Journal of Orthopedics & Rheumatology
Download PDF
Research Article
Early Failure of an Inlay Modular Shoulder Arthroplasty for Proximal Humeral Fracture in a Retrospective Series
Page R1,2, Brown G1,2, Richardson B1 and Eng K1,2*
1Department of Orthopedics, Deakin University, Australia
2Department of Orthopedics, Barwon Health University Hospital Geelong, Australia
*Address for Correspondence: Eng K, Orthopedics Department, Barwon Health University Hospital Geelong, Ryrie St, Geelong 3220, Australia; E-mail: kevineng@geelongortho.com.au
Submission: 26 April 2019;
Accepted: 30 May 2019;
Published: 07 June 2019
Copyright: © 2019 Page R, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 6, Issue: 1
Abstract
Background: Surgical reconstruction of proximal humeral fractures
is difficult, and failure may occur leading to revision surgery. The
development of convertible modular hemiarthroplasty has the potential
to reduce the complexity of revision surgery. The aim of this study was
to review the failure rate and modes of an inlay modular humeral
hemiarthroplasty prosthesis used for proximal humeral fractures.
Methods: A retrospective clinical review of the medical records
and X-rays was undertaken. A sawbone model was used to implant a
Global FX and a Global Unite convertible hemiarthroplasty to compare
differences in height and offset between the prostheses.
Results: Six patients (five females, one male) had a Global Unite
hemiarthroplasty with a mean age 73.66 years. Four (66%) failed
by superior migration at a mean of six months. In vitro sawbones
measurement identified the humeral height of the Global Unite was
approximately 3 mm higher than the Global FX (the previous model).
Conclusion: We experienced a 66% failure rate of the Global Unite
by superior migration. Our previous series of Global Fx had a failure rate
of 23%. We postulate that the extra height of the Global Unite increases
the excursion of the rotator cuff tendons, placing undue tension on the
rotator cuff and tuberosity construct predisposing to early failure. We
recommend that the consideration be given to downsizing the humeral
head and using a smaller body where possible.
Keywords
Hemiarthroplasty; Failure; Shoulder; Humerus; Global
Unite; Revision
Abbreviations
AOA NJRR: Australian Orthopaedic Association National Joint
Replacement Registry
Introduction
Proximal humeral fractures are common, with the majority
being treated non-operatively, achieving satisfactory results [1]
However, the optimal treatment of comminuted fractures in elderly
osteoporotic bone or unreconstructable high-energy fractures in
younger patients remains unclear with high complication rates
with attempted internal fixation [2]. Prostheses have been used to
treat these unreconstructable fractures [3]. However, this operation
remains technically difficult and results rely on tuberosity union and
restoration of rotator function. Modular prosthesis and then fracture
specific stems have been designed in an attempt to improve tuberosity
healing [4,5].
Despite these refinements, failure of the hemiarthroplasty may
occur leading to revision surgery. Superior migration is a common
mode of failure for cuff deficient shoulders, and is also seen in failed
hemiarthroplasties where the rotator cuff-tuberosity complex is
deficient. Superior migration is associated with large supraspinatus
tears, often with involvement of the infraspinatus [6]. Boileau reported that excessive humeral height more than 10mm was associated with
an increased rate of failure of the cuff tuberosity complex and poor
clinical result [7]. Version of the humeral prosthesis greater than 40
degrees and age over 75 years and female sex were also associated with
reduced clinical outcomes. Following rotator cuff or tuberosity failure,
conversion to a reverse shoulder arthroplasty can be considered to
accommodate tuberosity non-union and poor rotator cuff function
[8]. However revisions are associated with complications, including
but not limited to challenges with removal of a well-fixed stem [9].
The development of convertible components, which allow the
original humeral stem to be retained, may reduce complications in
relation to removal of the stem and operative time [9]. The Global
Unite is one of the convertible platform systems [10], with a collar
to aid tuberosity fixation and a modular “inlay” body that is fixed
inside the humeral shaft, allowing alteration of version and height
if desired. This is in contrast to other “onlay” convertible designs
in which the reverse body lies superior and outside the cut surface
[11]. Convertible constructs may have subtle differences in prosthetic
dimension such as head height or offset in comparison to traditional
designs. Technical adjustments may be required to avoid stress on
the rotator cuff.
