Journal of Pediatrics & Child Care
Download PDF
Research Article
Evaluating the Feasibility and Utility of an Educational Webinar Series on Autism for Pediatric Primary Care Providers: A Pilot Study
Ayala-Brittain ML1, Bergez-Cohn KC1, Mire SS1,2, Ahmed KL4, Berry LN3,4, Monteiro SA4, Strickland DC5 and Goin-Kochel RP3,4*
1Department of Psychological, Health, & Learning Sciences,
University of Houston, Houston, TX, USA
2Department of Educational Psychology, Baylor University, Waco,
TX, USA
3Psychology Section, Department of Pediatrics, Baylor College of
Medicine, Houston, TX, USA
4Meyer Center for Developmental Pediatrics &Autism, Texas
Children’s Hospital, Houston, TX, USA
5DiagnoseFirst, Raleigh, NC, USA
*Address for Correspondence:
Goin-Kochel RP, Psychology Section, Department of
Pediatrics, Baylor College of Medicine, Houston, TX, USA;
Telephone: 832-824-3390; Facsimile: 832-825-3399;
E-mail: kochel@bcm.edu
Submission: 10 February, 2023
Accepted: 24 March, 2023
Published: 29 March, 2023
Copyright: © 2023 Ayala-Brittain ML, et al. This is an open
access article distributed under the Creative Commons Attribution
License, which permits unrestricted use, distribution,
and reproduction in any medium, provided the original work
is properly cited.
Abstract
Background: Parents of children later diagnosed with autism
spectrum disorder (ASD) frequently raise concerns about their
child’s behavior and development with their pediatric primary
care providers (PPCPs). However, few PPCPs make timely referrals
to ASD specialists following positive ASD-screening results, and
even fewer evaluate for ASD themselves-actions that contribute
to the ASD-detection gap (i.e., the time span between first
concerns and eventual diagnosis). Some literature suggests that
PPCPs’ lack of knowledge about and/or confidence in managing
ASD/suspected ASD contributes to referral and diagnostic delays.
Methods: To evaluate the utility of an online educational
platform to guide PPCPs in the early identification and
management of ASD, we invited PPCPs within a hospital-affiliated,
pediatric-practice network to participate in a three-part webinar
series on screening, diagnosis, and referral practices for ASD.
Each webinar lasted approximately one hour and conferred one
continuing medical education credit. Pre- and post-test surveys
were imbedded within each webinar and solicited open-ended
feedback.
Results: Among 288 potential participants, 37 (12.8%)
completed the first of three webinars and 28 (9.7%) completed all
three. All pre-post knowledge and confidence scores increased
significantly for each webinar (all p ≤ .001). Participants’ openended
feedback was largely positive; most reports cited
information about the M-CHAT-R/F follow-up interview (Screening
webinar), videos contrasting neurotypical/atypical behaviors
(Diagnosis webinar), information on testing/medical workup
(Referral webinar), and referral resources (Referral webinar) as the
most helpful aspects.
Conclusion: The PPCP response rate was relatively low, despite
efforts to increase engagement with the webinars. This may
have resulted from lack of time, a frequently reported barrier to
PPCPs’ participation in educational activities. Among those who
participated, significant knowledge and confidence gains were
observed, and provider feedback was overwhelmingly positive.
Findings have implications for the development/refinement
of such webinars for broader distribution, as well as alternate
learning platforms to increase utility.
