Journal of Pediatrics & Child Care
Download PDF
Research Article
Allergic Rhinitis and Asthma in Association with Fungal Pollution of Indoor Environments
Sibi Das1*, Sethi Das C2, Silvanose C3 and Jibin VG4
1Sri Siddhartha Medical College, Tumkuru, Karnataka, India
2Aster CMI Hospital, Bengaluru, India
3Laboratory Manager, Dubai Falcon Hospital, Dubai, UAE
4Pediatrics Department, District Hospital, Bundi, Rajasthan, India
*Address for Correspondence:
Sibi D, Sri Siddhartha Medical College, Tumkuru, Karnataka,
India; E-mail: sdsilvanose@gmail.com
Submission: 23 January, 2023
Accepted: 03 March, 2023
Published: 06 March, 2023
Copyright: © 2023 Sibi D, et al. This is an open access article
distributed under the Creative Commons Attr-ibution License,
which permits unrestricted use, distribution, and reproduction
in any medium, provided the original work is properly cited.
Abstract
Allergy or asthma is triggered by inhaling allergens such
as dust, mites, pet dander, pollens, and fungal molds. Samples
were collected from various indoor environments including
air conditioner filters, carpets, indoor plant soil, living room air,
and pillow covers of residents living in air-conditioned flats for
screening the fungal pollution of indoor environments and their
role in allergies and asthma. This study included 30 residents with
school-aged children suffering from allergies or asthma and
a healthy control group of another 20 other residential indoor
environments. The fungi isolated from indoor environments include
Aspergillus niger, A. nidulans, A. flavus, A. fumigatus, Alternaria
sp., Paeciliomyces species, Bipolaris species, Trichophyton
verrucosum, and T. rubrum. Aspergillus species were isolated from
all environments while Trichophyton species were only isolated
from indoor plant soil. The fungal presence was higher in the
indoor environments of group 1 with allergic rhinitis and asthma
with a significant p-value <0.00001 showing its role in allergic
rhinitis when compared the group 2 without allergy or asthma.
The children suffering from allergies and asthma were further
grouped into intermittent (70%), persistent (13%), and asthma or
allergic asthma (17%) cases based on symptoms and duration.
For the treatment of intermittent allergic rhinitis, a combination of
oral antihistamines, and nasal decongestants were used, while
persistent allergy symptoms were treated with corticosteroids
(oral/intranasal), oral antihistamines, and oral leukotriene receptor
antagonists. Asthma cases were treated with salbutamol sulfate,
a bronchodilator, and oral leukotriene receptor antagonists
with a combination of antiallergic treatments. A combination of
treatments with improved indoor hygiene showed better relief for
allergic rhinitis and asthma and was significantly reduced from
persistent symptoms to intermittent or recovered from allergic
symptoms.
Keywords
Allergic rhinitis; Asthma; Aspergillus species; Antihistamine;
Corticosteroid; leukotriene
Introduction
Rhinitis is a condition that involves nasal inflammation and is
characterized by recurrent sneezing, a runny nose, itchy eyes, and
nasal congestion that can disrupt sleep. It may also increase the
risk of other conditions, such as sinusitis and asthma, as these are
common comorbidities associated with allergic rhinitis. Rhinitis can
be caused by infections or inhaled allergens, such as dust, pet dander,
dust mites, fungal molds, and pollens. However, allergic rhinitis is
a hypersensitivity response to a variety of inhaled environmental
allergens and is characterized by rhinorrhea, nasal congestion,
itching of the nose, and sneezing [1,2]. When allergens are inhaled,
they encounter the nasal mucosa and diffuse into nasal tissues. In
recent years, evidence of the links between rhinitis and asthma has
been strengthened, and their strong correlation may be explained by
the theory of the unified airway, which suggests that upper and lower
airway inflammation share common pathophysiologic mechanisms,
coexist, and communicate via systemic circulation [3,4].
