Journal of Orthopedics & Rheumatology
Download PDF
Case Report
A Rare Case of Aspergillus Spondylodiscitis In B-Cell Acute Lymphoid Leukemia
Sachin SJ1*, Smruthy AM2, Goutham KJ2, Shalaka2, Anjali Matani1, Priyank Tripati2, Nishit1, Amey CP1 and Chintankumar HK3
1Consultant haematology & Stem cell transplant, HCG Cancer
Hospital, Bangalore, India
2Clinical Pharmacology, HCG Cancer Hospital, Bangalore, India
3Department of Infectious disease, HCG Cancer Hospital, Bangalore,
India
*Address for Correspondence:
Sachin SJ, Consultant haematology & Stem cell transplant, HCG Cancer
Hospital, Bangalore, India; Phone: +91-9741351357; E-mail: drsachin.
jadhav@hcgel.com
Submission: 11 November 2021;
Accepted: 15 December 2021;
Published: 20 December 2021
Copyright: © 2021 Sachin SJ, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Introduction: Spondylodiscitis is an infection of the disc space
and surrounding vertebrae. Mycobacterium tuberculosis and
bacterial infections are the most prevalent causes, but fungal
spondylodiscitis is comparatively uncommon. Mycotic infections
are most commonly caused by Candida and Aspergillus species.
Aspergillus is a saprophytic fungus that lives mostly in soil and plants.
The incidence of Aspergillus affecting the bone among all cases of
invasive aspergillosis is estimated to be 3%. They infiltrate the spine in
immunocompromised patients, such as those who have had an organ
transplant, are on chronic steroid medication, or are undergoing
chemotherapy.
Case Report: An adult malewith Type 2 Diabetes Mellitus,
Hypertension and alcoholic liver disease was diagnosed with B-Cell
Acute Lymphoblastic Leukemia with CALLA positive, FISH Negative. He
was started on chemotherapy with G-MALL 07/03 regimen. During BFM
76/79 Re-intensification phase II the patient complained severe lower
back pain. A CT guided biopsy from the area previously diagnosed
to have Discitis (T4-T5 disc bulge soft tissue) showed negative for
malignancy. In view of persistent backache, MRI of whole spine and
pelvis was done, which revealed L4-L5 disc inflammation of infectious
etiology. Surgery for L4-L5 stabilization and biopsy from the same
region analyzed with molecular PCR revealed Aspergillus spp. Patient
was initiated on Anti-fungal agents.
Conclusion: Invasive aspergillosis most commonly affects the
sinopulmonary tract, with the lung being the most common location
of infection, while Aspergillus osteomyelitis is rare. Contiguity,
hematogenous spread, and direct implantation are all factors that
affect bone tissues. The prevalence of Aspergillus disrupting the bone
is believed to be 3% of all cases of invasive aspergillosis, with rates
ranging from 1 in 10,000 to 1 in 250,000. Treatment outcomes are greatly
influenced by a variety of factors, including neurological illnesses,
underlying conditions, and early detection and management.
Introduction
Spondylodiscitis is an infection of the disc space and surrounding
vertebrae. Mycobacterium tuberculosis and bacterial infections are the
most prevalent causes, but fungal spondylodiscitis is comparatively
uncommon. Mycotic infections are most commonly caused by
Candida and Aspergillus species. Aspergillus is a saprophytic fungus that
lives mostly in soil and plants. The incidence of Aspergillus affecting
the bone among all cases of invasive aspergillosis is estimated to
be 3%.They infiltrate the spine in immunocompromised patients,
such as those who have had an organ transplant, are on chronic
steroid medication, or are undergoing chemotherapy [1]. Invasive
aspergillosis can migrate from the lungs to the brain, kidneys,
heart, and bones, with the spine being a main target. It is frequently
misdiagnosed at first presentation because to its potentially delayed
start and non-specific clinical symptoms [2]. Medical therapy alone
or surgery with medical therapy is the mainstay of treatment [3,4].
Here, we report the case of an immunocompromised 53-year-old
male with L4-L5 spondylodiscitis caused by Aspergillus.
Case
A 53 year old gentleman with Type 2 Diabetes Mellitus,
Hypertension and alcoholic liver disease was diagnosed with
B-Cell Acute Lymphoblastic Leukemia with CALLA positive, FISH
Negative. He was started on chemotherapy with G-MALL 07/03
regimen. During G-MALL 07/03 induction phase 1 he developed
vincristine induced pseudo-obstruction which was managed with
conservative treatment. During Induction with G-MALL 07/03
phase II, the patient had increased transaminase level, biopsy showed
features of alcohol induced liver dysfunction also he was found to
have secondary haemochromatosis with deposition of iron in liver
and heart managed with Deferoxamine in view of this the treatment
was changed to BFM 76/79 chemotherapy protocol with appropriate
hepatic dose modification. While on the chemotherapy, post PEG
asparaginase (BFM 76/79 Reintensification Phase1) he had an
episode of elevated liver enzymes. Later he developed transient loss of
vision further examination revealed occipital lobe abscess for which
he underwent surgical excision and was also treated with empirical
antibiotics and antifungal. The chemotherapy continued as per
schedule and he was post BFM 76/79 consolidation, BFM 76/79 Reintensification
phase I and II.
