas Health Science
Center San Antonio Joe and Teresa Long School of Medicine, San
Antonio, TX USA
4Department of Pediatric Cardiology, University of Texas Southwestern Medical Center, Dallas, TX USA
4Department of Pediatric Cardiology, University of Texas Southwestern Medical Center, Dallas, TX USA
*Address for Correspondence: Snigdha Bhatia, Division of Pediatric Cardiology,
Department of Pediatrics, Children’s Hospital of Michigan, Detroit, MI, USA Email Id: snigdhabhatia@gmail.com;
Phone: 832-991-2172
Submission: 08 June 2023
Accepted: 26 July 2023
Published: 31 July 2023
Copyright: © 2023 Bhatia S, et al. This is an open access
article distributed under the Creative Commons Attr-ibution
License, which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is
properly cited.
Keywords: Metabolic bone disease; Prematurity; Bronchopulmonary
dysplasia
Abstract
Objective: Preterm infants (PI) are at increased risk of developing
metabolic bone disease (MBD).This study assessed the association of
diuretics for bronchopulmonary dysplasia (BPD) with MBD.
Study Design: This retrospective study included infants ≤30 weeks gestation and birth weight ≤1500 grams. Infants were divided into diuretic group and control group. Diuretic use was defined as hydrochlorothiazide and spironolactone for >7 days and MBD as PTH >100 mg/dL. Data was analyzed using SPSS and p <0.05 was considered significant.
Results: The study included 201 infants, with a mean gestational age 26.31 ± 1.73 weeks. There were 68 (33%) in the diuretic group vs. 133 (67%) in the control group. 41 vs. 24% (p<0.05) infants in the diuretics group who received diuretics for BPD also developed MBD. 80% vs. 20% (p<0.001) infants with BPD were treated with diuretics. Diuretics did not improve the respiratory status in these PI. We found infants given diuretics remained on ventilation for longer total number of days (p<0.001).
Conclusion: PI treated with diuretics for BPD are more likely to develop MBD without any significant improvement in respiratory status
Study Design: This retrospective study included infants ≤30 weeks gestation and birth weight ≤1500 grams. Infants were divided into diuretic group and control group. Diuretic use was defined as hydrochlorothiazide and spironolactone for >7 days and MBD as PTH >100 mg/dL. Data was analyzed using SPSS and p <0.05 was considered significant.
Results: The study included 201 infants, with a mean gestational age 26.31 ± 1.73 weeks. There were 68 (33%) in the diuretic group vs. 133 (67%) in the control group. 41 vs. 24% (p<0.05) infants in the diuretics group who received diuretics for BPD also developed MBD. 80% vs. 20% (p<0.001) infants with BPD were treated with diuretics. Diuretics did not improve the respiratory status in these PI. We found infants given diuretics remained on ventilation for longer total number of days (p<0.001).
Conclusion: PI treated with diuretics for BPD are more likely to develop MBD without any significant improvement in respiratory status
Abbreviations
BPD (bronchopulmonary dysplasia); MBD (metabolic bone
disease); PI (premature infants); PTH (parathyroid hormone)
Introduction
Bronchopulmonary dysplasia (BPD) is a chronic lung disease
that develops because of neonatal/perinatal lung injury. It is the most
common respiratory complication of prematurity and is associated
with an increased risk of death and poor neurodevelopment outcomes
[1]. Currently, there is no US Food and Drug Administrationapproved
treatment to prevent BPD. Many off-label therapies such
as caffeine (timing and duration still under investigation), vitamin
A, postnatal systemic steroids (associated with poor long-term
neurodevelopment outcomes), and diuretics are used in infants with
BPD (no proven efficacy and safety profile) [2].
Long-term use of diuretics in infants with BPD is common
to improve lung mechanics and gas exchange. The rationale for
this practice lies in targeting clinical, radiographic, and pathologic
evidence of interstitial and peribronchiolar pulmonary edema [3] and
some studies show that occasionally diuretics improve gas exchange
by improving lung compliance and decreasing pulmonary resistance
[4]. Hydrochlorothiazide and spironolactone combination is the
most used diuretic combination in infants with BPD [5-8] Thiazides
and spironolactone both act on the distal tubule, and their combined
use causes fever electrolyte abnormalities compared to loop diuretics
such as furosemide.