Keywords
Autism Spectrum Disorder; Pediatric Primary Care;
Pediatricians; Knowledge and Confidence
Introduction
Diagnostic prevalence of autism spectrum disorder (ASD) has
dramatically increased in the United States (U.S.), with the latest
figure estimating 1-in-44 children have ASD [1]. Although core
symptoms of ASD are usually observed within the first 2 years of life,
only 42% of children with ASD are evaluated before age three [2]. Currently, the average age at ASD diagnosis in the U.S. is around
4 years, meaning many children are missing out on important
interventions during the window of opportunity when they are most
impactful [3]. Early diagnosis is key to families’ access to intensive
behavioral interventions that promote developmental outcomes
across domains (language skills, adaptive-functioning skills, social
skills) and throughout the lifespan. However, the present delay of
approximately 2.7 years between initial parent concerns and ASD
diagnosis (i.e., “the ASD-detection gap”) is especially concerning
because diagnostic delays or inaccurate diagnoses can limit or
prevent access to these services. Moreover, these delays maybe even
greater for children from under-resourced or minoritized groups
[4], representing a social injustice and highlighting the necessity of
increasing access to timely diagnostic services for all children with
suspected ASD. Bolstering access through existing points of contact
in primary care represents a potentially effective mechanism for
accomplishing such aims.
The Role of Pediatric Primary Care Providers in Early ASD Identification:
During the first five years of a child’s life, pediatric primary care
providers (PPCPs) are typically the first point of contact for families
when developmental concerns arise, which coincides with the critical
years for an ASD diagnosis (Committee on Children with Disabilities
[CCD], 2001; [5-7]. Because of the frequency of well-child visits and
parent familiarity with pediatric offices, PPCPs are essential to early,
accurate ASD identification and are considered a gateway to early intervention services. PPCPs serve multiple roles in this process,
including responding to parents’ initial concerns, recognizing atrisk
children though routine developmental surveillance, diagnosing
ASD, referring children to appropriate specialists, and helping
caregivers advocate for their children [7,15]. Consequently, the
American Academy of Pediatrics (AAP) provides specific guidelines
for PPCPs with regard to identifying, diagnosing, referring, and
treating children with ASD within the primary care setting [8].Screening Recommendations and Practices Following Positive Screens:
Current AAP guidelines indicate that (a) general developmental
surveillance should take place at the 9-, 18-, 24-, and 30-month
well-child visits to determine whether a child is meeting expected
milestones, and (b) ASD-specific screening should occur at 18- and
24-months to identify children whose symptoms may emerge or
become more apparent during the second year of life (CDC, 2019).
Though research supports the validity of ASD-specific screening
tools in primary care, their use among PPCPs has ranged from as low
as 8% to as high as 60% in recent years [9]. Barriers to use of the
Modified Checklist of Autism in Toddlers, Revised with Follow-Up
(M-CHAT-R/F, one of the most commonly used ASD screeners, have
included an inability to complete necessary follow-up interviews,
time constraints, and provider concerns about false-negative screens
[10]. Despite these barriers, PPCPs in hospital-affiliated pediatric
practice networks have high rates of M-CHAT-R/F screening [11]. In
one of these studies, 93% and 82% of eligible children received ASD
screening at their 18- or 24-month well-child visits, respectively; in
another, 91% of children were screened with the M-CHAT-R/F at
well-child visits between the ages of 16 to 24 months [12].If a child screens positive (i.e., higher likelihood of ASD) and/or
if a PPCP observes concerning symptoms, AAP guidelines suggest
several concurrent steps [7], including referrals for comprehensive
evaluation, audiology evaluation, and early intervention services.
PPCPs should not wait for a definitive ASD diagnosis to make
referrals [7,13]; following this guideline helps to expedite intervention
to address developmental concerns while simultaneously exploring
specific diagnostic considerations, as well as ruling out possible
hearing loss. Yet recent studies suggest that referrals from pediatricians
to ASD specialists are not happening as frequently as recommended.
Monteiro and colleagues (2019) found that even though rates of
ASD-specific screening were high in their study, only 31% of children
who screened positive were referred for ASD specialist evaluation.
Moreover, among these screen-positive children, PPCPs referred
only 20% to ECI and 16% to private therapy (12% were already
receiving services). These results are similar to those of Wallis and
colleagues (2020) who found that 40.2% of children received at least
one recommended referral (i.e., early intervention, audiology, and
comprehensive ASD evaluation); however, only 3.7% received all
recommended referrals.
