Journal of Pediatrics & Child Care
Download PDF
Case Report
Hypertriglyceridemia Induced By L-Asparaginase and Prednisolone in Pediatric Hemato-Oncology: A Case Report
Goutham KJ2, Swathi J3, Nishit3, Deepti A2, Harika V2, Rekha B2, Priyank T2, Roshini DG3, Hanan P2, Anjali M3, Amey P3 and Sachin SJ1
1Hematology & SCT, HCG Cancer Hospital, Bangalore, India
2Clinical Pharmacology, HCG Cancer Hospital Bangalore, India
3Consultants, HCG Cancer Hospital, Bangalore, India
*Address for Correspondence:
Sachin SJ, Hematology & SCT, HCG Cancer Hospital,
Bangalore, India; Phone: 9741351357; E-mail: drsachin.
jadhav@hcgel.com
Submission: 11 May, 2022
Accepted: 24 June, 2022
Published: 29 June, 2022
Copyright: © 2022 Goutham KJ, et al. This is an open access
article distributed under the Creative Commons Attr-ibution
License, which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is
properly cited.
Abstract
Introduction: L-asparaginase and corticosteroids are widely used
in the chemotherapy of acute lymphoblastic leukemia (ALL). This
combination is known to cause several adverse effects one of which
is hypertriglyceridemia. Although the condition is asymptomatic and
reversible it can lead to serious complications.
Case description: This case report of 2-years 6 months old Indian
male baby who was on treatment for ALL on day 41 triglycerides levels
were 3324mg/dL with no significant symptoms, it was well managed,
and the triglyceride levels drop down to 117mg/dL without any
complications and interruption in the ongoing treatment.
Conclusion: Combination therapy of L-asparaginase and steroids
cause hypertriglyceridemia through various mechanisms leading to
various life-threatening complications. However, there are no standard
guidelines available to treat drug induced hypertriglyceridemia.
Frequent monitoring of serum levels may aid in early diagnosis,
prevents complications.
Introduction
L-asparaginase (ASP) has been a key component of the
chemotherapy regimens used for acute lymphocytic leukemia (ALL)
in children for 50 years. The combination of ASP with polyethylene
glycol (PEG-ASP) is a long-acting formulation with a half-life of 6
days which facilitate for intramuscular or intravenous administration
[1]. L-ASP and PEG are associated with various adverse effect
commonly fatigue, nausea, vomiting, thrombosis, hepatotoxicity,
hypersensitivity (clinical and subclinical), pancreatitis, thrombosis,
and very rarely hypertriglyceridemia [2]. The administration of
asparaginase can cause elevation of the triglyceride levels which is
generally seen in around 10% of ALL diagnosed children. Although
triglyceride level can hike in the adult patients receiving asparaginase,
it occurs most frequently among pediatrics in compared to
adults [2,3]. Asparaginase-induced hypertriglyceridemia can be
asymptomatic to symptomatic such as it shows symptoms like
transaminasemia, pancreatitis, and life-threatening thrombosis or
hyper-viscosity syndrome [4]. Nevertheless, most often the condition
is reversible and is rarely associated with complications [5]. Here
we report a rare case of PEG L-Asparaginase, and steroids induced
asymptomatic severe hypertriglyceridemia that is well managed
without any complications.