We present our experience with Global Unite fracture after noting
a high early rate of failure via superior migration. We postulated was
that the modular convertible bodies may increase the humeral height
in comparison to the non-convertible hemiarthroplasty due the
component geometry, leading to early rotator cuff failure.
Materials and Methods
We undertook a retrospective review, and performed a sawbone
comparison of the height and offset of the Global FX and the
convertible, platform based Global Unite.
Case review:
Cases that utilized a Global Unite were identified from medical records. The records and X-rays were assessed for complications
retrospectively. The following parameters were assessed on X-ray.
Vertical tuberosity displacement was defined as abnormal if the
tuberosity united <10 mm below the summit of the head or more
than >5 mm above. Horizontal tuberosity displacement was defined
as no bone lateral to the prosthesis in the AP X-ray, and the tuberosity
seen in the lateral view behind the prosthesis [7]. This implies that
the tuberosity has displaced posteriorly due to the pull of the
infraspinatus. Proximal migration of the prosthesis was defined on
an AP X-ray as an acromiohumeral distance of <7 mm 7 or a >5 mm
migration of the center of the prosthetic head from the central axis of
the glenoid [12]. This implies that the entire posterosuperior rotator
cuff has failed and the humerus is migrating proximally.Sawbone model:
The aim was to compare the Global Unite and Global FX in the
same sawbone model to assess the differences in height and offset. A
left sided sawbone model was utilized.Defining the axis of offset:
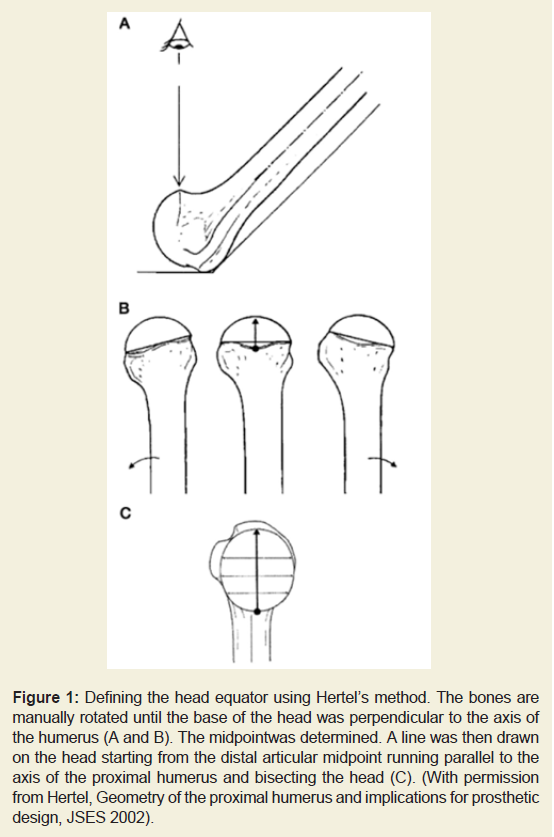
We identified the “distal articular midpoint” as defined by Hertel
[13]. Briefly, with the humerus raised at a 45 degree angle to the table,
the humerus was rotated until the base of the head was perpendicular to the axis of the shaft of the proximal humerus. The “distal articular
midpoint” was defined as the midpoint along this line. The head
equator was then drawn from the distal articular midpoint running
parallel to the axis of the proximal humerus and bisecting the head
[14]. This line was used to measure offset perpendicular to the axis
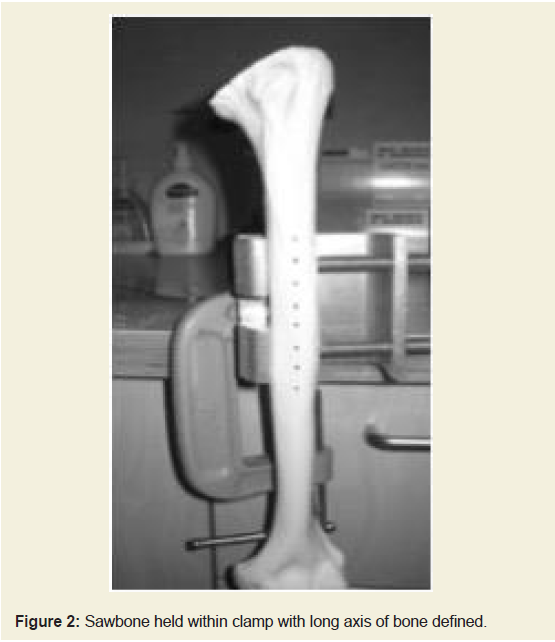
of the shaft.The sawbone was fixed into a vice with the two clamps buried into
the bone model to prevent movement (Figure 1and 2).
