Journal of Pediatrics & Child Care
Download PDF
Case Report
Distal Femoral Physiolysis in a Myelomeningocele Patient - Early and Accurate Diagnosis
Martin AR1,2, Syros A2 and Payares-Lizano M1*
1Department of Orthopaedic Surgery, Nicklaus Children’s Hospital,
Miami, FL 33155, USA
2Miller School of Medicine, University of Miami, Miami, FL 33136,
USA
*Address for Correspondence:
Payares-Lizano M, Department of Orthopaedic Surgery,
Nicklaus Children’s Hospital, Miami, FL 33155, USA; E-mail: mpayaresmd@gmail.com
Submission: 09 September, 2021
Accepted: 04 May, 2022
Published: 09 May, 2022
Copyright: © 2022 Martin AR, et al. This is an open access
article distributed under the Creative Commons Attr-ibution
License, which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is
properly cited.
Abstract
Background: Neurogenic physiolysis is the spontaneous widening,
inflammation, and fracture of long bone physes in children with spinal
cord defects. This condition is also referred to as epiphysiolysis and is
often missed by parents and physicians alike due to the lack of typical
fracture symptoms like pain and deformity.
Case Presentation: We present the case of a 5-year-old lumbarlevel
myelomeningocele patient who presented to the emergency
department with edema, warmth, and erythema of the knee joint, and
was later found to have elevated inflammatory markers concerning
for infection. After a thorough workup helped to rule out infection and
other life-threatening illness, the patient was successfully treated for
physiolysis of the distal femur with cast immobilization.
Conclusions: General pediatricians and orthopaedic specialists
should remain vigilant in recognizing physiolysis in this patient
population. Missed or delayed diagnosis may lead to iatrogenic
harm and can have negative long-term effects on patient’s physical
development and independence.
Abbreviations
MMC - Myelomeningocele, HKAFO - Hip-knee-ankle-footorthosis,
PT - Physical therapy, ESR - Erythrocyte sedimentation rate,
CRP - C-reactive protein, AP - Anterior-posterior, MRI - Magnetic
resonance imaging
Introduction
Children with congenital spinal cord defects like
myelomeningocele (MMC) are often times paraplegic and insensate
in the lower extremities. Low bone mineral density and lack of pain
feedback put them at high risk of atraumatic fractures in the lower
extremities, seen in 10-30% of patients with myelomeningocele [1,2].
Spontaneous isolated long bone physeal fracture or physeal widening
in spina bifida patients, referred to as physiolysis or epiphysiolysis,
is thought to occur secondary to a combination of repetitive
microtrauma, musculoligamentous imbalance, and osteopenia
[3,4]. The proximal tibial and distal femoral physes are most often
affected. The most common presenting symptom is a painless, warm,
and swollen joint, oftentimes first noticed by a parent [2,3,5]. These
patients, and their parents, often do not recall any precipitating event.
The lack of pain and history of trauma not only delays diagnosis
but often leads to the misdiagnosis of infection, possibly subjecting
patients to iatrogenic harm secondary to invasive diagnostic tests,
as well as continued repetitive microtrauma due to the delayed
diagnosis [3]. The physeal widening seen on plain films of patients
with physiolysis is similar to that seen in patients with scurvy, rickets,
syphilis, and osteomyelitis [5,6]. Thus, early and accurate diagnosis
is important.
We present the case of a child with lower lumbar spina bifida
who presented with an atraumatic warm and swollen knee, found to have distal femoral physiolysis. Due to her lack of traumatic history,
compounded with joint swelling and redness, the initial workup was
for infection. This case demonstrates the importance of recognizing
the unique presentation physiolysis in patients with spina bifida and
avoiding a delayed or missed diagnosis.
Case Presentation
A 5-year-old female with a history of lower lumbar level
myelomeningocele had been followed in our multidisciplinary spina
bifida clinic since age 5 months. Her managed conditions included
hydrocephalus, bowel and bladder incontinence, and bilateral lower
extremity paralysis. She had been using a hip-knee-ankle-footorthosis
(HKAFO) since age 2 and was able to use a stander for short
periods during physical therapy (PT) but was otherwise wheelchairbound.