Allergic rhinitis is a chronic respiratory tract condition that can
significantly affect a patient’s quality of life. The clinical expression of
the disease is the result of a cascade of immunological and biochemical
events. It is estimated that more than 400 million people worldwide
are affected by allergic rhinitis, which includes 10-30% of adults
and 40% of children. Among them, 71% of patients are triggered by
environmental factors [1,5,6]. Home environmental assessments can
be valuable tools for the comprehensive management of asthmatic
and allergic diseases. Indoor structures can harbor allergens,
making the home a primary target for allergens. Fungi are one of
the allergens that tend to inhabit areas with high moisture content
and low light levels [7]. Allergic rhinitis and asthma are both chronic
inflammatory disorders, with overlapping epidemiology and sharing
some treatment approaches [8,9]. This study aims to evaluate the
level and biodiversity of fungi in indoor environments, their role in
allergic rhinitis and asthma, and to review current treatment options
and management.
Materials & Methods
This study was conducted in fifty indoor environments of
residents living in air-conditioned multistoried buildings in Dubai,
United Arab Emirates to assess the indoor fungal presence. It
includes 30 residents with children 5 to 12 years with allergic rhinitis
or asthma and 20 with healthy children without allergic rhinitis or
asthma. Samples were collected from air conditioner filters, carpets,
indoor plant soil, pillow covers, and indoor air using an air sampler
and transported to the microbiology lab for fungal culture and
identification. The fungal colonies were counted and identified by
cultural characteristics and morphology of hyphae and spores under
microscopy using lactophenol aniline blue stain.
A survey was done to assess the children having any type of
allergy or asthma and recorded the details of clinical diagnosis and
treatment from clinics or hospitals prescribed by a pediatrician. The
samples collected from the healthy group were included in Group 2
and those who suffer from allergies were included in Group 1, based on the symptoms and duration of the diseases sub-categorized into
intermittent, persistent, and asthma or allergic asthma cases. A
follow-up screening was performed after 3 months with improved
conditions such as weekly cleaning of air condition filters, indoor
air purification with a HEPA filter air purifier, frequent change of
bedding, and removal of indoor plants from the living room.
Results
The symptoms of allergic rhinitis were rhinorrhea, nasal
congestion, itching of the nose, and sneezing. Allergic rhinitis was
further sub-grouped into intermittent (70%), characterized by
allergic symptoms ≤ 3 days in a week; persistent (13%), characterized
by allergic symptoms >3 days a week with disturbed sleep and lack
of regular activity, or if symptoms persist >4 consecutive weeks.
Asthma or allergic asthma cases (17%) were together as they have a
similar treatment approach. Common asthma signs and symptoms in
children include coughing, particularly at night, wheezing, breathing
difficulty, chest tightness, or discomfort.
The main difference between intermittent and persistent allergic
rhinitis was the frequency, degree, and duration of symptoms. Both
types of allergic rhinitis shared some similarities in symptoms,
while there were also differences in the severity of symptoms and
their impact on daily life. Symptoms of intermittent allergic rhinitis
include sneezing, runny nose, nasal congestion, and itchy or watery
eyes. Persistent allergic rhinitis had these same symptoms, with
additional symptoms noticed as sore throat, coughing, and fatigue.
The symptoms of intermittent allergic rhinitis were generally less
severe than those of persistent allergic rhinitis and lasted for a short
period of time. In contrast, persistent allergic rhinitis symptoms were
more severe and lasted for weeks or even months in some cases. This
can have a significant impact on quality of life. Intermittent allergic
rhinitis was not severe enough to impact daily life. On the other
hand, persistent allergic rhinitis had a significant impact on daily life,
making it difficult to carry out daily activities.