Figure 1: Defining the head equator using Hertel’s method. The bones are
manually rotated until the base of the head was perpendicular to the axis of
the humerus (A and B). The midpoint was determined. A line was then drawn
on the head starting from the distal articular midpoint running parallel to the
axis of the proximal humerus and bisecting the head (C). (With permission
from Hertel, Geometry of the proximal humerus and implications for prosthetic
design, JSES 2002).
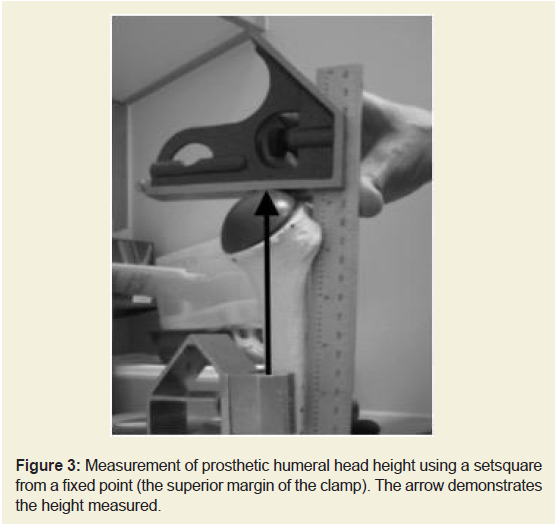
Marks were made using a set square along the shaft of the
humerus parallel to its longitudinal axis. This line was used to align a
setsquare to consistently measure height. Height was measured from
the proximal tip of the vice, which was a consistent fixed point to the
most superior margin of the humeral head (Figure 3)
Figure 3: Measurement of prosthetic humeral head height using a setsquare
from a fixed point (the superior margin of the clamp). The arrow demonstrates
the height measured.
An anatomic neck cut was made. The shaft was prepared for
size 10 Global FX stem. A 52 mm + 18 head was attached. Digital
calipers were used for measurements of offset and height along the
axis described above. The same bone and cuts were retained. A size
10 Global Unite with a 0 body, size 10 stem and a 52+18 head was
inserted. Measurements were made again
A 52 + 15 head was then measured as recommended by the DePuy
technical guide as the equivalent head size to adjust for the prosthetic
collar [10]. Smaller heads were then utilized to find the height that
was equal to the Global FX.
Results
Clinical series:
Six patients (five female, one male) with a mean age of 73.66 years
(range 63-82 years) had a Global Unite hemiarthroplasty between 2013-2015. The indications were four part fractures in four patients
and fracture dislocations in two. All operations were performed by
shoulder fellowship trained Orthopedic surgeons, with four done by
a extended deltoid splitting approach as described by Robinson [15],
and two by a standard deltopectoral approach. All surgeries were
performed acutely at a mean of 5.5 days post injury (range 1-15 days).
