Journal of Pediatrics & Child Care
Download PDF
Research Article
*Address for Correspondence: James Nevin, Department of Emergency Medicine, Connecticut Children’s Medical Center, 282 Washington Street, Hartford, CT 06106; Tel: (203)470-1439; Fax: (860)545-9202; E-mail: jnevin21@gmail.com
Citation: Nevin J, Wilkens P, Smith S, Sturm J, Chicaiza H. Physical Exam and Historical Patient Factors Associated with Diagnosis of Pneumonia. J Pediatrics Child Care. 2015;1(1): 4.
Copyright © 2015 by Nevin et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Pediatrics & Child Care | ISSN: 2380-0534 | Volume: 1, Issue: 1Submission: 31 December 2014 | Accepted: 16 January 2015 | Published: 21 January 2015
Reviewed & Approved by: Dr. M. Olivia Titus, Associate Professor of Pediatrics, Medical University of South Carolina, USA
Of the 266 diagnosed with pneumonia, 91% (242) had a CXR. In comparison, only 13% (27/231) of patients in the control group without the diagnosis of pneumonia had a CXR. 80% (193) of the CXRs in the group diagnosed with pneumonia were interpreted as positive by a board certified pediatric radiologist (Figure 1). 7% (17) of the CXRs in the group diagnosed with pneumonia were interpreted as negative by a board certified pediatric radiologist (Figure 1).
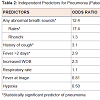
The following were significant independent predictors of physician diagnosed pneumonia controlled for whether or not a CXR was performed: abnormal breath sounds OR 12.4 (95% CI: 5.7-26.9), cough OR 3.1 (95% CI: 1.5 - 6.3), and duration of fever >2 days OR 2.9 (95% CI: 2.1-4.1) (Table 2). Tachypnea, fever at triage, retractions, and oxygen saturations below 95% were not associated with the diagnosis of pneumonia.
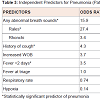
A sub-analysis of patients 5 years of age and older was also performed. The following were significant independent predictors of physician diagnosed pneumonia controlled for whether or not a CXR was performed: rales OR 27.4 (95% CI: 4.8, 93.0) history of chest pain OR 29.5 (95% CI: 6.8-127.2), abnormal breath sounds OR 15.9 (95% CI: 4.7-53.9), cough OR 4.31 (95% CI: 1.3-14.2), and duration of fever >2 days OR 3.5 (95% CI: 2.0-6.0) (Table 3). Tachypnea, retractions, and oxygen saturations below 95% were not associated with the diagnosis of pneumonia.
The independent predictors of pneumonia were similar between children 2 years to 18 years and those from birth to 2 years. Rales OR 13.7 (95% CI: 5.6, 33.7), any abnormal breath sounds OR 7.6 (95% CI: 4.5, 13.0), cough OR 3.5 (95%CI: 2.0, 6.2) and duration of fever greater than 2 days OR 2.3 (95% CI: 1.9, 2.9) were significant. In addition, tachypnea (respiratory rate greater than 95% for age) was also found as an independent predictor with OR 1.6 (95% CI: 1.03,2.35).
Physical Exam and Historical Patient Factors Associated with Diagnosis of Pneumonia
James Nevin1*, Paul Wilkens1, Sharon Smith1, Jesse Sturm1 and Henry Chicaiza2
- 1Department of Emergency Medicine, Connecticut Children’s Medical Center, Hartford, CT, USA
- 2Department of Pediatrics, Stony Brook Children’s Hospital, Stony Brook, NY, USA
*Address for Correspondence: James Nevin, Department of Emergency Medicine, Connecticut Children’s Medical Center, 282 Washington Street, Hartford, CT 06106; Tel: (203)470-1439; Fax: (860)545-9202; E-mail: jnevin21@gmail.com
Citation: Nevin J, Wilkens P, Smith S, Sturm J, Chicaiza H. Physical Exam and Historical Patient Factors Associated with Diagnosis of Pneumonia. J Pediatrics Child Care. 2015;1(1): 4.