Prematurity also predisposes neonates from the time of birth,
towards developing metabolic bone disease (MBD). Approximately
80% of fetal bone mineralization occurs in the third trimester of
pregnancy (32-36 weeks) [8]. This mineralization and accretion is
often lost when a neonate is born prematurely. Studies have shown
that although MBD may be a self-limiting condition, its long-term
effect on stature, bone development, kidney function and future risk
of osteoporosis is not to be dismissed [9,10]. Orth et al attempted to
study the effect of early versus late initiation of diuretics in patients
with MBD and found no difference in the development of MBD
based on the timing of exposure [11]. In another study by Chen et
al, prolonged use of diuretics > 2 weeks was noted to be a risk factor
for the development of MBD in neonates ≤ 32 weeks gestation [12].
The role of chronic diuretic use for BPD and the increased risk of
developing MBD in premature infants (PI) remain undetermined.
The aim of this study was to determine the association of chronic
diuretic use for BPD and MBD in PI.
Methodology
Study Population: This is a retrospective case-control
study conducted at level IV neonatal intensive care unit
at The University of Texas Medical Branch (UTMB),
Galveston. The institutional review board (IRB 18-0073) at
UTMB approved the study and waived the need for consent.
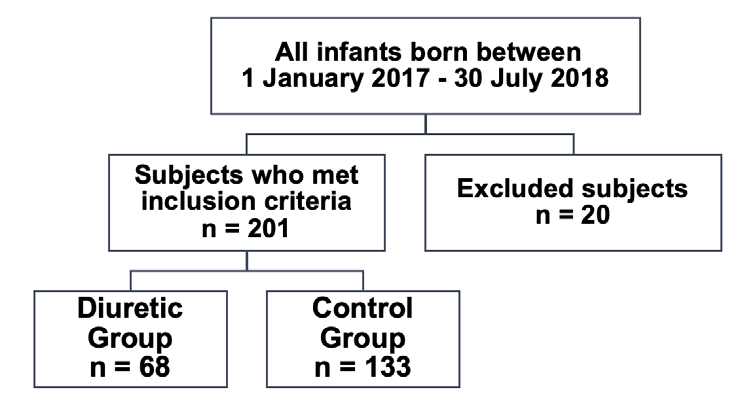
Inclusion and Exclusion Criteria: The electronic medical record
for all infants born at our center between 1st January 2017 and 30th
July 2018 was reviewed (n=221). Infants with birth weight ≤1500 g
and ≤30 weeks gestational age who were admitted to the neonatal
intensive care unit were included in the study (n=201).Infants with
known lethal chromosomal or congenital abnormalities, necrotizing
enter colitis, or spontaneous intestinal perforation were excluded
from the study.
Study groups: The study population was divided into the diuretic
group (infants who received hydrochlorothiazide and spironolactone
for BPD for >7 days), and the control group (infants who did not
receive diuretics). Their hospital course was reviewed for the
development of MBD before, during, and after the start of diuretics.
Definition of BPD: BPD was defined as infants requiring
respiratory support at 36 weeks postmenstrual age [13].
Definition of MBD: Parathyroid hormone (PTH) levels > 100
IU/L and X-ray evidence of fraying and irregular femoral metaphysic.
Screening of MBD: In our center, routine screening for MBD
is done at 4 weeks postmenstrual age for infants born at ≤34
weeks of gestation. These neonates undergo screening for MBD
which includes serum calcium, phosphorus, alkaline phosphatase
(ALP), PTH, Vitamin A levels and X-Rays of bilateral knees. PTH
>100 IU/Lis considered significant for MBD and knee X-rays,
25-hydroxy Vitamin D levels are obtained, and calcium bicarbonate
supplementation is started. The PTH level is then obtained every
2 weeks until 2 consecutive PTH values are <100 IU/L. Evidence
of femur demineralization and irregular metaphyseal edges are
considered positive for MBD on radiographic imaging.
