International Journal of Otorhinolaryngology
Download PDF
Research Article
The Rate and Outcome of Sinonasal Disease in Children with Primary Immunodeficiency; Tertiary Hospital Experience
Almalki M1*, Alsaab F2, Fayhan Alroqi3, Shaheen N4 and Alhumaid S1
1Resident Otolaryngology-Head and Neck Surgery Department King
Abdulaziz Medical City
2Deputy Chairman of Pediatric Surgery Department Consultant Pediatric Otolaryngology, Davison of Otolaryngology-Head and Neck Surgery. King Abdulaziz Medical City (KAMC)
3King Abdullah International Medical Research Center (KAIMRC), King Saud Bin Abdulaziz University for Health Sciences, Ministry of National Guard Health Affairs (MNGH), Riyadh, Saudi Arabia
4Department of Biostatistics and Bioinformatics, King Abdullah International Medical Research Center (KAIMRC)
2Deputy Chairman of Pediatric Surgery Department Consultant Pediatric Otolaryngology, Davison of Otolaryngology-Head and Neck Surgery. King Abdulaziz Medical City (KAMC)
3King Abdullah International Medical Research Center (KAIMRC), King Saud Bin Abdulaziz University for Health Sciences, Ministry of National Guard Health Affairs (MNGH), Riyadh, Saudi Arabia
4Department of Biostatistics and Bioinformatics, King Abdullah International Medical Research Center (KAIMRC)
*Address for Correspondence: Almalki M, Resident Otolaryngology, Head and Neck surgery, Department, King Abdulaziz Medical City, Saudi Arabia E-mail: almalkiamalak@gmail.com
Submission: 13 October, 2023
Accepted: 14 November, 2023
Published: 20 November, 2023
Copyright: © 2023 Almalki M, et al. This is an open-access
article distributed under the Creative Commons Attribution
License, which permits unrestricted use, distribution, and
reproduction in any medium provided the original work is
properly cited.
Abstract
Objectives: To determine the rate, characteristics and outcome
of sinonasal disease (SD) among primary immune compromised (PID)
pediatric patients.
Methods: Cross-sectional retrospective study. All pediatric patients with primary immunodeficiency aged 18 years or less of both genders, had otorhinolaryngology (ORL) encounter or sinus CT at King Abdulaziz Medical City, Ministry of National Guard Health Affairs (MNGHA), Riyadh between January 2015 and December 2020 were included.
Results: 123 pediatric patients diagnosed with PID between 2015 and 2020. 9 patients were diagnosed with sinonasal disease. Chronic rhinosinusitis with nasal polyposis is the most common type of SD (66.66%). No significant association was found between having SD and bone marrow transplantation (P=0.424). Sinus CT Lund Mackay score was significantly higher in SD (p = 0.005). Endoscopic sinus surgery was carried in 44.44% of patients. 90% were alive and stable by the end of the study.
Conclusion: In conclusion, sinonasal disease constitute major risk of morbidity as well as for mortality in immunocompromised patients. Thus, early detection with high threshold of suspicion should be considered in this critical population.
Methods: Cross-sectional retrospective study. All pediatric patients with primary immunodeficiency aged 18 years or less of both genders, had otorhinolaryngology (ORL) encounter or sinus CT at King Abdulaziz Medical City, Ministry of National Guard Health Affairs (MNGHA), Riyadh between January 2015 and December 2020 were included.
Results: 123 pediatric patients diagnosed with PID between 2015 and 2020. 9 patients were diagnosed with sinonasal disease. Chronic rhinosinusitis with nasal polyposis is the most common type of SD (66.66%). No significant association was found between having SD and bone marrow transplantation (P=0.424). Sinus CT Lund Mackay score was significantly higher in SD (p = 0.005). Endoscopic sinus surgery was carried in 44.44% of patients. 90% were alive and stable by the end of the study.
Conclusion: In conclusion, sinonasal disease constitute major risk of morbidity as well as for mortality in immunocompromised patients. Thus, early detection with high threshold of suspicion should be considered in this critical population.
Introduction
The diagnosis and management of sinonasal disease in immune
competent patients is usually straightforward [1].However, in
immune compromised patients, the management can be very
challenging because of vague symptoms, paucity of the immune
response, and frequent association with aggressive and rapidly
progressive infection [2]. In addition, due to the advances in medical
field, the number of immune compromised patients is increasing
leading to more opportunistic infections by unusual pathogen such
as Pseudomonas aeruginosa and fungal agents [3,4].