Reasons for Referral and Diagnostic Inactions Following Positive Screening:
Considering that some interventions are predicated on the
ASD diagnosis, it is critical to understand where potential obstacles
lay in PPCPs’ screening, diagnostic, and referral workflows so that they can be addressed. PPCPs themselves report lacking knowledge
of treatment options, insufficient training in ASD diagnosis and
treatment, ambiguity regarding their role in ASD-specific care, and
difficulty with care coordination [14-16]. Some research indicates
that, although PPCP knowledge of ASD symptomology is high (i.e.,
recognizing language communication problems, social interaction,
limited area of interest), a majority of PPCPs (61%) report difficulty
facilitating connections between families of children with ASD
and community services [17], as well as having discussions about
recommended next steps. PPCPs also consistently report lacking
knowledge about school-based services (Hastings et al., 2014) - a
critical gap because so many families rely heavily on services offered
through their local school districts [18].In addition to lacking knowledge about available services and
supports, PPCPs also hold a number of beliefs about ASD that may
affect their referral/diagnostic actions. Some providers endorse
negative attitudes toward the utility and necessity of validated
screening tools and believe that developmental surveillance alone
is sufficient for ASD identification [19,20]. Other providers claim
they do not refer children with suspected ASD for a comprehensive
evaluation so as to avoid negative emotional reactions from parents.
Many PPCPs report difficulty reconciling the AAP mandate to screen
and diagnose ASD early with a lack of knowledge about treatment
options and resources available for this population [21]. Moreover,
because of insufficient training, many PPCPs report low confidence
in their ability to provide care for children with ASD, as well as low
self-efficacy in the ASD-referral process [4-6]. Lacking knowledge
and confidence in these areas may help explain PPCPs’ poor followthrough
in making necessary referrals to autism specialists, thereby
contributing to the ASD-detection gap.
ASD-Specific Education and Supports for Pediatricians:
One means of addressing PPCPs’ role in ASD identification is
through training that improves their ASD-specific knowledge and
confidence. A study of PPCPs in Brazil found that an educational
training program in ASD identification, diagnosis, and treatment
significantly improved PPCPs’ knowledge about ASD and was
associated with increased referral patterns four months after the
training program ended, with providers referring six times as many
suspected cases of ASD [22]. ASD-specific training programs have
also had significant effects when implemented with medical residents.
In one such study, web-based learning activities, combined with
hands-on training, resulted in 95% of residents reporting increased
confidence identifying ASD within the primary care setting (Hine
et al., 2021). Web-based or online training programs may be
particularly valuable in offering a free and flexible way for healthcare
providers to access such information, and an internet search quickly
reveals that the number of such course offerings abounds. However,
there is limited evidence of their quality and utility. It is not clear
how often such programs are actually being used, how they are
valued by the intended audiences, and whether they influence
providers’ knowledge and confidence about ASD and subsequent
clinical practices. For example, one study found that health care
professionals who held inaccurate perceptions about their role within
the ASD diagnostic process were less likely to acknowledge their
need for such information/supports and advocate for training [13], suggesting that those who are most in need of this information may
be unlikely to seek it on their own. Furthermore, because of the time
and costs involved with developing and updating online training
materials, it is important to examine whether this is an acceptable
educational platform for PPCPs. To that end, the current pilot study
sought to evaluate (a) PPCPs’ use and acceptability of an introductory
educational webinar series on ASD-screening, diagnosis, and referral
practices; and (b) potential improvements in PPCPs’ knowledge and
confidence about ASD-screening, diagnosis, and referral practices
following their participation.Methods
Participants:
Participants were PPCPs from a network of 51 primary care
clinics associated with a large hospital system in Houston, Texas.