Case Report
A 2-years 6 months old Indian male baby (height 88cm, weight
13.1kg) presented with complaints of bilateral leg pain in the last 6
months, an inability to walk in the past 8 days and pain in abdomen from 5-6 days. On laboratory investigation: the complete blood count
showed pancytopenia with atypical cells on the peripheral smear,
Bone marrow aspiration smear showed 78% blasts with features of
acute leukemia (FAB-L1 classification), Marrow flow cytometry
showed B-ALL and CALL positive. Further an abnormal karyotyping
was observed with t (1:9) (q 21; p13) and I (9) (q 10) trisomy of
9q [hyper diploidy and del (9) (p)] whereas liver function, serum
glucose, thyroid function test and serum cholesterol were within
normal limits. Considering above findings, Patient was planned to
start on protocol 1 A pred (1AP) AIEOP BFM 2017, which includes
tablet prednisolone (20mg/m2)10mg PO TID daily [from D1-D28]
along with vincristine (1.5mg/m2) 0.8mg IV push with a running
NS on a three way and daunorubicin (30mg/m2) 16mg in 100ml
NS IV over 1 hour [each four doses- D8, D15, D22, D29], peg-LAsparaginase
(2500IU/m2/dose) 1335 IU in 100ml NS IV over 2
hours i.e., two doses on- D12 & D26. During the therapy, Liver
function was assessed before each dose of peg-L-asparaginase and
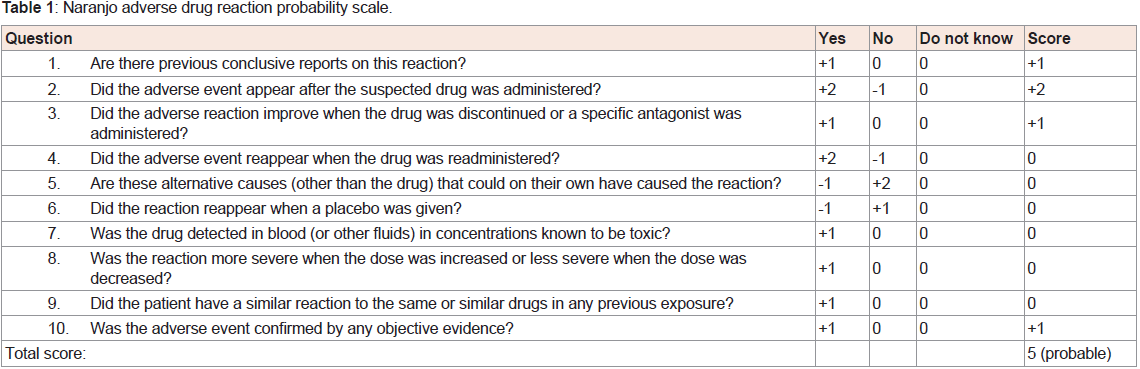
random blood glucose was measured daily. On day 41 blood sample
collected in EDTA tubes for routine blood investigation appeared
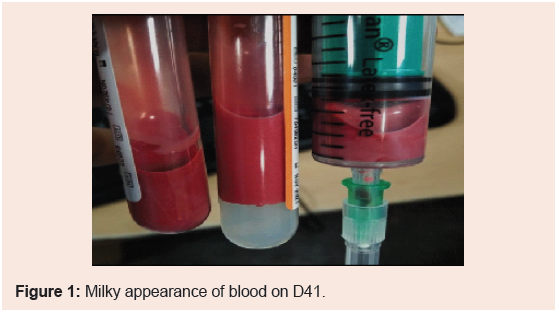
to be milky (Figure 1). Further investigation showed elevated triglyceride level to 3324 mg/dl and Naranjo ADR probability scale
used for causality assessment (Table 1). The case was interpreted
as possible case of Peg- L- Asparaginase and prednisolone induced
hypertriglyceridemia with causality assessment score of 4. Despite of
this life-threatening condition, patient triglyceride level gradually fall
back to normal within 2 weeks (1st day: 3324 mg/dl, 3rd day: 1458 mg/
dl, 14th day: 117 mg/dl) secondary to strict diet modification (<20%
low fat diet) without any drug based treatment approach. Patient
doesn’t experience any complications due to elevated triglyceride.
Patient received further treatment and was discharged.
Discussion
Peg-L-asparaginase or L asparaginase is an effective drug in
childhood acute lymphoblastic leukemia (ALL) and it has become an
important component of most childhood ALL treatment regimens
during induction, intensification, and maintenance phases of therapy
[6]. It is known that asparaginase in combination with steroids results
in massive elevation of triglycerides leading to hypertriglyceridemia.
The ADR may be dose dependent or time dependent [7].