Data collection:
Chart review was performed, and clinical data included gestational
age, birth weight, gender, diagnosis of BPD, duration of parenteral
nutrition, IUGR, comorbidities, history of metabolic bone disease,
diuretic use, mean days on various respiratory support, X-ray findings
and sodium supplementation were noted. Maternal characteristics
such as history of infection, chorioamnionitis, premature prolonged
rupture of membranes, chronic hypertension or pregnancy-induced
hypertension, use of antenatal steroids were also collected.Statistical analysis: Statistical analyses were carried out
using SPSS. Procedures used included Chi-Square test and t-test.
Multivariate analysis was done using likelihood ratio forward stepwise
method. The level of statistical significance was set at p < 0.05.
Results
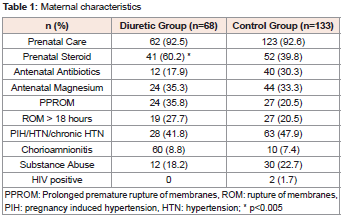
During the study period from January 2017 to August 2018,
201 neonates ≤ 30 weeks of gestation at the time of birth, and with
birth weight ≤1500 grams were included in the study. Of these, 68
neonates received diuretics for BPD for ≥ 7 days, and 133 neonates
did not (control group) [Figure 1]. The mean gestational age of the
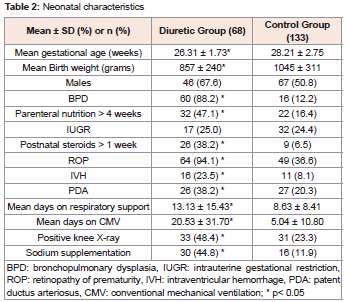
infants in the diuretic group was 26.31 weeks ± 1.7 days vs. 28.21
weeks ± 2.8 days in the control group. The maternal demographics
for the two groups are summarized in [Table 1] . A significant number
of PI in the diuretic group had maternal history of prenatal steroid
administration (60.2% vs. 39.8% respectively). The infants in the
diuretic group were significantly younger (26.31 weeks ± 1.7 days
vs. 28.21 weeks ± 2.8 days in the control group) and smaller (857
± 240 grams vs 1045 ± 311 grams in the control group and had a
significantly higher incidence of comorbidities such as BPD, MBD,
intraventricular hemorrhage and patent ductus arteriosus [Table 2] .
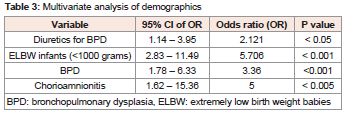
Multivariate logistical regression analysis was done for the significant
variables from the univariate analysis which showed that use of
diuretics for BPD, extremely low birth weight (<1000 grams), BPD
and chorioamnionitis were independently associated with the risk of
MBD between the two groups [Table 3] .
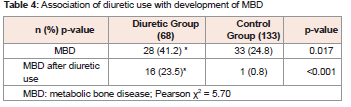
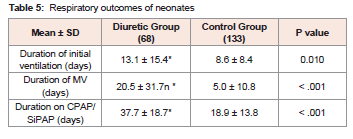
Our study showed that a significant number of neonates developed
MBD after starting diuretics (41% vs. 33%, p=0.017) [Table 4] .The
duration of initial days of mechanical ventilation (13.1 ± 15.4 days vs.
8.63 ± 8.41 days in the control group, p=0.010) as well as total days of
mechanical ventilation (20.5 ± 31.7 vs.5.0 ± 10.8 days, p<0.001) were
significantly higher in the diuretic group compares to the control
group [Table 5] Similarly, the number of days of positive-pressure
ventilation i.e. continuous positive-pressure ventilation or biphasic
positive-pressure ventilation were also higher in the diuretic group.
We attempted to measure improvement in FiO2 requirement in these
neonates, which was limited by changes in modes of ventilation and
not amenable to statistical analysis.
Discussion
Our study showed that PI who receive diureticsfor BPD have
significantly higher rates of MBD(23% vs 0.8% p<0.001). This could
be confounded by the likelihood that such neonates are comparatively
more premature, have lower birth weight and worse respiratory
disease, but multivariate analysis confirmed that the high rate of MBD
in the diuretic group was independent of gestational age. The study
by Orth et al suggested that the timing of starting diuretics did not
affect the onset of MBD, and the total cumulative dose of furosemide
may be associated with a higher incidence of MBD [11]. We studied
the onset of MBD in PI after diuretic use for >7 days and did find
higher rates of MBD in these infants after diuretic use compared to
the control groups.