Email invitations to PPCPs were sent by the study team in two waves
to 263 providers within the network (Wave 1 [n = 132], Wave 2
[n = 131]). A third group of providers (n = 25) from an integrated
primary care clinic were also invited following a specific request
from their group for training in ASD diagnosis, thus creating a total
sampling pool of 288 providers. Because these participants were
employees of the hospital system, we did not solicit demographic
or otherwise potentially identifiable information. This strategy
helped to maintain privacy, reduce time burden on participants and
encourage participation, and further mimicked real-world training
opportunities (i.e., outside the research context).Materials:
This study was reviewed and approved by the Internal Review
Board at Baylor College of Medicine. The three-part webinar series
was designed by the study team to educate PPCPs in Screening,
Diagnosis, and Referrals for ASD. This series was developed with
input from a paid consultant who had extensive expertise in ASD
screening with the M-CHAT-R/F and in partnership with Diagnose
First (diagnosefirst.com), a web-based resource that provides video based
education and instruction in early ASD detection and ASD
diagnosis. Each of the three webinars included evidence-based
content that was consistent with current AAP-practice parameters
for screening and management of ASD. The Diagnosis webinar,
in particular, focused on ASD core symptoms and included high quality
videos selected from Diagnose First’s extensive ASD video
library that contrasted neurotypical and ASD-related behaviors in
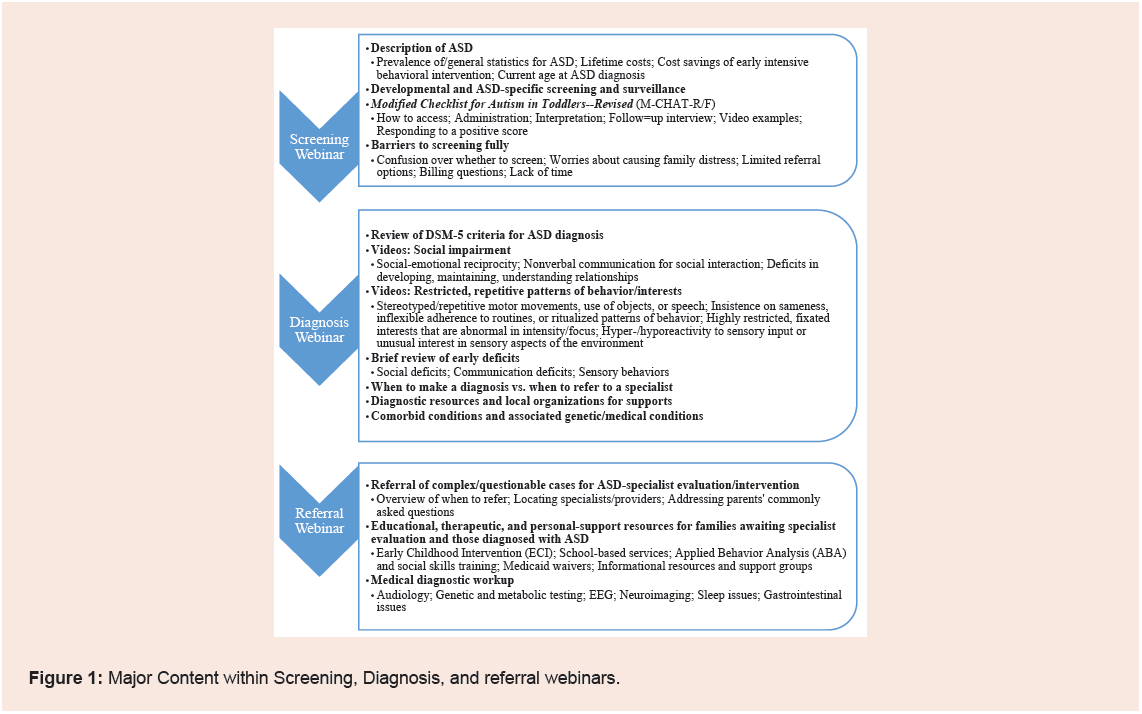
young children. An overview of the content for each webinar is in
Figure 1. The webinar series was hosted on Diagnose First’s web-based
platform, which required users to request a free, unique login
to access the site’s content. Each webinar was self-paced, lasted
approximately one hour, and conferred one hour of continuing
medical education (CME) credit, as approved through the hospital’s
Office of Continuing Medical Education.Electronic pre- and post-webinar questionnaires were developed
by the study team and embedded within each webinar. Each
questionnaire contained 10 items, three of which assessed potential
changes inself-reported knowledge of and confidence in ASDscreening,
-diagnosis, and -referral practices. Response options
to these items were on a four-point Likert-type scale ranging from
“1-Not at all” to “-Extremely,” with higher scores indicating greater
knowledge/confidence. The remaining items on each survey queried other content presented in each webinar; because these content items