Fungal sinusitis is classified into non-invasive and invasive
sinusitis based on the presence of fungal invasion into the submucosa
and adjacent structure [5]. The invasive fungal sinusitis is additionally
subclassified into chronic and acute disease, both of which affect
patients with some degree of immunodeficiency [5].Chronic fungal
sinusitis usually presents with non-acute symptoms such as lowgrade
fever, facial pain, epistaxis, or nasal congestion over months
to years. In contrast, acute fungal sinusitis usually presents rapidly
within less than one month period. In addition to the typical sinusitis
symptoms, patients may present with visual changes and cranial
neuropathies which indicate progression of the disease [3]. However,
patients with severe neutropenia frequently present with unspecific
symptoms such as fever lasting for more than 48 hours in early stages
with other symptoms occurring in later stage leading ultimately to
poor prognosis [6].The lack of ability to mount an efficient immune
response is thought to be responsible for its relatively high 50% to
90% mortality rate [7].
Early diagnosis and immediate treatment are considered vital for
better survival rates [6].The gold standard for diagnosis of fungal
sinusitis is histopathologic examination of nasal biopsies [7]. Middle
turbinate biopsy at the time of nasal examination is recommended
as a safe and effective method for timely diagnosis. This procedure
can be performed either upon patient’s admission or in outpatient
clinic setting at the time of endoscopic nasal examination [7].
Additionally, cultures are used to identify the offender agents and
their antimicrobial susceptibility. Aspergillus and Mucorales are the
most commonly isolated pathogens in acute invasive fungal sinusitis
(AIFS) [3]. Recently, more rapid and sensitive detection methods,
such as in situ hybridization and polymerase chain reaction (PCR),
have been used to facilitate immediate diagnosis [4]. Findings on
imaging workup are usually not specific in the early stages of the
disease and might lead to underestimation of the disease extent.
However, they remain critical to assess invasive sinonasal disease and
for surgical planning.
Optimal management of sinonasal disease in immune
compromised patients requires a multidisciplinary approach [3].
Urgent aggressive surgical debridement with antifungal therapy is the
mainstay of treatment in AIFS. In adult population, the main surgical
treatment is endoscopic sinus surgery (ESS). Reported success rate
is up to 80% with acceptable safety profile. ESS is also used in the
pediatric population, but less frequently, and mostly used for chronic
rhinosinusitis that is refractory to medical treatment. Outcome is
generally satisfactory with success rates in otherwise healthy children
ranging from 82% to 100%, and an estimated complication rate of
1.4%. However, limited data are available regarding ESS in immune
compromised children [4].
The purpose of the study is to shed light on the incidence,
characteristics, and outcomes of sinonasal disease in pediatric
primary immunodeficiency patients and thus facilitate in developing
guidelines for evaluation and management in such patients. To
the best of the author's knowledge, there are no similar researches
addressing this matter in Saudi Arabia.
Materials and Methods
The study was a retrospective cross-sectional study, approved
by the local institutional review board (IRB) King Abdullah
International Medical Research Center. All pediatric patients with
primary immunodeficiency aged 18 years or less of both genders,
had Otorhinolaryngologist (ORL) encounter or sinus CT at King
Abdul-Aziz Medical City, Ministry of National Guard Health Affairs
(MNGHA), Riyadh between January 2015 and December 2020 were
included. Patients aged 19 years and above, diagnosed with secondary
immunodeficiency were excluded from the study. Demographic,
clinical and radiological data were collected in pre-specified form. All
data regarding the patient were collected from the patient's electronic
record.
The study is based on a structured data collection sheet. The data
were entered into excel sheet. The data collection sheet is composed
of 14 questions, and divided into 4 domains; patient demographics
(gender and age), clinical (presenting symptoms), evaluation (Imaging
and pathology), and management (management and outcome).
Statistical Analysis:
The demographic and clinical characteristics such as gender,
presenting symptoms, and imaging data were presented as frequency
and percentage. Age was reported as mean and standard deviation.
Rate of sinonasal disease was estimated by dividing the number of
patients who had the disease over the total number of patients. Rate
was reported along with the corresponding confidence interval.Fisher exact test was used to association between categorical
variables. Mann-Whitney test was also used to test for association
as the variable of interest was not normally distributed. Level of
significant was set at 0.05.The analysis was conducted by using SAS
version 9.4.
