International Journal of Otorhinolaryngology
Download PDF
Postoperatively, betamethasone, epinephrine and saline drops are used four times daily and suction toilet is performed 2 hourly. Serial examinations under anaesthesia and endoscopic nasal washouts were performed at 2 weeks, and subsequently at 4 and 8 weeks if required.
The ideal procedure for choanal atresia should be quick and safe, restoring a normal nasal passage and avoiding any damage to surrounding structures [1]. Despite stenting, the restenosis rate remains high at 9-36% [5]. Stents have many disadvantages; discomfort, unsightliness, difficulty breast feeding and damage to the alar, septum or columella [6]. There have been several stentless repairs reported in the literature, but all associated with certain complications; temporary re-stenoses and palatal perforations.
Letter to the Editor
*Address for Correspondence: Hiro Ishii, United Kingdom International Journal of Otorhinolaryngology, UK, Tel: 07584070569; E-mail: hiro.ishii.85@gmail.com
Citation: Ishii H, Sproson E, Salib R, Andrea Burgess and Hasnaa Ismail-Koch. Choanal Atresia Repair without the Need for Stenting or Drilling: A Technical Modification. Inter J Otorhinolaryngology. 2016; 3(1): 2.
Copyright © 2015 Ishii H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Otorhinolaryngology| ISSN: 2380-0569 | Volume: 3, Issue: 1
Submission: 08 September, 2016 | Accepted: 28 September, 2016 | Published: 06 October, 2016
Choanal Atresia Repair without the Need for Stenting or Drilling: A Technical Modification
Hiro Ishii*, Eleanor Sproson, Rami Salib, Andrea Burgess and Hasnaa Ismail-Koch
- United Kingdom International Journal of Otorhinolaryngology, UK
*Address for Correspondence: Hiro Ishii, United Kingdom International Journal of Otorhinolaryngology, UK, Tel: 07584070569; E-mail: hiro.ishii.85@gmail.com
Citation: Ishii H, Sproson E, Salib R, Andrea Burgess and Hasnaa Ismail-Koch. Choanal Atresia Repair without the Need for Stenting or Drilling: A Technical Modification. Inter J Otorhinolaryngology. 2016; 3(1): 2.
Copyright © 2015 Ishii H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Otorhinolaryngology| ISSN: 2380-0569 | Volume: 3, Issue: 1
Submission: 08 September, 2016 | Accepted: 28 September, 2016 | Published: 06 October, 2016
We would like to present our modified technique to repair choanal atresia without the need for drilling or postoperative stenting.
Traditional repairs utilise postoperative stents for a variable period [1,2]. Stent-less repairs have been mostly transnasal requiring the raising of mucosal flaps and lateral drilling leading to circumferential scarring [3,4].
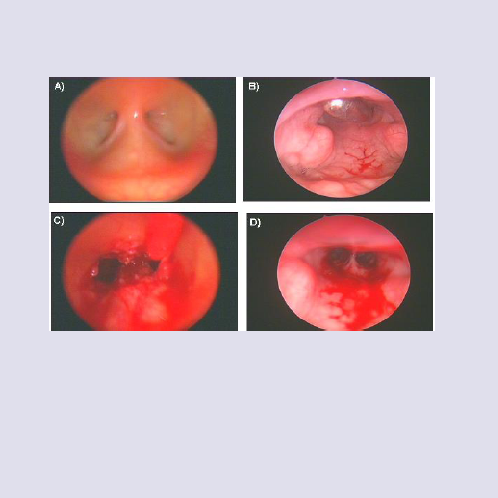
Our technique is performed under general anesthesia with oral intubation. The nose is decongested with 0.05% xylometazoline hydrochloride solution. Examination is performed with a 2.1 mmrigid endoscope. After insertion of an oral gag, a suture is used to retract the soft palate forwards. The atretic choanae are visualizedwith a 120° rigid endoscope transorally figure 1a. Urethral sounds (5F to 21F) are used to dilate the membranous portion of the choanae transnasally and can be seen transorally figure 1b. A small part of the posterior vomer is removed using paediatric back-biters figure 1c and redundant mucosa covers the exposed bone of the posterior septum.
Postoperatively, betamethasone, epinephrine and saline drops are used four times daily and suction toilet is performed 2 hourly. Serial examinations under anaesthesia and endoscopic nasal washouts were performed at 2 weeks, and subsequently at 4 and 8 weeks if required.
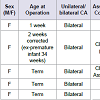
In total, we have performed this procedure on five patients Table 1. All patients were found to have bilateral choanal atresia and were female. Three of the patients were found to have isolated choanal atresia, one had an associated cleft lip and palate and one was found to have the CHARGE association. At the time of operation, three were operated at term, one at one week of age and one at 2 weeks of age corrected (for an ex-premature infant of 34 weeks’ gestation). The child with cleft lip and palate required two further dilatations; the child with CHARGE association had one further dilatation as did one of the isolated bilateral choanal atresia patients. The mean follow-up time is 24 months (median 3 years, range 4 months to 3 years). There are no complications documented in any of these patients.
The ideal procedure for choanal atresia should be quick and safe, restoring a normal nasal passage and avoiding any damage to surrounding structures [1]. Despite stenting, the restenosis rate remains high at 9-36% [5]. Stents have many disadvantages; discomfort, unsightliness, difficulty breast feeding and damage to the alar, septum or columella [6]. There have been several stentless repairs reported in the literature, but all associated with certain complications; temporary re-stenoses and palatal perforations.
Our method utilises the transnasal dilatation technique described by Morgan et al. and a transoral 120° endoscope [6]. In our technique, removal of a small part of the posterior vomer widens the neochoanae, thus negating the need for lateral drilling, associated with circumferential scarring. A formal mucoperiosteal flap can be very difficult to raise in a neonate and may be unnecessary, as redundant mucosa can be easily utilized to cover the exposed posterior septum.
In summary, this technical modification utilises traditional methods but crucially negates the need for both drilling and postoperative stenting. Thus far, it has proved successful in our hands and offers an alternative where space and access are limited. We are in the process of building a case series to validate its long-term efficacy.
References
- Yaniv E, Hadar T, Shvero J, Stern Y, Raveh E (2007) Endoscopic transnasal repair of choanal atresia. Int J Pediatr Otorhinolaryngol 71: 457-462.
- McLeod IK, Brooks DB, Mair EA (2003) Revision choanal atresia repair. Int J Pediatr Otorhinolaryngol 67: 517-524.
- Gujrathi CS, Daniel SJ, James AL, Forte V (2004) Management of bilateral choanal atresia in the neonate: an institutional review. Int J Pediatr Otorhinolaryngol 68: 399-407.
- Cumberworth VL, Djazaeri B, Mackay IS (1995) Endoscopic fenestration of choanal atresia. J Laryngol Otol 109: 31-35.
- Ibrahim AA, Magdy EA, Hassab MH (2010) Endoscopic choanoplasty without stenting for congenital choanal atresia repair. Int J Pediatr Otorhinolaryngol 74: 144-150.
- El-Ahl MA, El-Anwar MW (2012) Stentless endoscopic transnasal repair of bilateral choanal atresia starting with resection of vomer. Int J Pediatr Otorhinolaryngol 76: 1002-1006.