were not part of a validated instrument, they were collected to inform
future efforts only. Pre- and post-survey items for each webinar
were identical, yet item wording was tailored to match the webinar’s
topic (Screening, Diagnosis, or Referral). Additionally, post-test
questionnaires included open-ended text boxes for provision of
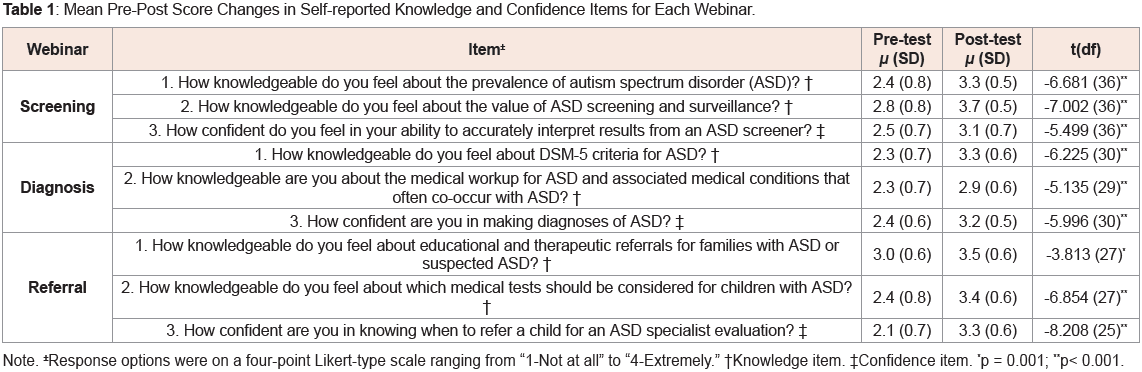
optional feedback. Table 1 contains the self-reported knowledge and
confidence items that were the primary focus of this study.
Table 1: Mean Pre-Post Score Changes in Self-reported Knowledge and Confidence Items for Each Webinar.
Procedure:
Potential participants received an initial email invitation,
followed by up to three reminder emails at two-week intervals. Each
invite/reminder email included instructions for requesting their
unique login information to access the webinar website. Once logged
in, participants were authorized to view the Screening, Diagnosis, and
Referral webinars, with controls enabled that mandated their viewing
in that order because content built on the preceding webinar. Before
and after each webinar, participants received the pre- and post-test
questionnaires; a participant could not view a given webinar without
first completing the pre-test for that webinar. Likewise, a participant
must have completed the prior webinar’s post-test in order to access
the next webinar’s pre-test. Following completion of each post-test
questionnaire, participants had the option to print a CME certificate.
Once participants completed the Referral post-test, they could
download and/or print the entire webinar series for future reference.
Overall, we designed the participation process to mimic training
opportunities outside the context of research, where institutional
mandates and monetary incentives are typically not encountered.To compare pre-post changes across all self-reported knowledge
and confidence scores for each webinar, paired-samples t-tests were
used, as these were ordinal variables with no “right” versus “wrong”
responses. Participants’ open-ended feedback was initially reviewed
for possible thematic analysis; however, because of the brevity
of these responses and clear emotional valence, content analysis
was applied to categorize participants’ statements as positive (i.e.,
praised/found value) [27], negative (i.e., criticized/disagreed with),
constructive (i.e., provided recommendations), and/or neutral (i.e.,
impartial comment). If a statement included more than one type of
content, then it was classified in each appropriate category (i.e., a
statement could have both positive and constructive components and
be counted in each of these categories).