Results
1) Demographic and Clinical Characteristics of the Study Cohort:
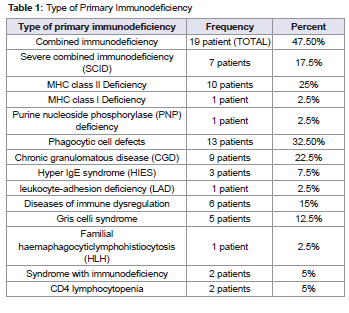
There are 123 pediatric patients who were diagnosed with
primary immunodeficiency between 2015 and 2020. 40 patients
were seen by ORL physicians during their admission or had sinus
CT. From these 40 patients, 19 patients (47.5 %) had combined
immunodeficiency, 10 patients had MHC class ll deficiency, 7
patients had severe combined immunodeficiency (SCID), 1 patient
had MHC class l deficiency, and 1 patient had Purine nucleoside
phosphorylase (PNP) deficiency. 13 patients (32.5%) had phagocytic
cell defects where 9 patients had chronic granulomatous disease
(CGD), 3 patients had HIES, and 1 patient had leukocyte-adhesion
deficiency (LAD). Also 6 patients (15%) had disease of immune
dysregulation in which 5 patients had Griscelli syndrome and one
patient had familial haemaphagocyticlymphohistiocytosis (HLH).
Lastly, only 2 patients had syndrome with immunodeficiency which
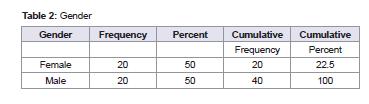
is CD4 lymphocytopenia [Table 1]. Regarding gender, 20 (50%) were
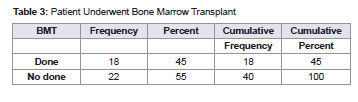
female patients and 20 (50%) were male patients [Table 2] . 18 patients
(45%) had bone marrow transplant. All patients had allogenic bone
marrow transplant [Table 3] .2) Demographic and Clinical Characteristics of Patients Developed Sinonasal Disease:
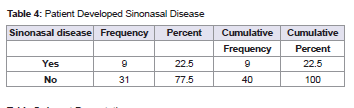
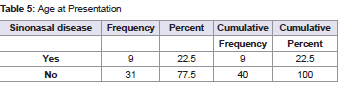
Out of these 40 patients included in the study, 9 patients
(22.5%) were diagnosed with sinonasal disease [Table 4]. Median
age for diagnosed patients was 7 years of age, with the youngest
patient aged less than 1 year and oldest was 13-year-old [Table 5].
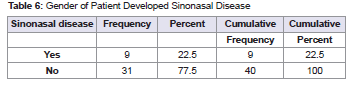
5 patients (55.56%) were male, and 4 patients (44.44%) were female,
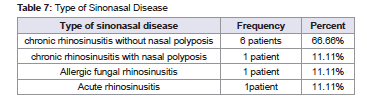
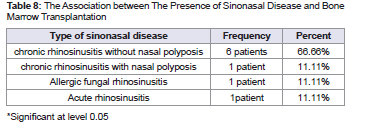
with no significant gender difference (P=1.00) [Table 6]. Chronic
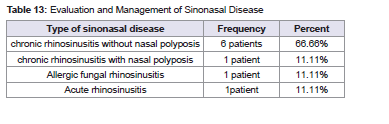
rhinosinusitis without nasal polyposis is the most common type
of sinonasal disease 6 patients (66.66%). Additionally, one patient
with chronic rhinosinusitis (11.11%) with nasal polyposis, one
patient with allergic fungal rhinosinusitis (11.11%) and lastly one
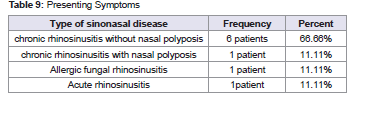
patient with acute rhinosinusitis (11.11%) [Table 8]. (P=0.424) Nasal obstruction was
the most common presenting symptom (33.3%), followed by fever,
facial pain, headache, and rhinorrhea (22.22%). Only one patient
(11.11%) had facial swelling. None of the patient had sign of ocular
involvement such asproptosisnoroculomotornervepalsy [Table 9].