Due to the COVID-19 pandemic, her PT sessions had been
cancelled for several months prior to presentation. The patient’s
mother brought her into the pediatric emergency department over
the weekend with a chief complaint of left knee swelling noticed
that morning. There was no recent history of trauma or travel. On
exam, the left knee was moderately swollen with a large effusion,
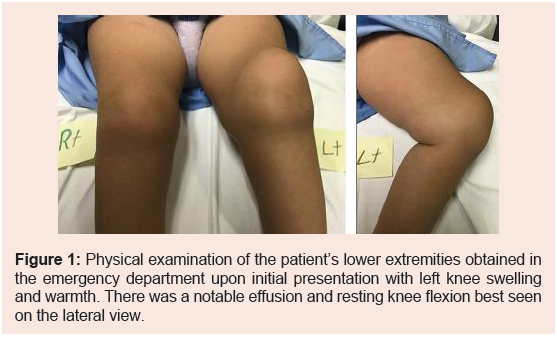
erythematous, and warm (Figure 1).
Figure 1: Physical examination of the patient’s lower extremities obtained in
the emergency department upon initial presentation with left knee swelling
and warmth. There was a notable effusion and resting knee flexion best seen
on the lateral view.
There was no sensation below the proximal thighs and no motor
function below the waste on bilateral lower extremities, as per baseline.
The knee was grossly stable on exam with full range of motion. Plain
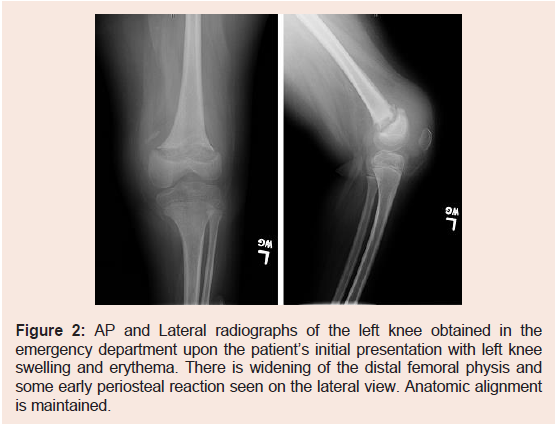
X-Ray films of the left knee demonstrated distal femoral physeal
widening and periosteal reaction (Figure 2).
Figure 2: AP and Lateral radiographs of the left knee obtained in the
emergency department upon the patient’s initial presentation with left knee
swelling and erythema. There is widening of the distal femoral physis and
some early periosteal reaction seen on the lateral view. Anatomic alignment
is maintained.
Vital signs and labs at that time were within normal limits. The
patient was placed into a long leg splint by the orthopaedic resident
on call and scheduled for outpatient follow up. Three days later,
the patient presented to the multidisciplinary spina bifida clinic for
follow up. She again was noted to have a painless large effusion of the
left knee. She was converted to a long leg cast and new x-rays were
obtained. There was noted to be no significant change in alignment
and osteolysis of the distal femoral physis with periosteal reaction.
Salter-Harris I fracture of the distal femur was suspected. Magnetic
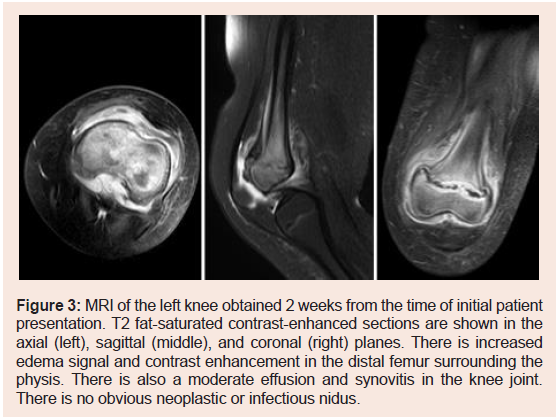
resonance imaging (MRI) of the left knee with and without contrast
was obtained 2 weeks from the time of presentation to further
delineate the process. MRI showed inflammation throughout the
distal femur and synovitis of the knee joint (Figure 3).
Figure 3: MRI of the left knee obtained 2 weeks from the time of initial patient
presentation. T2 fat-saturated contrast-enhanced sections are shown in the
axial (left), sagittal (middle), and coronal (right) planes. There is increased
edema signal and contrast enhancement in the distal femur surrounding the
physis. There is also a moderate effusion and synovitis in the knee joint.
There is no obvious neoplastic or infectious nidus.
