Journal of Orthopedics & Rheumatology
Download PDF
Acute zone II flexor tendon injuries of the hand in both genders. Cooperative patients aged more than sixteen years old. Uncooperative patients Age less than sixteen years old Mutilated hand injuries Associated fractures close to the tendon injury Vascular injury requiring revascularization.
Case Series
Repair of Acute zone II flexor tendon injuries using a wide awake technique in the hand
Khaled NA*,Serry MA, Basyoni Y and Mansour W
- Department of Orthopedic Surgery, Faculty of Medicine, Mansoura University Hospital, Egypt
*Address for Correspondence: Nour A Khaled, Department of Orthopedic Surgery, Manusora University Hospital, Egypt, E-mail: kk_nour@yahoo.com
Citation: Khaled AN. Adipofascial Posterior Interosseous Reverse Flap for Soft Tissue Loss on Dorsal Aspect of the Hand. J Orthopedics Rheumatol. 2018; 5(2): 11.
Copyright: ©2018 Khaled NA. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 5, Issue: 2
Submission: 29 September, 2018 |Accepted:29 October, 2018| Published:31 October, 2018
Abstract
Introduction:Flexor tendon injuries of the hand are a challenging task for surgeon due to the peculiar anatomy of the tendons passing through flexor tendon sheaths, surgeons have to avoid increasing the bulkiness of the tendon through its sheath, as this may affect the functional results of the tendon repair.
Methods:Prospective study has been conducted targeting patients with acute zone II flexor tendon injuries admitted at Orthopedic department in Mansoura Emergency Hospital within the period from February 2016 till February2018, and their follow up for minimum three months at outpatient clinic of Upper limb and Hand surgery unit, Mansoura university orthopedic center.
Conclusion and recommendation:Using the wide awake technique provides an optimal opportunity to test repair strength making the surgeon much more comfortable to initiate early active motion. Besides, rising trend toward using early active rehabilitation protocol in case of strong repair using four or more strand repairs is recently supported in literature.
Keywords
Hand; Flexor tendon injuries; wide awake technique
Introduction
Flexor tendon injuries of the hand are a challenging task for surgeon due to the peculiar anatomy of the tendons passing through flexor tendon sheaths, surgeons have to avoid increasing the bulkiness of the tendon through its sheath, as this may affect the functional results of the tendon repair [1].
The goals of surgical treatment of a lacerated intra-synovial flexor tendon have remained constant: accurate cooptation of the tendon ends in such a manner as to allow application of a postoperative rehabilitation protocol that encourages tendon gliding, inhibits the formation of peritendinous adhesions, stimulates restoration of the gliding surface, allows for primary healing of the repair site, and ultimately restores normal range of motion to the finger [2].
However, being operated under general or brachial plexus block anesthesia to allow use of tourniquet for hemostasis, the tensile strength and intra-synovial smooth gliding of the repair can’t be assessed actively intraoperative [3]. As a result, tendon adhesion, rupture of the repair and triggering are still present in clinical practice even in fewer incidences than before. Also complications of tourniquet, even rare, still may occur.
Vanishing the concept of epinephrine danger in the finger has permitted us to use epinephrine as a hemostatic with lidocaine as an anesthetic in hand surgery, therefore we can use such combination to perform flexor tendon repairs on wide-awake comfortable patients with no tourniquet [4]. Wide-awake technique permits the intraoperative active movement enabling surgeons to detect tendon repair gapping, any gliding difficulties or non-tendinous intersection in the repair site and correct them before skin closure thus decreasing incidence of complications occurring with the conventional methods [3].
As the FDS enters the fibrous flexor sheath on the palmer aspect of the proximal phalanx (P1), it splits encircling the FDP tendon and rejoins deep to it forming the Camper’s chiasm then inserts by separate slips into the middle phalanx (P2). The FDP tendon runs through the fibrous flexor sheath initially deep to the FDS, then superficial distal to Camper’s chiasm and finally as the single tendon distal to the FDS insertion to be inserted into the base of the distal phalanx (P3) [5].
Abbreviations
FDS: Flexor Digitorum Superficialis; FDP: Flexor Digitorum Profundus.
Patients and Methods
Patients
After approval of local ethical committee of Mansoura faculty of medicine, this Prospective study has been conducted targeting patients with acute zone II flexor tendon injuries admitted at Orthopedic department in Mansoura Emergency Hospital within the period from February 2016 till February2018, and their follow up for minimum three months at outpatient clinic of Upper limb and Hand surgery unit, Mansoura university orthopedic center.
A Written informed consent explaining the whole procedure under study in this search has been obtained from all patients and absolute confidentiality as regard the patient’s names and addresses has been taken in consideration.
Inclusion criteria
Exclusion criteria
As shown in figure, twenty six patients with acute zone II flexor tendon injuries have been operated by the wide awake technique, but only twenty two patients were included in this study having fulfilled the inclusion and exclusion criteria of this study while the remaining four patients were discarded as they didn’t complete the minimum follow up period of three months.