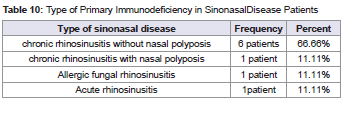
Regarding the underlying PID, 6 patients (66.66%) had combined
immunodeficiency, 2 patients (22.22%) had phagocytic cell defects,
and only one patient (11.11%) had Diseases of immune dysregulation
[Table 10].3) Sinus CT Scan Screening:
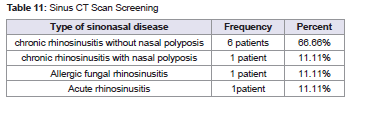
All of the diagnosed 9 patients with sinonasal disease had CT
scan. On the other hand, from the 31 unaffected patients, 27 patients
(87.10%) had screening sinus CT. For BMT, 17 patients out of 18
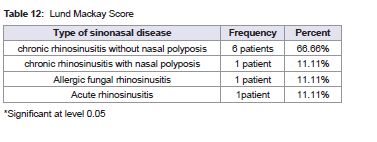
patients (99.44%) had screening sinus CT [Table 11] . A significant
difference in the mean of Lund Mackay score was observed between
those who had sinonasal disease and those who did not (p = 0.005).
It was observed that those with sinonasal disease had a significantly
higher Lund Mackay score compared to those without sinonasal
disease (16.89 + 4.78 vs 8.15 + 7.98) [Table 12].4) Evaluation and Management of Sinonasal Disease (N=9):
Further evaluation for diagnosed patients included nasal swab and
biopsy. 6 patients (66.67%) had nasal swab, while 5 patients (55.56%)
had nasal biopsy. 3 patients (33.33%) has positive results, 2 patients
were bacterial culture while only 1 patient had positive fungal culture.
Fungal Aspergillus was the detectable fungal pathogen. Endoscopic
sinus surgery was carried out in 4 patients (44.44%) of the total 9 with
sinonasal disease. None of the patients was given any antifungal agent
[Table 13] .5) Outcome of Patients Included in the Study (N=40):
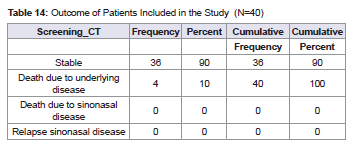
36 patients (90%) were alive and stable by the end of the study,
with no recurrent disease or relapse. However, 4 patients (10%)
passed away due to underlying disease with more advanced infections
that were not related to sinonasal disease [Table 14] .Discussion
This study offers insight into the occurrence, features, and outcomes
of sinonasal illness in children with primary immunodeficiency. To
the best of our knowledge, no analogous studies have been conducted
in Saudi Arabia. The study's findings demonstrate the guidelines for
evaluating and managing sinonasal illness in immune compromised
pediatric patients. This study comprised 40 individuals who had sinus
CT scans performed or been seen by ORL physicians.
Primary immunodeficiency disorders (PID) refer to a
heterogeneous group of disorders characterized by defect in one
or more components of the immune system [8]. Most of PID
result from inherited genetic defects; however some diseases are
not yet defined at the molecular level. In these cases, the disease is
considered primary only if all other potential contributors to immune
dysfunction such as viral or bacterial infections, malnutrition, or
immunosuppressive drugs have been excluded [8]. According to
American Academy of Allergy, Asthma, and Immunology, PID are
broadly classified into combined B- and T-cell immune deficiencies,
well-defined syndromes with immunodeficiency, predominantly
antibody deficiencies, diseases of immune dysregulation, congenital
defects of phagocyte, defects of innate immunity, auto inflammatory
disorders, and complement deficiencies [9]. In this study most of
the affected patients (66.66%) with sinonasal disease had combined
immunodeficiency.
There were 20 (50%) male patients and 20 (50%) female patients.
Only 18 individuals (45%) had a bone marrow transplant. However,
only 9 (22.5%) of the 40 patients were diagnosed with the sinonasal
illness. The diagnosed patient's median age was seven years, with
the youngest patient being less than 1 year-old and the oldest being
13 years of age. Similarly, a study conducted in 2017 by Amit Ritter
showed that immune suppressed pediatric patients with a mean age
of 9.5 year had acute rhinosinusitis [4]. Although a difference in the
prevalence of sinonasal disease was observed between those who
had a history of bone marrow transplantation and those who did
not (16.7% vs 27.3%), no significant association was found between
having sinonasal disease and bone marrow transplantation. (P=0.424)
According to our findings, nasal obstruction was the most
prevalent presenting symptom (33.3%), followed by fever, face pain,
and rhinorrhea (22.2 %). The least reported symptoms in this study
were nasal discharge and difficulty breathing [10]. Only one patient
(11.11 %) had facial swelling, which has previously been found to
be strongly indicative of acute invasive fungal rhinosinusitis (AIFR)
[4], yet none of the patient in this study developed AIFR. In contrast,
study in pediatric immune competent conducted by Alshehri et al.
in Saudi Arabia in 2021 found that fever was the most commonly
reported complaint (50%), followed by red eye (44%), runny nose
(42%), cough (41%), and headache (36 %).10 However most studies
in pediatric immune compromised patients showed that fever was
main presenting symptom. [4,11] On the other hand, 3 patients were
asymptomatic in this study suggesting that the absence of fever does
not rule out sinus infection.
