International Journal of Otorhinolaryngology
Download PDF
Research Article
*Address for Correspondence: Francesco Capuano, MD, Department of Otolaryngology, University Campus Bio-Medico, Via Alvaro del Portillo 21, 00128 Rome, Italy, Tel: +39 06 225411489; Fax: +39 06 22541520; E-mail: f.capuano@unicampus.it
Citation: Manuele C, Francesco C, Massimiliano V, Antonio M, Paol V, et al.. Bone Conduction after Stapes Surgery in Otosclerotic Patients with Mixed Hearing Loss: Fact or Fiction? Inter J Otorhinolaryngology. 2015;2(2): 4.
Copyright © 2015 Francesco et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Otorhinolarygology | ISSN: 2380-0569 | Volume: 2, Issue: 2
Submission: 31 August 2015 | Accepted: 26 October 2015 | Published: 30 October 2015
Comparing pre and post AC-PTA thresholds we have a statistically significant improvement [Pre-op: 59.1 dB ± 14.4; Postop: 33.8 dB ± 12.98 p< 0.05] ( Table 2).
Analyzing each AC frequencies we observed a statistically significant improvement in all frequencies, with higher improvement in low frequencies ( Figure 1).
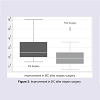
The evaluation of pre and post-op 5-PTA BC thresholds showed a statistically significant improvement [Pre-op: 29.1 dB ± 10.49); Postop: 22.1 dB ± 10.74; p< 0.05] ( Figure 2); this result was confirmed analyzing each frequencies; in particular we had an improvement for all frequencies, with a p < 0.05 from 250 to 2000 ( Figure 3).
In general 34 % (n.18) of our patients had an improvement in BC threshold after surgery ( Figure 4).
The Hearing Improvement ([pre-op air/bone conduction] - [post-op air/bone conduction]) for AC was 25.3 dB, while for BC was of 6.9 dB. No dead ears were encountered
Bone Conduction after Stapes Surgery in Otosclerotic Patients with Mixed Hearing Loss: Fact or Fiction?
Casale Manuele, Capuano Francesco*, Vitali Massimiliano, Moffa Antonio, Vella Paola, Ciglia Giacomo and Salvinelli Fabrizio
- Department of Otolaryngology, University Campus Bio-Medico, Rome, Italy
*Address for Correspondence: Francesco Capuano, MD, Department of Otolaryngology, University Campus Bio-Medico, Via Alvaro del Portillo 21, 00128 Rome, Italy, Tel: +39 06 225411489; Fax: +39 06 22541520; E-mail: f.capuano@unicampus.it
Citation: Manuele C, Francesco C, Massimiliano V, Antonio M, Paol V, et al.. Bone Conduction after Stapes Surgery in Otosclerotic Patients with Mixed Hearing Loss: Fact or Fiction? Inter J Otorhinolaryngology. 2015;2(2): 4.
Copyright © 2015 Francesco et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Otorhinolarygology | ISSN: 2380-0569 | Volume: 2, Issue: 2
Submission: 31 August 2015 | Accepted: 26 October 2015 | Published: 30 October 2015
Abstract
The aim of the study is to investigate the effect of stapes surgery on bone conduction (BC) in otosclerotic patients with mixed hearing loss.We retrospectively reviewed surgical database of 52 otosclerotic patients with mixed hearing loss.We retrospectively reviewed surgical database of 52 otosclerotic patients with mixed hearing loss. The guidelines of the American Academy of Otolaryngology-Head and Neck Surgery for the evaluation of results of treatment of conductive hearing loss were used.
Post-op 5-PTA BC thresholds showed a statistically significant improvement [Pre-op: 29.1 dB (10.5); Post-op: 22.1 dB (10.7); p< 0.05], confirmed by a mean gain of 6.9 dB in each BC frequencies. Our result suggests that selected otosclerotic patients with mixed hearing loss and small air-bone gap could be benefit from stapes surgery, restoring hearing and to stem BC impairment and otosclerotic progression.
Keywords
Otosclerosis; Hearing loss; StapedectomyIntroduction
Otosclerosis is a primary bone disorder affecting the labyrinthine otic capsule and the middle ear ossicles especially the uncusstapedial joint. It has a prevalence of 1-2% in the Caucasians; it is more common among the female sex and in more than 50% of patients it is hereditary. It clinically begins between 20 and 40 years of age and it is characterized by a slowly progressive hypoacusia, frequently associated with tinnitus and, more rarely, with vestibular symptoms. The otosclerosis course is quite irregular and quiescent phases alternate with disease progression periods; classically, earlier otosclerosis manifests itself more rapid and unfavorable.Patients with otosclerosis have three options: observation, to opt for hearing aids and surgery that achieves a long term best results.
As reported in literature, the indications [1] for stapes surgery for otosclerosis are:
- Unilateral or bilateral otosclerosis in which the average Air Bone Gap (AB gap) of four frequencies (500-1000-2000-4000 Hz) is 40 Db or more.