Methods
I) Initial Assessment:Twenty two Patients with zone II flexor tendon injuries were seen at emergency room and thorough examination and assessment was conducted including:
History taking
The range of age of the patients was from 16 to 41years old, 16 patients were males and 6 patients were females, 14 patients had hard manual or industrial work, while 8 patients had office jobs or domestic work.
None of patients involved in the current study were diabetic, hypertensive nor having other debilitating diseases. 16 patients were injured by knife and 3 others were injured by broken glass, while the remaining 3 patients were injured by other sharp instruments. 13 patients were assaulted by others, while the other 9 patients were accidentally injured.
All patients were recently injured and managed by primary tendon repair within 24 hours from injury. 14 patients had left hand injuries, 6 patients had right hand injuries and only 2 patients had both hand injuries.
In the current study, 22 patients had 32 digits injured. 17 patients had single digit injury, while 5 others had multiple digit injuries. The involved digits were distributed as follows: 3 thumb fingers, 4 index fingers, 7 middle fingers, 10 ring fingers, 8 little fingers.
Thorough clinical examination
A) The digital nerve injuries: Static two-point discrimination (s2PD) and in some cases moving two-point discrimination (m2PD) are the prevailing techniques to indicate sensory recovery after surgical digital nerve repair. Thus, there were 10 cases 6 of them have good outcome, while 4 of them have poor out come as shown in the article.
B) Local neurovascular assessment: Radial and ulnar digital nerves of the affected fingers were examined. 10 fingers had digital nerve injuries while the remaining 22 fingers were neurologically free.
All patients in the current study had intact distal vascularity with average digital pulp capillary refill time (2-6 seconds).
C) Assessment of the skin coverage: All patients had viable edges of injured wounds and were closed primarily with no need for skin reconstruction.
D) Assessment of the tendon integrity: 3 digits had zone II FPL tendon injuries. 29 digits had zone II FDP tendon injuries; among them 10 digital FDS tendons were intact, while the remaining 19 digits had both FDS and FDP tendons injured.
Radiological assessment
All patients had two views plain X-ray on the hand region and none of them had associated injuries whether fracture, dislocation,nor foreign body.
Then, the fascial paddle dissection is extended to the radial side. The ascia is gradually lifted from the Extensor Carpi Radialis Brevis (ECRB) and Extensor Digitorum Communis (EDC) muscles. Several septa have to be sectioned (between the ECRB and EDC and between the EDC and EDM) but we do not incise the septum between the EDM and the ECU. Lifting EDM to allow good evaluation of the septocutanous perforators, then the posterior interosseous nerve is isolated. The posterior interosseous artery is temporary closed by bulldog at its proximal part, the tourniquet is released and the perfusion of the flap is assessed. Ligation of posterior interosseous artery and rotation of flap through cutaneous tunnel with precaution to avoid rotation or kinking of pedicle. Inset of slap and secure to recipient site via interrupted absorbable sutures.finally the flap is covered with split thickness skin graft. The donor site is closed primary in layers. Bulky non-tight dressing is applied; the wrist is splinted in 10 degrees dorsiflexion.
I) first aid management: Intravenous antibiotics were initiated immediately in all cases. Primary wound care, cleaning gross contamination and sterile dressing, was conducted then below elbow slap was applied till time of operation. Pre-operative laboratory investigations, including only complete blood picture and bleeding profile, were requested for all patients.
II) Operative management
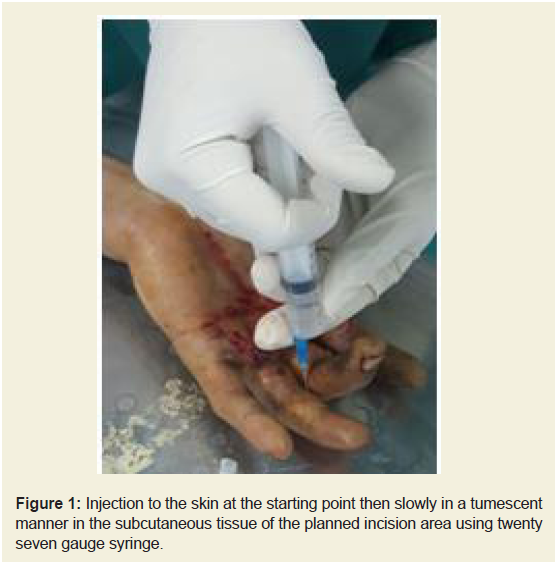
Wide-awake anesthesia: Starting at least 1cm beyond the proximal starting point of incision, a mixture of 1% Lidocaine HCL and 1:100,000 Epinephrine prepared and buffered by adding 8.4% sodium bicarbonate at a volume ratio of 1 ml: 10 ml to the mixture was injected at first perpendicular to the skin at the starting point then slowly in a tumescent manner in the subcutaneous tissue of the planned incision area using twenty seven gauge syringe as shown in (Figure 1).