The post operative rehabilitation was 6w weeks in an immobiliser
sling doing passive range of motion with no external rotation beyond
0 degrees. Then active range of motion as the patient tolerated was
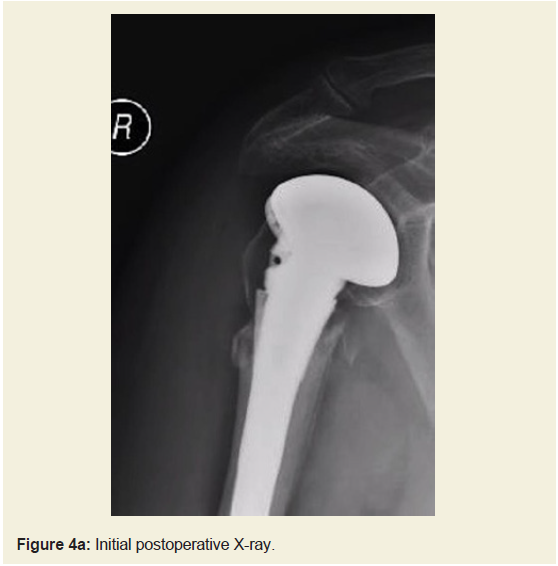
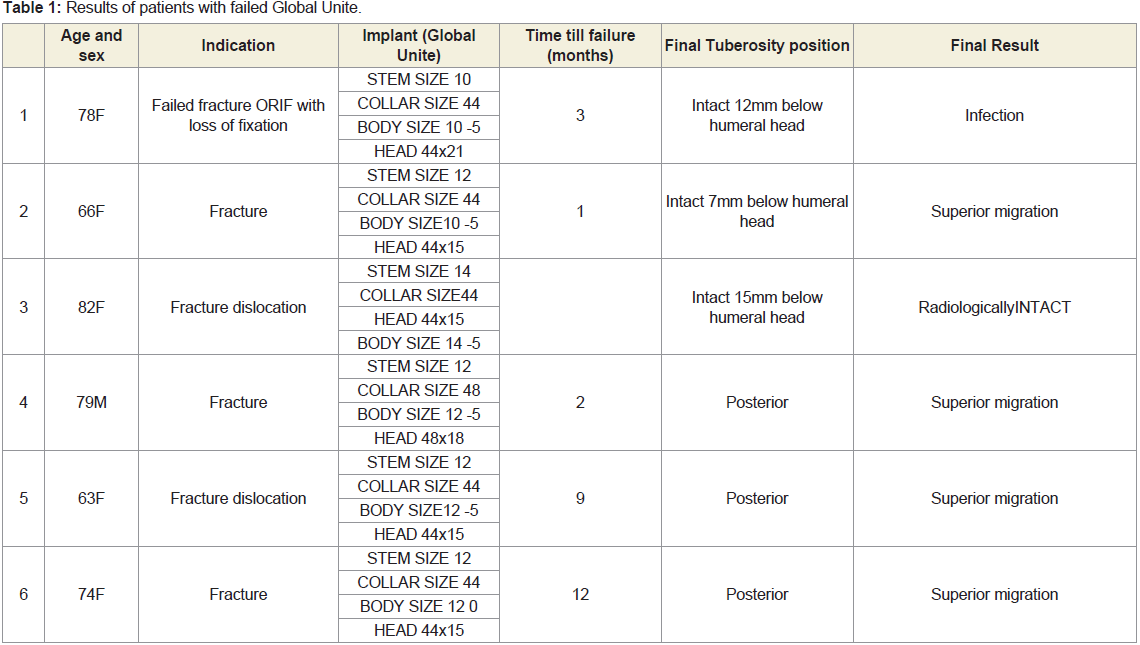
allowed from 6-12w, then strength work once range is recovered.The results of our patients are summarized in (Table 1). Four
(66%) failed by superior migration at a mean of 6 months (range
1-12 months) post operatively. Of these, two failed with tuberosities
united 7mm below humeral head (Figure 4a and 4b), and two with
non-united greater tuberosities. One had a deep infection. One was
adjudged to be intact radiographically, with united tuberosities and
no superior migration. All patients retained their original humeral
stem during revision surgery.
In contrast our previous series of monoblock Global Fx
hemiarthoplasties had a lower rate of radiological failure23%. 13
cases were reviewed from 2006. The mean follow up was 4.8yrs
(range 1.2 years - 14.9 years). 2 had superior migration, and 1 had a
radiologically loose stem.
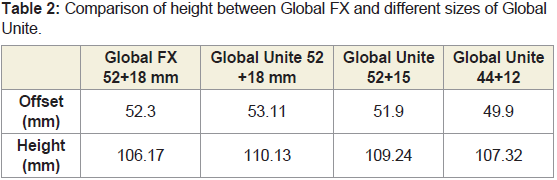
Sawbone measurements:
We noted that the height of the Global Unite was 3.96 mm
greater when the same size head (52+18) was used (Table 2). The
recommended adjustment of using a 3mm smaller head height
(52+15) reduced the height difference to 3.07 mm. Approximate
equivalence to the Global FX was achieved with a 44+12 head.Discussion
We found a 66% failure rate of the Global Unite proximal
humeral hemiarthroplasty in our series via a mechanism of superior
migration. The Global Unite head height is 3.96mm higher than the
Global FX, which we hypothesize may lead to over tensioning of the
rotator cuff resulting in a non-anatomical reconstruction, which
must be accounted for when using the modular implant.