Copyright © 2015 by Nevin et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Pediatrics & Child Care | ISSN: 2380-0534 | Volume: 1, Issue: 1Submission: 31 December 2014 | Accepted: 16 January 2015 | Published: 21 January 2015
Reviewed & Approved by: Dr. M. Olivia Titus, Associate Professor of Pediatrics, Medical University of South Carolina, USA
Abstract
Background: The use of chest radiography (CXR) to aid in the diagnosis of pneumonia varies among pediatric emergency physicians. Recent guidelines recommend clinical assessment to diagnose community-acquired pneumonia.Objective: To study the association between historical and physical exam findings in children who were diagnosed with pneumonia in the pediatric emergency department (PED).
Design/Methods: A retrospective chart review of patients (birth-18 years of age) who presented with symptoms suspicious for pneumonia in an urban PED was conducted between 01/01/10-12/31/11. Symptoms suggestive of pneumonia included chief complaints of fever, respiratory/difficulty breathing, or cough. Children were excluded if they had chronic lung diseases (i.e. asthma), and non-infectious etiologies (i.e. costochondritis). Children with a PED physician discharge diagnosis of pneumonia were compared to those with the same symptoms but without a diagnosis of pneumonia. Variables analyzed included: tachypnea, fever, duration of fever, chest pain, history of cough, any retractions, oxygen saturation, and physician documented abnormal breath sounds. Chi-square analysis was performed and a logistic regression model was used. CXRs were interpreted by a board certified pediatric radiologist.
Results: 497 children met inclusion criteria (51% female, 31% Caucasian, mean age 5.8 yrs). 266 children with a diagnosis of pneumonia were compared to 231 without. 91% (242/266) of those diagnosed with pneumonia had a CXR compared to 13% (27/231) without. The following were significant independent predictors of physician diagnosed pneumonia controlled for CXR performed: abnormal breath sounds OR 12.4 (95% CI: 5.7-26.9), cough OR 3.1 (95% CI: 1.5-6.3), and duration of fever >2 days OR 2.9 (95% CI: 2.0-4.1). Tachypnea, retractions, and oxygen saturations below 95% were not associated with the diagnosis of pneumonia. In children 5 years and older chest pain was a significant predictor with OR 29.5 (95% CI: 6.8-127.2).
Conclusion: Clinical predictors of pneumonia for children 2 years and older included abnormal breath sounds, cough, and fever > 2 days. Chest pain was also a significant predictor in children older than 5 years.
Keywords
Pneumonia; Chest radiograph; Pediatric emergency departmentAbbreviations
PED: Pediatric Emergency Department; CXR: Chest Radiography; CAP: Community-Acquired PneumoniaIntroduction
Community-acquired pneumonia (CAP) is a very common and serious illness in pediatric patients [1]. Emergency department physicians use a number of criteria to diagnose pneumonia, including clinical and epidemiologic data, findings on chest radiography, and laboratory tests [2,3]. Traditionally, features including cough, fever, wheezing, difficulty breathing, chest pain, and abdominal pain have been significant indicators of pneumonia, but there is disagreement as to their relative contribution to the diagnosis [2,4]. The reasons for this disparity can be due to the lack of a gold standard for the diagnosis of pneumonia, difficulties in identifying the subtle signs of pneumonia, and variability in the interpretation of chest radiographs [5].A chest radiograph has historically been a major contributor to the diagnosis of pneumonia in children. However, recent research has called into question the necessity of a chest radiograph due to the variability of interpretation and its inability to distinguish between the various microbiological causes [2,6-9]. Chest radiographs in patients suspected of having pneumonia are sometimes read as normal, and this can lead physicians to treat pneumonia regardless of radiologic findings [9]. One study showed that 21% of patients clinically diagnosed with community-acquired pneumonia had negative chest radiographs at presentation [7]. The Infectious Diseases Society of America (IDSA) guidelines for management of CAP in infants and children older than three months of age state that routine chest radiographs are not necessary for the confirmation of suspected CAP in patients well enough to be treated in the outpatient setting [6]. Moreover, chest radiographs are not without risk; though exposure to radiation from a chest radiograph is minimal, future cancer risk increases with the decreasing age of the child and the number of chest radiographs and other radiation exposures [10].