At the last cycle of BFM 76/79 Re-intensification phase II the
patient complained severe lower back pain. A CT guided biopsy
from the area previously diagnosed to have Discitis (T4-T5 disc bulge
soft tissue) showed negative for malignancy. In view of persistent
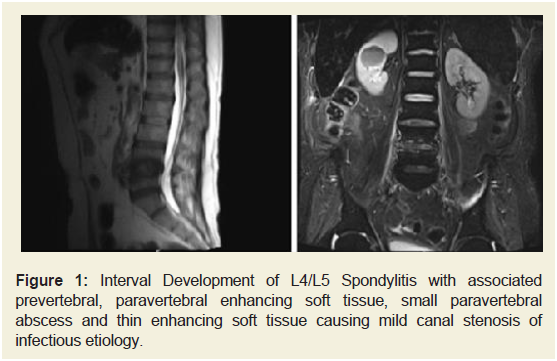
backache, MRI of whole spine and pelvis was done (Figure 1),
which revealed L4-L5 disc inflammation of infectious etiology. The
patient underwent posterior spinal decompression with wit L4-L5
debridement with instrumentation and stabilization. Intraoperative
findings showed unstable L4-L5 vertebra. Biopsy from the same region
analyzed with molecular PCR revealed Aspergillus spp. The patient
was initiated on empirical antifungal treatment with Liposomal
Amphotericin B with necessary premedication but after the third dose he developed hypersensitivity reaction and the treatment was
interrupted. His treatment was thus changed to Voriconazole, after
the first dose of which he developed an episode of hallucination.
Following this, Isavuconazole was prescribed for 6 months and he
tolerated it with significant symptomatic improvement. After 2 weeks
of isavuconazole therapy, during the next follow up visit voriconazole
was re-challenged and the patient tolerated it well which was done in
view of financial constraints. He is now on follow up with voriconazole
maintenance therapy.
Figure 1: Interval Development of L4/L5 Spondylitis with associated
prevertebral, paravertebral enhancing soft tissue, small paravertebral
abscess and thin enhancing soft tissue causing mild canal stenosis of
infectious etiology.
Due consent was taken from the patient before publication
procedures.
Discussion
Aspergillus species are saprophytic microbes that are ubiquitous.
Invasive aspergillosis most commonly affects the sinopulmonary
tract, with the lung being the most common location of infection,
while Aspergillusx osteomyelitis is rare. Contiguity, hematogenous
spread, and direct implantation are all factors that affect bone tissues.
The prevalence of Aspergillus disrupting the bone is believed to be
3% of all cases of invasive aspergillosis, with rates ranging from 1 in
10,000 to 1 in 250,000. Men are 3 times as likely as women to be
affected [5,6].
Although Aspergillus spondylodiscitis is an uncommon
opportunistic fungal infectious illness, it has recently overtaken
Candida spondylitis in terms of occurrence. It most commonly
arises in an immunocompromised host as a result of AIDS, organ
transplantation, chemotherapy, or immunosuppressive medication,
among other factors [2,7]. The patient in this case was
immunocompromised, and the predominant focus of Aspergillus
appeared to be pulmonary.
Aspergillus spondylodiscitis is characterised by a lack of
particular clinical characteristics. Lower back pain with or without
fever, neurologic impairments due to cord damage, or kyphosis are
the most prevalent symptoms. The majority of patients developed
spondylodiscitis or epidural abscess at one or more vertebral levels.
Diagnosing aspergillus spondylitis early is difficult and requires a high level of suspicion. Histopathological investigation and bacterial
culture are the most reliable diagnosis procedures for Aspergillus
spondylitis. Diagnostic imaging, such as CT and/or MRI, is necessary
for disease staging and guiding orthopaedic and/or neurosurgical
intervention [2,4,7]. In our case, the patient is known ALL, and
radiological findings suggested infective spondylodiscitis at L4-L5.
The diagnosis was confirmed by a surgical biopsy.
Surgical decompression in combination with antifungal therapy
is advised for Aspergillus spondylodiscitis patients who have spinal
instability or symptoms consistent with spinal cord or radicular
compression or abscess formation. The Infectious Diseases Society of
America (IDSA) recommends an antifungal treatment regimen of at
least 8 weeks, with longer courses (>6 months) frequently required.
Voriconazole has been recommended as a first-line treatment,
either alone or with surgical debridement. Amphotericin B or
Isavuconazole is an alternative primary treatment. Itraconazole has
been used subsequent to a course of Amphotericin B. Posaconazole
or echinocandins have been used in the treatment of Aspergillus
spondylodiscitis with limited results [4]. In the present case,
Aspergillus spondylodiscitis was treated with Isavuconazole as patient
could not tolerate Voriconazole and Amphotericin B. Isavuconazole
have numerous benefits over existing azoles, including comparable
effectiveness with fewer adverse effects, favorable pharmacokinetic
characteristics, and good absorption when administered orally
but affordability as maintenance therapy remains a disadvantage
to be addressed [8]. The patient tolerated and is symptomatically
better with the current medication. Treatment outcomes are greatly
influenced by a variety of factors, including neurological illnesses,
underlying conditions, and early detection and management.