Results
Overall, 37/288 providers (12.8%) completed the Screening
webinar; 31/288 providers (10.8%) completed the Diagnosis webinar;
and 28/288 (9.7%) providers competed the Referral webinar.
However, even in this small sample, paired samples t-tests revealed
statistically significant pre-post increases (p ≤ .001) across all selfreported
knowledge and confidence scores for each webinar (see
Table 1). Similarly, disagreement with the statement that “Only
specialists are able to diagnose ASD, and primary care providers do
not have the training to make an accurate diagnosis,” significantly
increased from pre- to post-test (t[29] = -2.757, p = 0.01).
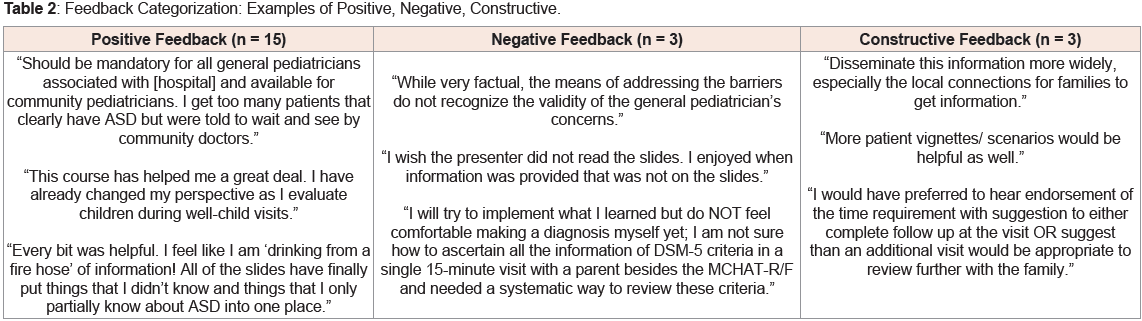
A total of 19 PPCPs provided open-ended feedback about the
webinars; 15 (78.9%) included positive sentiments. Three responses
(15.8%) contained negative feedback; five (26.3%), constructive
feedback; and three (15.8%), neutral feedback (see examples in Table 2). One participant recommended that the webinar series, “…should
be mandatory for all general pediatricians associated with [hospital],”
and two participants recommended broader distribution of the
webinars to community pediatricians. Four participants requested a
page of resources (e.g., .pdf or Word document), and one requested a
copy of the slides. Two of the comments categorized as neutral were
related to technical issues and one was a comment about Epic (the
electronic health record [EHR] used by the network of practices).
In terms of the most helpful content/information in each webinar,
the most common responses were (a) M-CHAT-R/F follow-up
interview for the Screening webinar (50.0%); (b) videos contrasting
neurotypical/atypical behaviors for the Diagnosis webinar (57.1%);
and (c) testing/medical workup (57.1%) and referral resources
(57.1%) for the Referral webinar.