The aim of this study was to determine which signs or symptoms are most common in children who are diagnosed at a Pediatric Emergency Department with pneumonia. The results will then be used to outline the factors that indicate a high probability of pneumonia. This information would allow physicians to make more confident diagnoses of pneumonia and therefore reduce the number of chest radiographs.
Methods
Type of studyAfter institutional review board approval from Connecticut Children’s Medical Center, we conducted a retrospective chart review of patients who presented with symptoms suspicious for pneumonia to an urban Pediatric Emergency Department (PED) with approximately 57,000 visits a year.
Study population
The study population included children from birth to 18 years of age who presented with symptoms suspicious for pneumonia between January 1st, 2010 and December 31st, 2011. Data was analyzed for patients aged 2 years and older. Although the CAP guidelines are applicable to children aged 3 months and older, the primary analyses were done with children 2 years and older to prevent confusion with viral illnesses such as bronchiolitis. Study subjects were randomly selected from all patients presenting during this year based on chief complaint. Symptoms suggestive of pneumonia included chief complaints of fever, respiratory/difficulty breathing, and cough. Children were excluded if they had chronic lung diseases (i.e. asthma, broncho pulmonary dysplasia, sickle cell disease, any lung disease necessitating a tracheostomy), and non-infectious etiologies (i.e. costochondritis, trauma). Demographic information was collected including: age, race, sex, and insurance status (categorized as self-pay, public, or private).
Study design
The study subjects were divided into two groups: 1) patients with an ICD-9 discharge diagnosis of pneumonia as determined by the pediatric emergency medicine attending, and 2) a control group of patients with symptoms similar to those of pneumonia without a discharge diagnosis of pneumonia. The control group was utilized to compare differences in signs and symptoms between children diagnosed with pneumonia and children who were not diagnosed with pneumonia. Variables analyzed included: tachypnea (respiratory rate > 95% for age), fever (temp>38.0C), duration of fever (days), history of cough, any retractions, oxygen saturations, and physician documented abnormal breath sounds (rales, rhonchi, or wheezes). A sub-analysis was performed for patients greater than or equal to 5 years of age. Variables included in the sub-analysis are all variables listed above, with the addition of chest pain. History of cough, documentation of respiratory retractions, and abnormal breath sounds were extracted from the treating physician’s notes. If there was a discrepancy in documentation, the attending physician notes were used instead of the trainee notes. Demographics, clinical parameters, and results of chest radiographs were collected for both groups. Chest radiography (CXR) obtained in the study population was interpreted by a board certified pediatric radiologist. All data were obtained from the emergency department electronic medical record.
Analysis
Chi-square analysis was performed for each variable and a logistic regression model was used to identify significant independent predictors of a pneumonia diagnosis.
Results
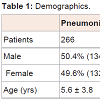
Of the 1600 charts (800 in each group) randomly identified for this study, 497 study subjects met the inclusion criteria. 51% (252) of the study subjects were female and31% (153) were Caucasian (Table 1). The mean age of the study subjects was 5.8 years (Table 1). 266 patients with the diagnosis of pneumonia were compared to the control group of 231 patients without the diagnosis of pneumonia. Asthma accounted for approximately 90% of exclusions in both groups. The other exclusions were broncho pulmonary dysplasia, sickle cell disease, and tracheostomy dependence.Of the 266 diagnosed with pneumonia, 91% (242) had a CXR. In comparison, only 13% (27/231) of patients in the control group without the diagnosis of pneumonia had a CXR. 80% (193) of the CXRs in the group diagnosed with pneumonia were interpreted as positive by a board certified pediatric radiologist (Figure 1). 7% (17) of the CXRs in the group diagnosed with pneumonia were interpreted as negative by a board certified pediatric radiologist (Figure 1).