While histopathology is the gold standard for diagnosing
sinonasal illness, paranasal sinus computed tomography (sinus CT)
is very useful and informative tool for diagnosis and effective surgical
planning. [12,13] However, in the early stages of the disease, it displays
nonspecific alterations such as unilateral enlargement of the nasal
cavity or paranasal sinuses. The nuclear magnetic resonance imaging
(MRI) is critical when the orbital or cranial invasion is suspected [14].
In our study, nine diagnosed patients received CT scans, whereas 27
patients (87.10 %) received screening sinus CTs. This suggest that
most immune compromised patients get full investigations including
sinus CT during hospital admissions to rule out invasive infections,
specially for patients who don’t have specific symptoms. The mean
Lund Mackay Score in our diagnosed patients was 16.88 compared to
8.15 of unaffected patients.
Culture investigations are also helpful in identifying the species
responsible for sinonasal illness.[4,15] However, the diagnostic
usefulness of these species is mainly restricted by their slow growth
rate, particularly for fungal infections.[4] Direct microscopy and
Histopathological results are faster alternatives, although species
identification is more challenging with these approaches.[16,17] Only
three patients (33.33 %), in our study got positive microbial infection
findings, i.e., two patients had a bacterial infection while only one
patient had a fungal infection. That is why mortality in this study
was related to underlying diseases rather than bacterial or fungal
infection, as in AIFR. Likewise, study in adult immune compromised
patients showed similar detection rate where (36%) of the patients
had positive culture results [6]. The detected fungal species in our
study was Aspergillus spp which is in accordance with previous
studies [18,19,20]. These microorganisms are saprophytes that may
be found in degraded materials, soil, and fruits, as well as in healthy
people's throats, nasal cavities, and feces. However, they can become
pathogenic in immune compromised patients [12,21]. Lastly, none of
the patients were given any antifungal agent.
Endoscopic debridement was performed based on clinical and
imaging results. 4 patients out of 9 (44.44 %) underwent endoscopic
sinus surgery, which was effective in terms of no recurrent disease or
relapse. 36 patients (90%) were alive and stable by the end of the study
while 4 patients (10%) passed away due to underlying disease rather
than sinus related infection. High survival rate explained by the fact
that none of the patient had AIFR compared to other study where
survival rate was only (49.7%) [20]. The degree of immunosuppression
and the state of the underlying illness have previously been linked to
the prognosis and mortality of AIFR. BMT is a risk factor for fatal
fungal infections [12,22,23]. where one study reported survival rate
was only 57% in 14 bone marrow transplant recipients, including
6 pediatric patients, affected with invasive sinonasal aspergillus.22
However, in the present study even though 17 out of 18 BMT patients
(99.44 %) had screening sinus CT; BMT was not risk factor to develop
sinonasal disease.
Conclusion
In conclusion, sinonasal disease constitutes a major risk of
morbidity as well as for mortality in immune compromised patients.
However, they may be under-diagnosed in pediatric immune
compromised patients as they tend to be asymptomatic and usually
present as either acute invasive ones or in late chronic subtype.
Thus, early detection with low threshold of suspicion should be
considered in this critical population. This could be achieved by
having a screening sinus CT in their early disease course. This will
help in early appropriate investigations such as cultures and biopsies
and further required surgical and medical management and finally a
better prognosis.
Author Contributions:
Malak Almalki was involved in the data collection, and in writing
the original draft of the manuscript. Fahad Alsaabwas involved
inmethodology, reviewing, and editing of the manuscript. Fayhan
Alroogiwas involved in reviewing the manuscript. Naila Shaheen
was involved in statistical analysis. Salwa AlHumaid was involved in
writing, reviewing, and editing of the manuscriptEthics Statement:
This study was approved by approved by the local institutional
review board (IRB)King Abdullah International Medical Research
Center.Data Availability:
The data that support the findings of this study are available from
the corresponding author, [Almalki MA] upon reasonable request.References
5. Montone KT (2016) Pathology of fungal rhino sinusitis: a review. Head and neck pathology 10: 40-46.