Probable mechanisms through which asparaginase and
corticosteroid increase triglycerides in the body is through inhibition
of lipoprotein lipase i.e., TGs are cleared from the circulation by
endothelial cell lipoprotein lipase (LPL), which catabolises TGrich
particles (chylomicrons and VLDL) into fatty acids, and these
are then taken up by adipose tissue. Conversely, decreased LPL
activity causes elevated serum TGs. Decreased hepatic synthesis of
lipoprotein, increased synthesis of VLDL and Increased synthesis of
TG rich particles may be another explanation for increased TG levels
[4]. On the other hand, corticosteroids are also known as adipokinetic
agents which increases triglyceride synthesis and also increases the
activity of lipoprotein lipase [7], a key enzyme required for the
hydrolysis of triglycerides. When asparaginase and steroids are given
together, it is likely that triglyceride-rich lipoproteins are rapidly
formed but insufficiently cleared which can cause significant changes
in serum lipid levels [6]. Studies revealed that asparaginase inhibits
the activity of LPL [3]. If hypertriglyceridemia remains undiagnosed
or neglected can lead to severe complications (metabolic syndrome,
pancreatitis, stroke, peripheral artery disease, coronary artery
disease and carotid artery disease, thrombosis, osteonecrosis) [8],
hemophagocytic lymphohistiocytosis [9]. Discontinuation of culprit
drug is the prime attempt toward the management drug induced ADR is discontinuation of drug [10]. It is known that ADR will further
increase the treatment burden and may worsen the disease condition
[11]. But in our case lack of diagnosis at early-stage lead to drastic
increase in TGs levels i.e, 3324mg/dl which is after both the doses of
PEG L-Asparaginase. But this case was well managed with strict diet
modifications and regularly monitoring TGs levels.
Development of acute pancreatitis indicates severity of the
condition and permanently cessation of PEG L-Asparaginase [12].
Even though no standard guidelines on management of asparaginase
and steroids induced HTGs till date [7], Very few studies have
discussed on this regard. Hoogerbrugge N. et.al, reported similar
case of HTG induced by L-asparaginase and corticosteroids. So, the
treatment was delayed until plasma TGs levels lowered. Further,
while rechallenging of causative drugs to avoid cumulative effects
of steroids and asparaginase was given for subsequent doses after
steroids was stopped [3]. Studies have also treated the extreme
levels of TGs levels with Gemfibrozil 600 mg orally twice daily [2],
Gemfibrozil 1200 mg orally per day followed by fish oil 3600mg/day
and after 2 weeks fibrates were started [13], IV infusion of SMOFlipid
at 0.5 g/kg/day [14], plasmapheresis has been proven to decrease TGs
levels within few hours of administration [15].
Kimberly M Lau.et.al, mentioned about treatment
recommendations available i.e,
➢ If TGs < 1000mg/dl, continue asparaginase with frequent
monitoring for developing pancreatitis.
➢ If TGs > 1000mg/dl, recommend withholding asparaginase
until TGs levels normalise [2].
However, it is surprising to note that only 10% of the children
encounter with hypertriglyceridemia during the treatment of ALL,
studies should continue to grow for the exact reason of HTG associated
with PEG and corticosteroids leading to any specific mutations. On
no account in the previous literature conveyed about L-ASP/PEG
serum levels and extent of monitoring this is also a drawback of our
study. Moreover, practitioners should routinely do therapeutic drug
monitoring (TDM) of the causative drug that helps to guide therapy
decisions at early stage [2]. As seen in previous literature therapy
decisions were confined to each case basis.
Conclusion
Asparaginase is a lifesaving agent of all pediatric ALL protocols and is increasingly used to treat patients in combination with various
other agents. With many protocols incorporating prolonged and high
intensity asparaginase treatment, it is important that practitioners
should be aware of all possible treatment-related toxicities. Early
diagnosis, frequent monitoring of serum levels and management
of asparaginase toxicity will aid in promoting optimal treatment
outcomes without any discontinuation of therapy.
List of abbreviations
ADR= Adverse Drug Reaction, ALL= Acute Lymphoblastic
Leukemia, ASP = Asparaginase, D= Day, HTG= Hypertriglyceridemia,
LPL= Lipoprotein Lipase, PEG =Polyethylene Glycol, TDM
=Therapeutic Drug Monitoring, TGs= Triglycerides, TID= Thrice a
Day, VLDL= Very Low-Density Lipoprotein.