The following were significant independent predictors of physician diagnosed pneumonia controlled for whether or not a CXR was performed: abnormal breath sounds OR 12.4 (95% CI: 5.7-26.9), cough OR 3.1 (95% CI: 1.5 - 6.3), and duration of fever >2 days OR 2.9 (95% CI: 2.1-4.1) (Table 2). Tachypnea, fever at triage, retractions, and oxygen saturations below 95% were not associated with the diagnosis of pneumonia.
A sub-analysis of patients 5 years of age and older was also performed. The following were significant independent predictors of physician diagnosed pneumonia controlled for whether or not a CXR was performed: rales OR 27.4 (95% CI: 4.8, 93.0) history of chest pain OR 29.5 (95% CI: 6.8-127.2), abnormal breath sounds OR 15.9 (95% CI: 4.7-53.9), cough OR 4.31 (95% CI: 1.3-14.2), and duration of fever >2 days OR 3.5 (95% CI: 2.0-6.0) (Table 3). Tachypnea, retractions, and oxygen saturations below 95% were not associated with the diagnosis of pneumonia.
The independent predictors of pneumonia were similar between children 2 years to 18 years and those from birth to 2 years. Rales OR 13.7 (95% CI: 5.6, 33.7), any abnormal breath sounds OR 7.6 (95% CI: 4.5, 13.0), cough OR 3.5 (95%CI: 2.0, 6.2) and duration of fever greater than 2 days OR 2.3 (95% CI: 1.9, 2.9) were significant. In addition, tachypnea (respiratory rate greater than 95% for age) was also found as an independent predictor with OR 1.6 (95% CI: 1.03,2.35).
Discussion
Community-acquired pneumonia is a common condition that presents to pediatric emergency departments. As a result, prompt diagnosis is important to determine proper treatment. The use of CXRs to aid in the diagnosis of pneumonia varies among pediatric emergency physicians. Our results show that CXR was routinely used in our pediatric emergency department to aid in the diagnosis of pneumonia. Furthermore, patients were diagnosed and treated for pneumonia even though CXRs were interpreted by a pediatric radiologist as normal or inconclusive 20% of the time. Similar observations have been made by previous studies [7,9].Recent guidelines recommend clinical assessment for the diagnosis of CAP and state that routine chest radiographs are not necessary for the confirmation of suspected CAP in patients well enough to be treated in the outpatient setting [6]. As a result it is important to identify physical exam and historical patient factors associated with the diagnosis of CAP in children. Our results show that any abnormal breath sounds, rales, cough, and duration of fever (>2 days) were significant independent predictors of pneumonia in patients with ages older than 2 years. Similar observations were made by Neuman et al. in 2011 [5]. In contrast to the results publish by Neuman et al., oxygen saturations below 95% were not a significant independent predictor for pneumonia in our study. Emergency physicians may find that combining their diagnostic acumen with these specific risk factors may increase their confidence in diagnosing pneumonia, thus decreasing the use of CXR for children with straightforward presentations.
Since history of chest pain is a difficult symptom to obtain in patients younger than 5 years of age, we conducted a sub-analysis of patients 5 years and older with the addition of chest pain to the list of variables analyzed. In this analysis, we found that history of chest pain, cough, duration of fever (>2 days) and any abnormal breath sounds were significant independent predictors of pneumonia.
