International Journal of Otorhinolaryngology
Download PDF
Mini Review
Mentoplasty for theTreatment of Chin Deformities
Sofia OB*, Dolci JEL, Mitre EI and Lazarini PR
- Department of Othorrinolaryngology of Santa Casa of São Paulo, Brazil
*Address for correspondence: Oscimar Sofia B, Faculty of Medical Sciences, Otorhinolaryngologist, Maxillofacial Skull Surgeon, Department of Otorhinolaryngology, Rua Duarte de Azevedo, 284 Cj 73, CEP: 02036-021, Santana - São Paulo - SP, Brazil, Fax: (11) 2950-5096/99975-7530, E-mail: droscimar@cirurgiaface.com.br
Citation: Ahmed S, Yousif OY, Abuzeid M. Tumours of Salivary Glands in Sudan. Inter J Otorhinolaryngology. 2018;5(1): 5.
International Journal ofOtorhinolaryngology | ISSN: 2380-0569 | Volume: 5, Issue: 1
Submission: 07 March, 2018| Accepted: 13 April, 2018 | Published: 18 April, 2018
Copyright: © 2018 Oscimar Sofia OB, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Mentoplasty is a surgical procedure that is indicated for the treatment of chin deformities, in the absence of dental malocclusion. In this article the authors describe in a concise way the patient’ s evaluation, surgical technique, complications and illustrate with clinical cases.
Genioplasty is a surgical procedure indicated for the treatment of chin deformities. In this article, the authors describe the patient evaluation, surgical technique, complications and clinical cases in a concise manner.
Keywords
Chin; Deformities chin; Surgery; Facial bones; Surgery
Introduction
The facial beauty depends on the shape, proportion, position and harmony between its various subunits. Mento occupies a prominent position in the lower third of the face, both in the frontal view and in the facial profile. Surgical access to deformities of the chin began in the second half of the last century, with the development of silicone prostheses. Mento osteotomies have allowed a new approach to deformities, altering chin height and position [1,2].
As in most facial plastic subjects, there are no papers showing evidence of the ideal management of chin deformities.
We used various techniques of augmentation. It is difficult to find isolated promentonism, usually we find prognathism that is associated with maxillo-mandibular deformities. In this text, we discuss the deformities of the chin, and its correction, for patients who have acceptable dental occlusion, but with a deficit in the contour of the chin, and patients with malocclusion corrected concomitantly with mentoplasty.
The techniques for augmentation are: Osteotomies (with or without autogenous graft placement) and alloplastic implants. Both have advantages and disadvantages. Implants are technically simpler, easily removable and with a low incidence of complications, while osteotomies are indicated for asymmetries and marked micro generations. Implants can be inserted by intra- (or) extra-oral access, while osteotomies require intraoral access. Intraoral incisions are contaminated, and present the risk of labial incompetence if the mental muscle is not approached correctly. The extraoral incision has the disadvantage of leaving a visible scar.
The alloplastic implant and the sliding osteotomies can be used together to obtain satisfactory results in selected cases [3].
Facial Analysis
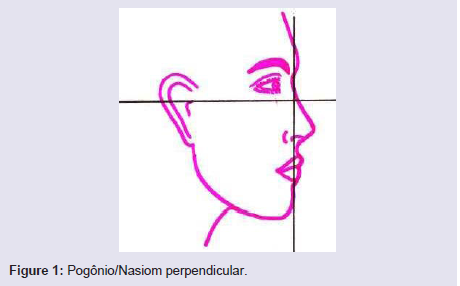
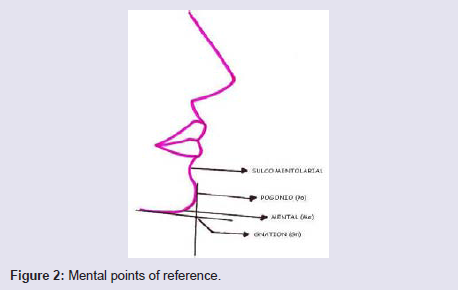
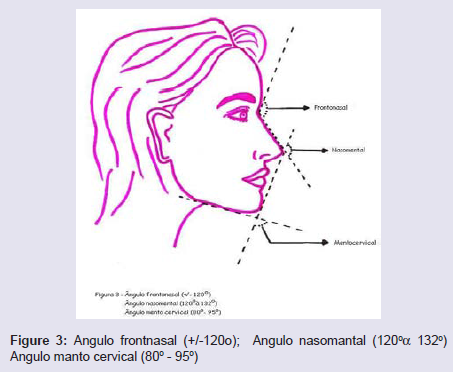
To determine the proper projection of the ment, we must use a method that is easy to execute, reproducible and that takes into account the aesthetic lines of the face. The simplest method to evaluate the projection of the chin is to draw a line perpendicular to the Frankfurt plane from the fronto-nasal suture (Figure 1). The chin should be in this line or slightly posterior. There are other methods of assessing chin projection, but they are more difficult to reproduce, calculate and use clinically. We always have in mind the important references of the mental region: chin-groove sulcus = depression below the lower lip, gnation = lowermost point of the contour of the mentum, pogonion = anterior point of the contour of the ment, mental = tion (Figure 2). Important angles of the mental region: Nasomental = 120 to 132 degrees, Mentocervical = 80 to 95 degrees, Nasal Frontal = about 120 degrees (Figure 3).