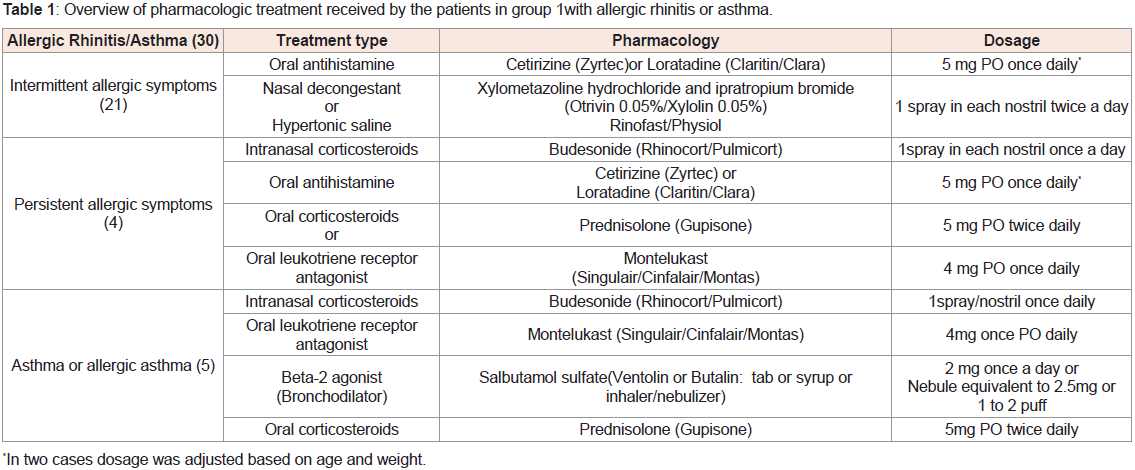
All children in the survey were between 5 and 12 years old, and
the treatments they received from various pediatric clinics were
documented and summarized in Table 1. Treatment for intermittent allergic rhinitis includes a combination of oral antihistamines and
nasal decongestants, while persistent allergy symptoms are treated
with corticosteroids (oral/intranasal), oral antihistamines, and oral
leukotriene receptor antagonists. Asthma cases are treated with
salbutamol sulfate, a bronchodilator, and oral leukotriene receptor
antagonists, in combination with antiallergic treatments.
Table 1: Overview of pharmacologic treatment received by the patients in group 1with allergic rhinitis or asthma.
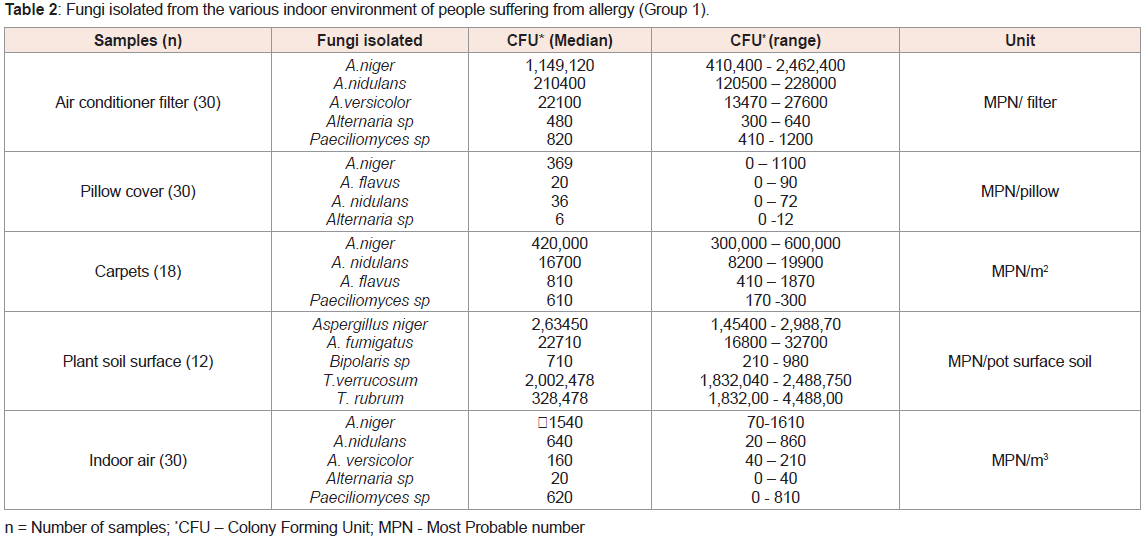
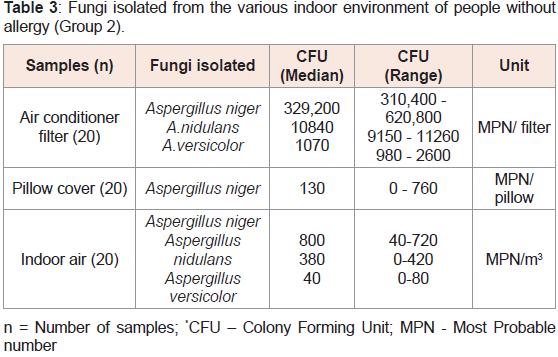
Table 2 presents the fungi isolated from various indoor
environments of people suffering from allergy or asthma (Group 1),
while Table 3 shows fungi isolated from various indoor environments
of people without allergy or asthma (Group 2). In Group 2, residents
did not use carpets and did not have indoor plants. The presence of
fungi in the indoor environments of Group 1 was significantly higher
(p-value <0.00001) than in Group 2, demonstrating its role in allergic
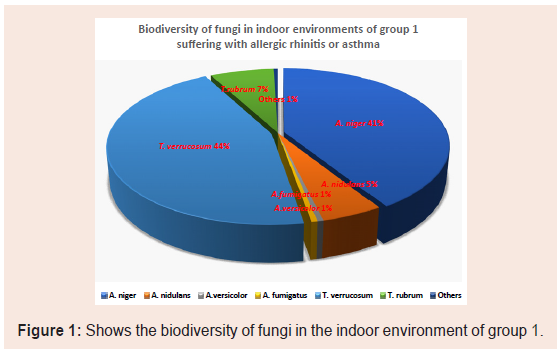
rhinitis compared to those without allergies. Figure 1 illustrates the
biodiversity of fungi in the indoor environment of Group 1.
Table 2: Fungi isolated from the various indoor environment of people suffering from allergy (Group 1).
A follow-up study recorded all cases of allergic rhinitis and asthma
were either reduced from persistent to intermittent or completely
recovered.
Discussion
Allergic rhinitis is a prevalent health problem that affects up to
40% of the global population, with higher rates among children [1,5].
Individuals with severe and persistent rhinitis are at greater risk of
developing asthma, which can cause chest tightness, breathlessness,
and nocturnal coughing [8,11]. Both allergies and asthma can be
triggered by inhaling common allergens such as dust, pet dander,
mites, pollens, and mold. Previous studies have shown that the
biodiversity of fungi in indoor environments varies depending on
climatic conditions like temperature and humidity [7,10]. Aspergillus
species were frequently found in the air conditioning filters of
hospitals, schools, cars, and homes, while Trichophyton species are