Discussion
We created an online educational program to educate PPCPs on
ASD-screening, diagnosis, and referral practices and then evaluated
provider use, acceptability, and potential improvements in PPCPs’ selfreported
knowledge and confidence about these practices following
their participation. An important observation with respect to use
was the low response rate. Our research design (a) included multiple
reminders as a means to encourage participation; (b) extended
recruitment beyond the targeted study-close date; (c) incentivized
participants with one hour of CME credit per webinar; and (d) enabled
downloading of each webinar as a take-away resource. We selected
a study design that mimicked real-world training opportunities,
with no institutional requirements to complete the webinars and no
financial incentives-essentially, an “if you build it, they will come”
approach. Despite efforts to increase participation rates, our sample
size remained small. This is particularly notable because those in the
integrated primary care clinic specifically requested training in ASD
diagnosis, yet only a handful participated. It is possible that many
providers simply could not find the time, as pediatricians frequently
report time constraints as barriers to providing ASD-specific support
and care. Additionally, the requirement to complete all aspects of
the previous webinar (i.e., pre-post measurements) before accessing
the next webinar may have deterred PPCPs from completing the
series. Although we included this requirement so that our content
sequentially built upon itself to reinforce key messages and align
with clinical practice (i.e., screening diagnosis referral), it may have
exasperated providers who were only interested in specific content
materials (i.e., referral information, medical workup). It also limited
our pool of participants for the Diagnosis and Referral webinars to
those who completed the Screening webinar. This is an important take
away, as many providers want more information about ASD (Carbone
et al., 2020), which emphasizes a critical need to understand how
providers want to receive this information. Interestingly, there was
relatively little drop off in participation from one webinar to the next;
31/37 (83.7%) who participated in the Screening webinar completed
the Diagnosis webinar, and 28/31 (90.3%) who participated in the
Diagnosis webinar completed the Referral webinar. Such continued
engagement may reflect providers’ acceptability of the series once
they began; though it is also likely that those who began the series in
the first place were those most interested in the content offered [28].
Despite our relatively small sample, results demonstrated that a brief (i.e., three 1-hour sessions) and convenient (i.e., self-paced and
available on-demand) webinar series on ASD screening, diagnosis,
and referral may be an effective way to educate PPCPs on these topics.
Participants showed measurable gains in self ratings of knowledge
and confidence in managing ASD following each of the webinars.
Also, more providers moved from thinking that only specialists could
diagnose ASD to recognizing that PPCPs could make the diagnosis
themselves. This is encouraging, as some providers who may have felt
that ASD diagnoses were out of their scope of practice may now feel
empowered to make the diagnosis in clear cases, thereby expediting
families’ next steps in accessing intervention services. Earlier research
suggested that, compared to other medical specialists who may
commonly see individuals with ASD (e.g., psychiatrists), PPCPs did
not differ in their knowledge about DSM criteria for ASD (Heidgerken
et al., 2005). Therefore, it is possible that providing information that
enhances PPCP confidence in their application of this knowledge
could facilitate clinical actions that lead to earlier ASD diagnoses
Among those who offered open-ended feedback, most of their
comments were complimentary, with many pointing out that the
materials were helpful, informative, and should be made available to
other pediatricians. Information about the M-CHAT-R/F follow-up
interview, videos in the Diagnosis webinar, and guidance regarding
medical workup and referrals were cited as the most valuable aspects.
PPCPs’ preference for diagnostic information and referral practices
are consistent with previously reported learning collaboratives
[6]. Interestingly, many PPCPs in this study indicated no prior
knowledge of the follow-up interview and/or a desire for more
information on how to obtain/administer it. While the M-CHATR/
F was always intended as a two-part screener [29], the majority of
pediatricians do not use the follow-up interview [8]. It is not clear
how this interview becomes separated from the initial screening
questions during clinical implementation, but our results suggest an
interest among some PPCPs to include it in their screening practices.
Pediatric clinics should evaluate whether they currently support
follow-up practices that enhance specificity of ASD-screening tools,
which may subsequently help providers feel more confident in their
referral actions.
Constructive and negative comments shared by participants
provided important considerations for future work to enhance/expand
educational tools and increase providers’ engagement in training.
A few participants made specific recommendations for improving
content, as well as shared their hesitation about implementing the
follow-up interview after a positive screen; both should be addressed
in updates to the webinars prior to subsequent distribution. The
recommendations to make the webinars more widely accessible
suggest that developing template presentations with information
tailored to a specific locale may increase generalizability and utility.
Additionally, participants were given the option to download and use
the webinar slides as a reference or resource for families they serve;
however, some may not have realized that they had this option, so
clarifying this feature and/or providing some instructions on this
process may be helpful [30-33].