Figure 3: Angulo frontnasal (+/-120o); Angulo nasomantal (120°α 132°) Angulo manto cervical (80° - 95°)
We must always remember the thickness of the subcutaneous tissue and the musculature of the mental region that will directly interfere with our surgical planning.
Surgical Technique
Mentonian osteotomy
After the clinical and radiological evaluation, we planned theheight, the inclination and the extension of the osteotomy of thement.
In cases of hypomentalism, we calculated the previous slip to animaginary line perpendicular to the Frankfurt plane, from Nasion.The opposite is applied to macrogen or promentonism.
We make the intra oral incision anterior to the fund of gingivalsulcus from canine to canine. The subperiosteal detachment extendsto the region of the apices of the first premolars, where we mustfind the mental nerve that should be visualized and preserved. Theperiosteum is elevated lower and laterally. The suprahyoid musclesand the lingual periosteum should be kept inserted to maintain thevascularization of the osteotomized bone segment [4].
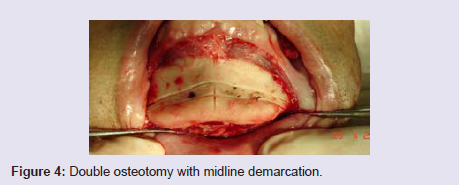
The osteotomy should be horizontal or inclined and asymmetrical,according to the planning, for this we use a reciprocating saw andperform a vertical mark in the midline for orientation at the time offixation. The osteotomy should be performed below the dental apices(Figure 4).
Bear in mind that sliding of the osteomized bone segment shouldbe done in the anteroposterior and / or lateral direction.
In order to increase vertical height, and horizontal slides greaterthan 10 mm from the limb, we used a bone graft inserted to theosteomized fragment (costal graft, cranial caliper, iliac) or performeda double osteotomy with a stepped slip (Figure 5). Autogenous graftsmay be bony, cartilaginous or osteocartilaginous.
The grafts have the disadvantage of requiring another surgicaltime for removal of the grafts, and resorption which may be partialor total due to local pressure and marked mobility of the adjacent softparts. Fat graft has total resorption.
The height of the lower third of the face, we do removing anintermediate fragment, that is, we make two osteotomies, keeping thelower fragment with its muscular insertions.
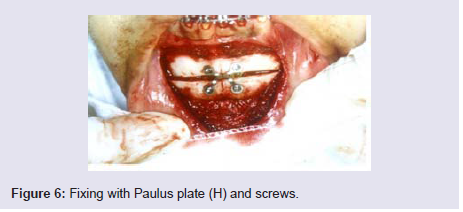
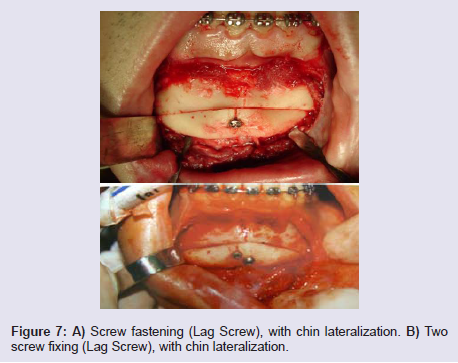
The fixation of the mobilized bone segment is made with steelwire number 1 or 2, in at least two points, or with miniplates andtitanium screws. We now use H-plate with 2 mm thick screws (Figure 6), or screws applied as Lag Screw (2 screws are advised to avoidfragment rotation) (Figure 7A and 7B).
Figure 7: A) Screw fastening (Lag Screw), with chin lateraliztion. B) Twoscrew fixing (Lag Screw), with chin lateralization.