The CAP guidelines were written to include children age 3 months and older [6]. Young infants may have viral etiologies or bronchiolitis and it is difficult to distinguish the etiology of pneumonia in patients younger than 2 years. We did not find any significant differences in predictors among our youngest patients, those from birth to 2 years. Significant independent predictors of pneumonia (duration of fever, history of cough, any abnormal breath sounds, rales) did not change upon inclusion of younger patients. The additional variable tachypnea was found to also be a significant predictor of pneumonia. Respiratory rate is variable and is sometime difficult to determine in young infants. Crying and fever can augment respiratory rate making this predictor challenging to interpret in clinical practice.
Developing a clinical practice guideline that incorporates the significant independent predictors of pneumonia would be advantageous. More importantly, it would reduce the over use of CXR for the diagnosis of pneumonia. This may result in decreased length of stay in the emergency department, reduce expenditure for radiographs and limit a child’s exposure to radiation.There are limitations to our study. First, the retrospective nature of the study design limits the information available to be analyzed. Incomplete or inaccurate transcription of medical records can cause some variability in the results. Additionally, we did not include patients with chronic respiratory conditions (i.e. asthma). Excluding this subset of patients allows us to more accurately correlate presenting symptoms with a discharge diagnosis of pneumonia. In doing so, however, we limit the applicability of the results to a heterogeneous patient population, as would be found in a typical emergency- department setting. Moreover, this study was conducted at a single tertiary pediatric emergency department and as a result, our results may not be applicable to other practice settings.
Finally, this study does not aid in identifying the root cause of community-acquired pneumonia (viral, bacterial, fungal, etc.). An ideal diagnostic solution would incorporate such factors, as the treatment plans for viral and bacterial pneumonia are different. Further investigation into the difference in symptoms caused by viral pneumonia and bacterial pneumonia, for example, would be useful in a future study and could be incorporated into a clinical practice guideline.
Conclusion
CXRs continue to be used routinely for the diagnosis of pneumonia in children. Clinical predictors of pneumonia included abnormal breath sounds, cough, and fever > 2 days. For children 5 years to 18 years, chest pain was also an independent predictor or pneumonia. For children from birth to 2 years, tachypnea was also an independent predictor of pneumonia. Future research is planned to develop a decision rule that identifies the need for CXRs when clinical assessment is unclear.References
- Dekate PS, Mathew JL, Jayashree M, Singhi SC (2011) Acute community acquired pneumonia in emergency room. Indian J Pediatr 78: 1127-1135.
- Lynch T, Bialy L, Kellner JD, Osmond MH, Klassen TP, et al. (2010) A systematic review on the diagnosis of pediatric bacterial pneumonia: when gold is bronze. PLoS One 5: e11989.
- McIntosh K (2002) Community-acquired pneumonia in children. N Engl J Med 346: 429-437.
- Mathews B, Shah S, Robert HC, Edward YL, Richard GB, et al. (2009) Clinical predictors of pneumonia among children with wheezing. Pediatrics 124: e29-e36.
- Neuman MI, Monuteaux MC, Scully KJ, Bachur RG (2011) Prediction of pneumonia in a pediatric emergency department. Pediatrics 128: 246-253.
- Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, et al. (2011) The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis 53: e25-76.
- Hagaman JT, Rouan GW, Shipley RT, Panos RJ (2009) Admission chest radiograph lacks sensitivity in the diagnosis of community-acquired pneumonia. Am J Med Sci 337: 236-240.
- O'Brien WT Sr, Rohweder DA, Lattin GE Jr, Thornton JA, Dutton JP, et al. (2006) Clinical indicators of radiographic findings in patients with suspected community-acquired pneumonia: who needs a chest x-ray? J Am Coll Radiol 3: 703-706.
- Wilkins TR, Wilkins RL (2005) Clinical and radiographic evidence of pneumonia. Radiol Technol 77: 106-110.
- Ron E (2002) Let's not relive the past: a review of cancer risk after diagnostic or therapeutic irradiation. Pediatr Radiol 32: 739-744.