Limitations and Future Directions
While this pilot study demonstrated the utility of an educational
webinar series for enhancing PPCPs’ knowledge and confidence in ASD-screening, diagnostic, and referral practices, there are
limitations to note. One is that our response rate was low; rendering a
relatively small sample that may not be reflective of the broader group
of PPCPs in the sampling pool. Notably, this study was conducted
prior to the onset of the COVID-19 pandemic, and it is possible that
learning preferences may be different now in the wake of increased
reliance on/familiarity with remote-engagement platforms. A second
limitation is that our questionnaires were not validated tools and were
designed to be extremely brief to encourage participant retention;
as such, they were limited in their range of content and likely do
not reflect a comprehensive assessment of what PPCPs learned
about ASD. A review of literature that included assessment of ASD
knowledge revealed no standardized approach or strong measure
of this construct, and there is a need for improved tools that are
cross-culturally relevant with corresponding content [11]. For this
reason, our focus in the current study was on PPCPs’ self-reported
knowledge and confidence ratings in the management of ASD.
Fourth, we do not know whether participation in the webinars led
to changes in providers’ screening, diagnostic, and referral behaviors
in their practices, although we intend to examine these actions in
subsequent work. Previous research in health professions suggests
that knowing does not always give rise to doing [17]. Therefore,
educational strategies alone may be insufficient to prompt changes in
practice. However, other research has observed changes in screening
and referral practices after educational interventions, such as ECHO
Autism [22]. As such, it will be valuable to follow the screening,
diagnostic, and referral practices of PPCP participants and compare
those to the practices of non-participant providers in the network.
Finally, our solicitation of open-ended feedback about the webinars
yielded brief comments from a relatively small number of PPCPs.
It is possible that a different methodological approach (e.g., indepth
interviews, focus groups) would yield data for more intensive
investigation of PPCPs’ experiences/recommendations regarding
provider education/training in the identification and management of
ASD.
Considering that participating PPCPs demonstrated important
self-reported knowledge and confidence gains as a result of their
participation in the webinars, further research should (a) explore
and compare the utility, acceptability, and efficacy of alternate ASDtraining
platforms for PPCPs; (b) develop and include validated
measures of ASD knowledge; (c) longitudinally assess potential
changes in PPCPs’ clinical practices following their participation
in educational/training opportunities; and (d) investigate the
acceptability of in-clinic supports (e.g., a best practice advisory),
in concert with educational opportunities, to remind providers
of appropriate courses of action at the point-of-care. Because the
response rate to participate in our webinar series was low, alternate
approaches to disseminating webinar content should also be explored
to provide more acceptable, on-the-go training opportunities that
providers can tailor to more precisely meet their educational needs.
Summary & Conclusion
Understanding PPCPs’ Knowledge of and Confidence in ASD
screening, diagnosis, and referral practices may allow behavioral health
professionals (e.g., psychologists, school-based personnel)
to collaborate more effectively with PPCPs by streamlining referral processes for ASD evaluation and facilitating earlier connections
with intervention services that ultimately stand to improve children’s
developmental outcomes. Our pilot findings highlight the promise of
a brief, webinar-based approach for improving PPCPs’ self-reported
ASD-care knowledge, as well as the need for more accessible, effective
educational tools and supports for PPCPs that will help close the
ASD-detection gap and provide immediate provisions for affected
children and their families.
Acknowledgement
This research was supported by a gift from the William Stamps
Farish Foundation to Dr. Goin-Kochel. Research reported in this
publication was also supported by the Eunice Kennedy Shriver
National Institute of Child Health & Human Development of the
National Institutes of Health under Award Number 1U54 HD083092
for partial support of Drs. Goin-Kochel’s and Ahmad’s effort. The
content is solely the responsibility of the authors and does not
necessarily represent the official views of the National Institutes of
Health. We wish to thank all of the providers who participated in
this project; Dr. Stan Spinner for his assistance with the recruitment
efforts and overall support of our research program; and the team at
Diagnose First for building and refining the webinar platform, as well
as their permission to use videos from their extensive library.