- Otosclerosis with severely declining bone conduction and AB gap < a 40 dB
- Very advanced otosclerosis
- Fixation of footplate in tympanoclerosis with an intact of repaired tympanic membrane
- Congenital anomalies with fixation of the footplate
The normal goal of stapes surgery for Ots is the closure of AB gap and in experienced hands the success rate for closure of ABG is up to 97% [2,3]. It could be considered an ABG after surgical procedure ≤ 10 dB as a successful stapes surgery.
Not rarely the progression of Ots affects inner ear leading to BC impairment. Some studies have valuated the BC trend after stapes surgery for otosclerosis.
Aarnisalo et al. showed a BC improvement after stapes surgery after 6 months follow up without statistically significance [4].Moscillo et al. showed a trend of BC improvement after surgery, statistically significant only in younger patients (< 45 years old) [5].
Quaranta [6], such us and Alireza Karimi Yazdi et al. noticed that only partial stapedectomy and not stapedectomy was associated with BC improvement at all frequencies [7].
Lippy performed stapedectomy in OTS patients with small ABG, obtaining excellent results with AB gap closure and BC improvement [1,2].
The aim of this retrospective study is to analyze and compare the effect of stapes surgery on bone conduction (BC) of adult otosclerotic patients
Materials and Methods
We retrospectively reviewed our surgical database, between January 2011 and January 2014, of 189 consecutive otosclerotic Caucasian adult patients referred to the ENT of Campus Bio-Medico, with hearing loss who underwent stapedectomy following the technique described and performed by House [8]. Patients older than 65 years old, with previous middle ear surgery and patients with pure conductive or sensorineural hearing loss, patients without an audiometric test at least 3 months after surgery were excluded from the study. All subjects had the same demographics (Caucasian), were operated by the same surgeon (FS), had the same prosthesis (floroplasticpiston prosthesis), under local anesthesia (2% lidocaine with epinephrine 1:100000) and sedation (midazolam 0.5 to 2 mg IV).According to our criteria we included 52 (M 12; F 40; age 50,02 range 32-64) patients with mixed hearing loss (HL) with a bone conduction > of 20 dB in at least three frequencies and an ABG ≥ 40 for at least four frequencies.
Each subject enrolled in our study underwent pre- and postoperative audiometric tests.
The mean time of audiometric testing after surgery was 6,4 months (range 3-14 months). The clinical follow-up period for each patient was of at least six months.
We compared pre and post stapes surgery Air conduction (AC) and BC thresholds using 7-Pure Tone Average (PTA) for the AC and 5-PTA for BC.
Moreover we compared the AC 7-PTA (125Hz-250Hz-500Hz-100Hz-2000Hz-4000Hz) and BC 7-PTA values for each frequencies (250Hz-500Hz-100Hz-2000Hz-4000Hz) pre and post-surgery.
Data are shown as mean and standard deviation or as median and interquartile range. Non-parametric (Wilcoxon test for paired data) test were used to compare different values. Our criterion for statistical significance was set at p values of less than 0.05 (2-tailed).
All statistical analyses were performed used STATA 9.
Comparing pre and post AC-PTA thresholds we have a statistically significant improvement [Pre-op: 59.1 dB ± 14.4; Postop: 33.8 dB ± 12.98 p< 0.05] ( Table 2).
Analyzing each AC frequencies we observed a statistically significant improvement in all frequencies, with higher improvement in low frequencies ( Figure 1).
The evaluation of pre and post-op 5-PTA BC thresholds showed a statistically significant improvement [Pre-op: 29.1 dB ± 10.49); Postop: 22.1 dB ± 10.74; p< 0.05] ( Figure 2); this result was confirmed analyzing each frequencies; in particular we had an improvement for all frequencies, with a p < 0.05 from 250 to 2000 ( Figure 3).
In general 34 % (n.18) of our patients had an improvement in BC threshold after surgery ( Figure 4).
The Hearing Improvement ([pre-op air/bone conduction] - [post-op air/bone conduction]) for AC was 25.3 dB, while for BC was of 6.9 dB. No dead ears were encountered
Discussion
In our institution the normal strategies are: observation when the patients is not bothered from hearing loss; hearing aids is preferred for patients with hearing impairment who do not want to undergo to a surgical operation; surgery is indicated for patients whit a great suspicious of otosclerosis (familiarity, female gender, age, audiometric tests, absence of reflex and typical timpanogram) with an Air Bone Gap (ABG) of at least 25 db for at least three frequencies is preferred. We do not perform CT for the diagnosis reserving this imaging technique for doubtful cases.Analysis of functional results shows that in our study our patients achieved considerable auditory gain after surgical operation. Because no cases of anacousia were found, we considered this sample particularly useful for analyzing postoperative BC auditory thresholds.
According to our results we noticed an improvement of BC threshold after stapes surgery. This is not a news.
Cahart was the first who noted an improvement in BC after stapes surgery, data confirmed by several authors [4-7].Many authors tried to explain this phenomenon.