common in soil and indoor plant soil [7,10,12,13]. The incidence of
fungi was higher in Group 1, particularly in indoor plant soil, A.C.
filters, and carpets, and the fungal colonization may contribute to
allergic rhinitis or trigger allergy symptoms in residents.
Allergy to fungal spores is an immune response that occurs when the body’s immune system overreacts to the presence of these
spores. When the fungal spores are inhaled, the immune cells called
dendritic cells capture them and present them to T-helper cells.
The T cells activate B-cells and produce specific antibodies called
Immunoglobulin E (IgE) against the spores, and that will bind
to mast cells and basophils. The activated mast cells and basophils release inflammatory mediators, such as histamine, leukotrienes,
and prostaglandins. These mediators cause allergy symptoms such
as swelling, itching, and mucus production. In response to the
inflammatory mediators, other immune cells, such as eosinophils
and neutrophils, are recruited to the site of the immune response.
These cells release additional inflammatory molecules and enzymes
that cause tissue damage and exacerbate the allergic reaction [14-16]. Similarly, exposure to fungal spores can trigger an asthma attack
in some people, leading to symptoms such as wheezing, coughing,
chest tightness, and difficulty breathing. Individuals with allergies
or asthma should be especially vigilant in monitoring and managing
indoor air quality to reduce the risk of exacerbating their symptoms
[17].
The pathologic features of allergic rhinitis and asthma have many
similarities as both conditions involve the activation of CD4+ T cells,
eosinophils, and mast cells by allergens [3,8,11]. The immediate
allergic reaction is coordinated by mast cells, and their mediators,
histamines, and leukotrienes are responsible for causing the
symptoms of allergic rhinitis, including smooth muscle constriction
and mucus secretion [3,8]. Second-generation antihistamines are
preferred treatment options in children as they are considered safe
and have less sedation compared to older antihistamines [9]. They
are highly effective at relieving the symptoms of histamine-mediated
allergic rhinitis, such as sneezing, itching, and runny nose. Intranasal
antihistamines have advantages over oral antihistamines as they
provide a higher concentration of medication to a specific, targeted
area with fewer adverse effects [9].