We postulate that the extra head height of the Global Unite
increases the excursion of the supraspinatus and infraspinatus tendon when the tuberosity is fixed just below the collar. This may place
undue tension on the rotator cuff and tuberosity construct, leading
to early failure.
Functioning of the rotator cuff is critical to the clinical outcome.
Boileau noted that the excessive humeral height compromised the
functional outcome [7]. Other factors influencing outcome were
final tuberosity position, age over 75 years and being female[7,12].
Similarly, others have also since reported on the poor results in
those with mal-united or non-united tuberosities [16-18]. Other factors recently reported include a critical shoulder angle>38 deg and
increased medical comorbidities such as Parkinson's disease [19].
The decision on how to manage comminuted fractures in elderly
osteoporotic bone or unreconstructable high-energy fractures in
younger patients remains difficult, and the results of hemiarthroplasty
can be variable. In a randomized controlled trial over 2 years, Olerud
noted that a hemiarthroplasty did not improve the range of motion
or constant scores in comparison to non-operative measures,
however the hemiarthroplasty group had less pain [20]. They noted
a 20% loss of position of tuberosities. In contrast Boon reported in
their randomized controlled trial that the hemiarthroplasty and
non operative grouphad no difference in pain at 12 m. The non
operative group had better abduction strength. Again there was
also no difference in constant scores. Superior migration was seen
in 20% of the hemiarthroplasty group [21]. In a systematic review
in 2008 looking at 810 hemiarthroplasties a proximal migration
rate of 6.8% was found. They noted a marked functional limitation
as well [17]. The Australian Orthopaedic Association National Joint
Replacement Registry (AOA NJRR) reported a 10% revision rate
for hemiarthroplasty with rotator cuff insufficiency being the most
common revision indication [22].
To produce more reliable outcomes, fracture specific stems have
been designed to enhance tuberosity fixation and ultimately union,
and these stems may lead to improved tuberosity union and improved
constant scores [23-25].
Arthroplasty systems with convertible stems may reduce morbidity
in revision negating the requirement for humeral osteotomy and
wider dissection. Reduced blood loss, fewer perioperative fractures,
fewer nerve palsies and infections when the humeral stem could
be retained and converted has been reported. The role of reverse
arthroplasty in primary treatment of these fractures is evolving and
become more common [26].
One potential benefit of the Global Unite is that its modular
components remain inside the humeral cut and supported by bone,
the concept of an ‘in lay’ prosthesis. A lack of proximal humeral bone
stock surrounding the components may concentrate forces on the
join leading to uncoupling or instability. Catastrophic failure of a
modular stems have been reported [27,28] When the links between
the components were outside, and therefore unsupported by, cortical
bone. Good results have been reported in primary arthroplasty using
the Global Unite shoulder system with revision from anatomic to
reverse possible with exchange of the modular components and
retention of the humeral stem [29].
A smaller diameter and reduced head height head may reduce
the tension on both the infraspinatus and supraspinatus, and this
technique has been utilized by Japanese surgeons for hemiarthroplasty
[30]. We would recommend making adjustments. The smallest body should be used and a reduction of head height of 3mm and width
should be considered.
The Global Unite prosthesis has been flagged in the Australian
Orthopedic Association National Joint Replacement Registry (AOA
NJRR) as a prosthesis with a higher than expected revision rate
[22]. The cumulative percent revision rate for hemiarthroplasty for
fracture is 8% at seven years. For the Global Unite it is 24.7% (73
cases) at two years, with the most common reason for revision being
rotator cuff insufficiency (57.1%). This highlights not only a potential
problem with this as a hemiarthroplasty, but highlights the value of
nationwide, inclusive post market surveillance of new prostheses to
guide surgeons in prosthesis selection.
Our paper is a retrospective case series with small numbers. We
did not use standardized X-rays and the reasons for failure may be
multifactorial.
Conclusion
Early warning regarding unforgiving and technically difficult
prosthesis is valuable, and the AOA NJRR data supports our concerns.
We recommend that surgeons consider their prosthesis selection
carefully with data from multiple sources. In addition to standard
techniques, reducing the body and head height should be considered
with use of this hemiarthroplasty.