According to Tonnodorf there are three components of BC hearing. These are distortional, inertial-ossicular and external canalosseotympanic components [9].
The first of these, distortional components, depends on vibration of the otic capsule caused by vibration.
The second depends on the movement of the ossicular chain.
The third one depends on external auditory canal.
In otosclerosis the main component affected is the second one, i.e. the ossicular inertia that is impaired because of the fixation on the uncus-stapedial joint. As Tonnodorf says, BC depends not only for direct transmission of the vibration to the inner ear fluids but it is also related to the relative movement of the footplate in the oval window due to the different inertia of the ossicular chain and the otic capsule [9].
Other authors made some hypothesis that could explain BC impairment in otosclerotic patients, first of all:
• Presence of toxic substances produces by the otospongiotic locus affecting the platina that can invade the cochlear fluid leading to a sensoneurinal loss [10].
• The elevated hypertension of the cochlear fluid due to stapes fixation [11,12] and due to the presence of a big otospongiotic focus over the oval window.
The removing of the greatest otospongiotic focus, typically all around the platina, could restore a good hearing in selected patients and to “put the leash” to the OTS and to BC impairment, reducing the fixation of the stapes and the production of toxic metabolites and the hypertension of the cochlear fluid, hypothesis is supported by studies of Vartianen and Karjalainen and confirmed by an electrophysiologic study of Lopponen and by clinical study of Lippy and Salvinelli [1,13-16].
Our data confirmed a BC improvement after stapedectomy as well showed in the House study that revealed a BC improvement, especially with stapedectomy technique with removal of the footplate greater than 25% [8]. We suggest performing stapes surgery also in selected otosclerotic patients with mixed hearing loss with small AB gap and/or small cochlear reserve, as also advised by other authors [1]. This indication to stapes surgery in these patients obviously requires a strong cooperation between patients and surgeon in order to reach the best results, preventing, in some cases, severe hearing impairment that compromise hearing aid benefit.
Conclusion
We know that these studies need additional research to explain the BC improvement after stapes surgery. Maybe a prospective trial could be helpful to reach this goal.References
- Sanna M, Sunose H, Mancini F, Russo A, Taibah A (2012) Middle ear and mastoid microsurgery (2nd edn), Thieme, New York, NY.
- Lippy WH, Burkey JM, Schuring AG, Rizer FM (1997) Stapedectomy in patients with small air-bone gap. Laryngoscope 107: 919-922.
- Rizer FM, Lippy WH (1993) Evolution of techniques of stapedectomy from the total stapedectomy to the small fenestra stapedectomy. Otolaryngol Clin North Am 26: 443-451.
- Aarnisalo AA, Vasama JP, Hopsu E, Ramsay H (2003) Long-term hearing results after stapes surgery: a 20-year follow-up. Otol Neurotol 24: 567-571.
- Moscillo L, Imperiali M, Carra P, Catapano F, Motta G (2006) Bone conduction variation poststapedotomy. Am J Otolaryngol 27: 330-333.
- Quaranta N, Besozzi G, Fallacara RA, Quaranta A (2005) Air and bone conduction change after stapedotomy and partial stapedotomy for otosclerosis. Otolaryngol Head Neck Surg 133: 116-120.
- Karimi Yazdi A, Sazgar AA, Motiee M, Ashtiani MK (2009) Improvement of bone conduction after stapes surgery in otosclerosis patients with mixed hearing loss depending from surgical technique. Eur Arch Otorhinolaryngol 266: 1225-1228.
- House HP, Hansen MR, Al Dakhail AA, House JW (2002) Stapedectomy versus stapedotomy: comparison of results with long-term follow-up. Laryngoscope 112: 2046-2050.
- Tonndorf J (1994) Bone conduction hearing. In: Keidel WD, Neff WD, edn. Handbook of sensory physiology. Berlin: Springer (Grade B).
- Causse J, Chevance LG, Bretlau P, Jorgensen MB, Uriel J, et al. (1977) Enzymatic concept of otospongiosis and cochlear otospongiosis. Clin Otolaryngol Allied Sci 2: 23-32.
- Carhart R (1962) Atypical audiometric configurations associated with otosclerosis. Ann Otol Rhinol Laryngol 71: 744-758.
- Carhart R (1950) Clinical application of bone conduction audiometry. Arch Otolaryngol 51: 798-808.
- Vartianen E, Karjalainen S (1992) Bone conduction thresholds in patients with otosclerosis. Am J Otolaryngol 13: 234-236.
- Vartianen E, Vartianen J (1995) The effect of preoperative bone conduction threshold levels on the results of stapes surgery. Eur Arch Otorhinolaryngol 252: 459-461.
- Lopponen H, Laitakari K (2001) Carhart notch effect in otosclerosis ears measured by electric bone-conduction audiometry. Scand Audiol Suppl 160-162.
- Salvinelli F, Casale M, Peco VD, Greco F, Trivelli M (2003) Stapedoplasty in patients with small air-bone gap: why not? Med Hypotheses 60: 535-537.