Allergic rhinitis and asthma are often associated, and the two
disorders interact at various levels, with rhinitis typically preceding
the development of asthma. The presence and type of asthma will be
influenced by sensitization and the duration and severity of allergic
rhinitis. A study found that 78% of asthma patients have allergic
rhinitis, while 38% of allergic rhinitis patients have asthma, showing
that persistent allergic rhinitis may develop into asthma [8]. Once the diagnosis is confirmed, the next step is to identify the allergen and
reduce the patient’s exposure to allergens. Medical treatment must
also be to manage the symptoms of allergic rhinitis, such as nasal
blockage, itchiness, and sneezing. These nasal medications are steroid
sprays for the nose, which could be taken regularly over periods, and
oral antihistamine medications to alleviate all symptoms of allergic
rhinitis. Since allergic rhinitis and asthma are inflammatory disorders
with similar pathophysiology, they also share common treatment
approaches, steroids being the mainstay of treatment for both.
The treatment options for allergic rhinitis include intranasal
corticosteroids, oral and topical antihistamines, decongestants,
intranasal anticholinergics, and leukotriene receptor antagonists.
Intranasal corticosteroids are effective as a first-line therapy for mild
to moderate disease. Second-line therapies, including antihistamines,
decongestants, and leukotriene receptor antagonists, are used for
moderate to severe disease [9,11]. In a study using budesonide nasal
corticosteroid spray for allergic rhinitis, it was found that nasal
corticosteroids are effective with or without antihistamines in the
treatment of the condition. Glucocorticoid nasal sprays are presently
the most effective single-agent maintenance therapy for allergic
rhinitis and cause very few side effects at the recommended doses. They
are particularly effective in relieving nasal congestion. Antihistamines
relieve the itching, sneezing, and runny nose of allergic rhinitis but do
not relieve nasal congestion. Antihistamines are available in a nasal
spray or oral formulation such as tablets or syrup.
Leukotrienes are another mediator and play a crucial role in
allergic rhinitis and asthma by causing airway muscle constriction,
leading to breathing difficulties, and increased mucus production.
Montelukast, a leukotriene LTD4 receptor antagonist, is an effective
treatment option for moderate to severe persistent symptoms of
allergic rhinitis with asthma and can be used in combination with
intranasal corticosteroids or antihistamines [4,8,9,11].
Asthma is a respiratory disease characterized by inflammation
and bronchospasm, different from allergies. It is not necessary to have
people with asthma who always have allergies. Airway inflammation
is formed when the lining of the airways becomes swollen and
clogged with mucus and fluid. Bronchospasm is formed when the
muscles around the airways tighten and contract. These conditions
leave a patient with cough, wheezing, chest tightness, and shortness
of breath, and when breathing issues become severe, it is referred to
as an asthma attack [8,11]. A cough associated with allergic rhinitis
was noted with asthma. Allergic diseases may occur in those who
have an overactive immune system, and in some cases, the immune
response causes the airways to swell and overproduce mucus due to
an allergen and leading to allergy-induced asthma [8,11]. People with
allergic asthma experience the same symptoms as those with nonallergic
asthma, including coughing, wheezing, chest tightness, and
shortness of breath.
Conclusion
Aspergillus species were the most common fungi isolated from
the indoor environment while Trichophyton species were also
isolated from the plant soil surface. A high incidence of fungi was seen in the indoor environment of residents suffering from allergies
and asthma. Many therapeutic options are effective against allergic
rhinitis, including a combination of antihistamines, corticosteroids
(intranasal and oral), and anti-leukotrienes. The treatment efficiency
was improved with hygienic environmental conditions by avoiding
fungal contaminants which were the major trigger in indoor
environments.
Acknowledgment
The authors would like to thank Al Hayat Pharmaceuticals,
Sharjah, UAE for their cooperation in this study