Despite advances in parenteral and enteral nutrition modalities for
premature neonates, MBD continues to be a significant co-morbidity
of prematurity. MBD is defined as decreased bone mineralization,
and its biochemical and diagnostic criteria varies from center to
center. Our center uses PTH as the biomarker for MBD screening,
and it has been shown to be more sensitive than ALP in a previous
study at our institute [14].
Premature infants lose the potential accretion of approximately
2.3-2.98 mmol/day of calcium and 1.9-2.98 mmol/day of phosphorus
due to their preterm birth [17,15] This lack of accretion makes them
more vulnerable to developing MBD than term infants. In addition,
pathophysiology of MBD in premature infants is multifactorial
[8,15]. Immature digestive system, use of total parenteral nutrition,
use of diuretics for fluid retention, congestive heart failure,
mineralocorticoid use for adrenal insufficiency, lack of mobility
and hormone imbalance also contribute to MBD [16] .Conditions
affecting placental transport of nutrients such as chorioamnionitis
and IUGR are also associated with high risk of MBD due decreased
in utero phosphate transport [16,17]. In our study, the presence of
chorioamnionitis increased the odds of MBD by five times (CI 1.65-
15.36, p <0.005). A higher incidence of postnatal MBD has been noted
in infants with IUGR in the study by Montaner Ramón et al [17],
however due to a smaller sample size we did not find this association.
A study of 835 infants from the prematurity and respiratory
outcomes program (PROP) did not show any improvement in long
term respiratory outcomes of infants when diuretics were used for
BPD [18]. Furosemide was the diuretic used in majority of these
patients whereas we studied hydrochlorothiazide and spironolactone
use, which are widely used for chronic management due to their
comparatively safer adverse effect profile.
Interestingly, the PROP study noted an increase in the need for
respiratory support in patients 1-7 days after receiving diuretics. Our
study supported these findings, as the mean duration of mechanical
ventilation as well as positive pressure ventilation was higher in the
diuretic group than the control group.
Across the US, 1/3rd premature infants <1500 grams birth weight
receive diuretics for BPD with a wide variation across the neonatal
centers [5]. This wide variation is because of potential adverse effects
of diuretics along with a lack of medical evidence of the timing,
appropriate dose, correct indication, and most importantly, level of
efficacy for the prevention of BPD. No randomized controlled trials
of diuretics use to prevent BPD have been done.
The results of our study are limited by its small sample size.
Though this is the first study to establish an increased risk of MBD in
PI after treatment with diuretics, these results need to be validated by
larger multicenter studies. Secondly, there is no standard definition
of MBD across centers, and different biomarkers are used in PI to
diagnose MBD. Our study used PTH to define presence of MBD,
which may not be a standard practice in other centers. Finally, our
study did not record the effect of diuretic use on MBD over longterm
follow-up. Longitudinal studies will help to establish the clinical
implications of MBD associated with diuretic use in PI.
Conclusion
Preterm infants treated with hydrochlorothiazide and
spironolactone for BPD are more likely to develop MBD after
diuretic use without any significant improvement in respiratory
status. Diuretic use in premature infants did not decrease the mean
duration of mechanical ventilation and positive pressure ventilation
compared to the control group. Diuretics should be used with caution
and monitored closely for MBD.
Ethics Approval:
The study was approved by the Institutional Review Board at
the University of Texas Medical Branch, Galveston, TX. Need for
consent was waived. The study was performed in accordance with the
Declaration of Helsinki.Contributor’s Statement:
Drs. Snigdha Bhatia and Sunil K Jain conceptualized and designed
the study, coordinated and supervised data collection, and critically
reviewed the manuscript for important intellectual content.
Drs. Snigdha Bhatia, and Maria J Abraham collected the data and
reviewed and revised the manuscript.
Drs. Mohammad Q Mehdi and Bruce Niebuhr carried out the
statistical analysis.
All authors approved the final manuscript as submitted and agree
to be accountable for all aspects of the work.