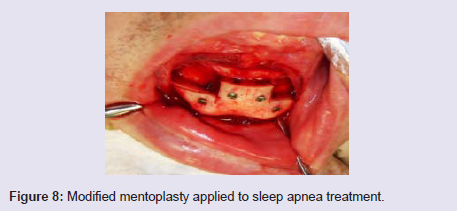
Mentoplasty may be a procedure applied to the treatment ofobstructive sleep apnea. In this case we make a technical modificationto draw a larger number of fibers of the genioglossus muscle (Figure 8).
The suture is made with absorbable wire (Catgut, Vicryl) numbers3-0 or 4-0, in two planes of preference, with special attention to therapprochement of the mental muscle.
Aloplastic Implants
Various materials can be used as a breast implant. The most widely used alloplastic implant in the world is solid silicone, both hard and soft. The most used material by us is porous polyethylene (Porex®), In our series has not yet occurred a major complication that would justify its removal. The same cannot be said of solid silicone, which has already been removed several times by displacements and bone erosions, including dental mobility of the region.
The great advantage of porous polyethylene is that it allows amore rigid fixation and, therefore, does not mobilize easily or causebone erosion [6].
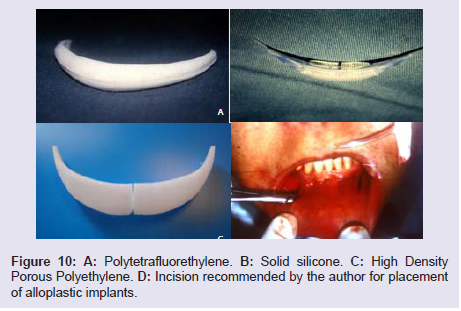
The authors recommend the technique of introducing a mentalprosthesis through a vertical incision of about one centimeter indiameter at the level of the canines, as the most feasible joiningthe two incisions, insertion of the recommended graft, suture anddressings (Figure 10A-10D).
Complications
Dental injury
The best way to avoid this complication is prevention.Cephalometry in conjunction with the panoramic jaw radiographprovides adequate insight into the position of the dental roots, whichshould be avoided during osteotomy and drilling for the placementof the screws or steel wire. If the dental apices are damaged, try topreserve them with endodontic treatment.
Infection
In the case of infection, culture material should be collected andempirical antibiotic therapy initiated promptly. In the case of implants,a sterile inflammatory process is expected around the implant, whichresolves in approximately 10 days. The inflammatory process lastingmore than 10 days should be considered infectious and treated as such.
Mentonian nerve injury
Meticulous dissection in the region of the foramen mentonianousually prevents nerve damage. Some paresthesia is expectedpostoperatively with spontaneous resolution. Paresthesia lastingmore than 6 months should be considered permanent. The use ofcorticosteroids in this situation is controversial [7,8].
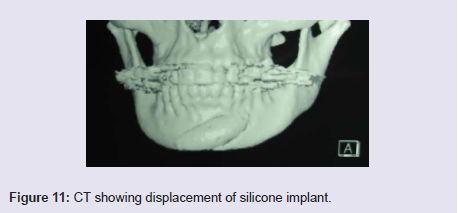
Displacement of the implant
Fastening with screws or steel wire prevents movement (Figure 11).
Bone Absorption
All alloplastic implants cause bone resorption, with potential to injure the dental roots, in addition to diminishing the projection of the ment.
References
- Hinds EC, Kent JN (1969) Genioplasty: the versatility of horizontal osteotomy. J Oral Surg 27: 690-700.
- Ward J, Podda S, Garri JI, Wolfe SA, Thaller SR (2007) Chin deformities. J Craniofac Surg 18: 887-894.
- Strauss RA, Abubaker AO (2000) Genioplasty: a case for advancement osteotomy. J Oral Maxillofac Surg 58: 783-787.
- Hu KS, Yun HS, Hur MS, Kwon HJ, Abe S, et al. (2007) Branching patterns and intraosseous course of the mental nerve. J Oral Maxillofac Surg 65: 2288-2294.
- Abramowicz S, Dolwick MF (2008) Intraoperative prediction of soft tissue positioning for advancement genioplasty using an anteriorly placed screw. J Oral Maxillofac Surg 66: 2166-2167.
- Gibbons AJ, Kittur MA, Sugar AW (2002) Stabilisation of genioplasty during rigid fixation: use of a holding screw. Br J Oral Maxillofac Surg 40: 346-347.
- Gui L, Huang L, Zhang Z (2008) Genioplasty and chin augmentation with Medpore implants: a report of 650 cases. Aesthetic Plast Surg 32: 220-226.
- Ward JL, Garri JI, Wolfe SA (2007) The osseous genioplasty. Clin Plast Surg 34: 485-500.