Erythrocyte sedimentation rate at that time was elevated at 53
and C-reactive protein was borderline at 3, raising some concern for
infection. Knee arthrocentesis was performed and resulted in a normal
cell count and negative cultures. At this point, we had comfortably
ruled out the possibility of osteomyelitis or septic arthritis, and
the diagnosis was confirmed as left distal femoral physiolysis. The
patient was managed in well-padded cast immobilization of the left
lower extremity for 2 months and then was transitioned to a custom
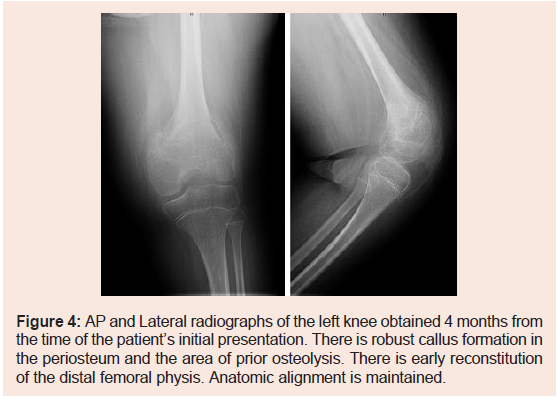
HKAFO for another month. X-rays obtained 4 months from the time
of onset demonstrated robust callus formation at the distal femoral
metaphysis and early reconstitution of the physis (Figure 4).
Figure 4: AP and Lateral radiographs of the left knee obtained 4 months from
the time of the patient’s initial presentation. There is robust callus formation in
the periosteum and the area of prior osteolysis. There is early reconstitution
of the distal femoral physis. Anatomic alignment is maintained.
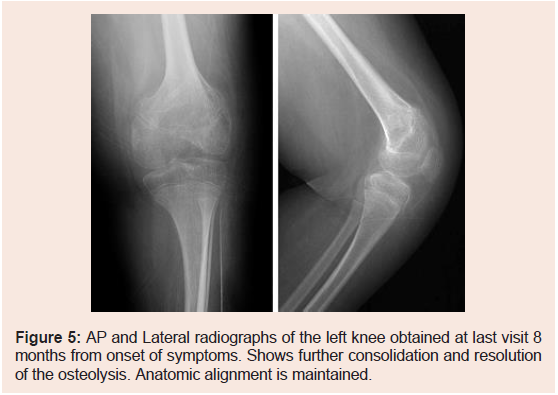
The patient was then cleared for return to routine physical
therapy without orthosis. At latest follow-up, 8 months after onset,
the patient was now 6 years old and was doing very well without any
recurrent left knee symptoms. Her function had returned to baseline.
Final X-rays demonstrated complete resolution of osteolysis, further
consolidation of callus, and maintenance of anatomic alignment
(Figure 5).
Discussion & Conclusion
The early recognition of physeal fractures in pediatric patients
with MMC spina bifida is crucial in improving patient outcomes
and avoiding long term consequences affecting their mobility and
independence [2,3,7]. The delayed recognition of injury by parents in
insensate patients can be further compounded by a physician’s missed or delayed diagnosis. This delayed diagnosis can turn relatively minor
injuries into unstable fractures due to repetitive microtrauma, which
can ultimately lead to complications such as premature physeal arrest,
angular deformity, or non-union [3,8]. Chronic stress on a fractured
physis can lead to physiolysis with widening and delayed healing,
which should be treated with immobilization of the extremity as
soon as possible [2,3]. Initial workup with plain radiographs is
the key in making the correct diagnosis, characterized by physeal
widening and periosteal reaction without angular or translational
deformity. However, these radiographic findings can often resemble
osteomyelitis or sarcoma, and should be closely monitored with serial
exams [2,7,9].
Furthermore, accurately diagnosing physiolysis in patients
with spina bifida is challenging due to the presentation of systemic
symptoms like fever, leukocytosis, and elevated inflammatory
markers (ESR, CRP), which often lead to the mistaken diagnosis of
cellulitis, osteomyelitis, or septic arthritis [2,3,10,11]. These symptoms
and lab findings typically resolve with immobilization and close
observation and should not always indicate advanced imaging or
invasive procedures like arthrocentesis. However, if patient follow-up
is limited, early and thorough diagnostic workup may be indicated to
rule out more severe, life-threatening disease. MRI with and without
gadolinium contrast can help identify the characteristic physeal
widening of physiolysis with islands of calcification, irregularity of
the zone of provisional calcification, and enhancement of the adjacent
epiphysis and metaphysic [8].
General pediatricians and orthopaedic specialists should remain
vigilant in recognizing the unique presentation of physiolysis in pediatric patients with spina bifida. Missed or delayed diagnosis may
lead to iatrogenic harm and can have negative long-term effects on
patient’s physical development and independence.