Figure 1: Injection to the skin at the starting point then slowly in a tumescent manner in the subcutaneous tissue of the planned incision area using twenty seven gauge syringe.
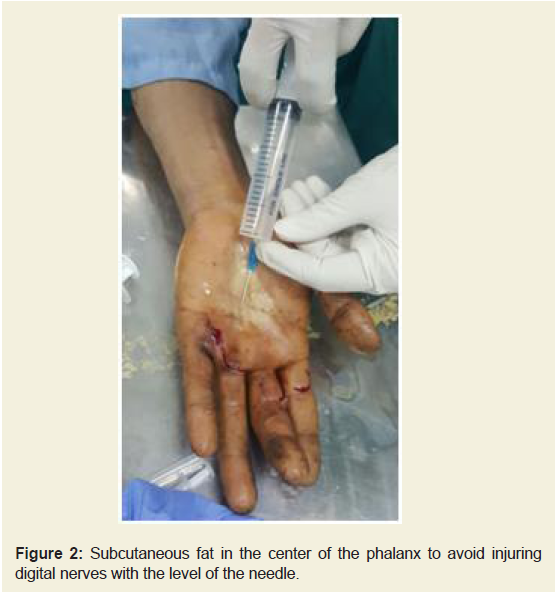
Finger injections were all in the subcutaneous fat (2-3 cc per phalanx) in the center of the phalanx to avoid injuring digital nerves with the bevel of the needle as shown in (Figure 2).
Figure 2: Subcutaneous fat in the center of the phalanx to avoid injuring digital nerves with the level of the needle.
Under local anesthesia the isolated integrity of FDP and FDS were checked again and confirmed pre-operative provisional diagnosis.
A gap period between anesthetic injection and beginning of the surgical procedure ranging from 25 to 30 minutes has been considered in all patients to get optimal hemostasis.
Sterile, deflated cuff of pneumatic tourniquet was applied to ipsilateral upper arm, as precautions in case of failure or intolerance WALANT technique.
The surgical approach
After proper positioning and draping of the patient, the wound was extended nearly 2 to 3 cm proximally and distally in zig zag incisions (Bruner approach).
Thorough debridement and irrigation was done, after that accurate evaluation of injured structures including neurovascular bundle, tendons and tendon sheath was conducted.
Tendon repair procedure
A) Retrieving the tendon ends: Preserving the fibrous sheath and the pulley system was taken in consideration during dissection to avoid postoperative bowstringing. However venting a sufficient part of the pulley to retrieve and effectively repair the injured tendon was done, but not exceeding two centimeter incision in the fibrous sheath, nor completely venting the most significant A2 and A4 pulleys.
According to the injury level and location of the torn tendon in relation to the significant A2 pulley, retrieval of the tendon was done by either of the following methods:
Injury at subdivision II A and II B “distal to A2” with nonretracted tendon was directly retrieved by fine toothed forceps with liability of venting the most distal part of A2 pulley, or the proximalpart of A4 to retrieve the proximal or the distal stump of the injured tendon respectively, and either C1, A3, C2, or all of them could be retrieved safely.
Injury at subdivision IIC “under A2 pulley” with retracted proximal stump usually required proximal extension of the main incision or adding a separate skin incision just proximal to A1 pulley to retrieve the tendon and pass it, using a small nylaton catheter or the tube part of scalp vein set, through A2 pulley which could have been partially vented either proximally or distally according to the injury level.
Injury at subdivision IID “proximal to A2” was easily retrieved after venting A1 and sometimes proximal A2 pulleys.
B) Repairing the tendon ends: In the current study, all FDP tendons were repaired by cruciate single cross stitched locked four strand method using 3/0 polypropylene (prolene TM) strand as a core suture followed by simple continuous running epitenon sutures using 5/0 prolene strand, while torn FDS tendons were excised except in zone IID were repaired the same manner as FDP tendons.
C) Intraoperative assessment of tendon repair: After placing the core suture, the patient was asked to actively flex and extend his or her finger to detect suture gapping or gliding difficulties to predict liability for postoperative rupture of the repair or triggering respectively.
In the current study only two fingers had intraoperative suture gapping and were managed by repeating the core suture while five fingers had intraoperative gliding difficulties and were managed by trimming the edge of the repair, then dilatation and partial venting of the nearby pulley.
After tendon repair was conducted, neurovascular bundle was assessed again and the previously detected ten digital nerve injuries were repaired by epineurial neurorrhaphy using 7/0 prolene strand. No single case of iatrogenic neurovascular injury was detected in our study.
Finally skin incision was stitched using 4/0nylon strand simple or mattress sutures and a static splint was applied to put the wrist joint at neutral position, the metacarpo-phalangeal joints at 60° flexion and inter-phalangeal joints in full extension.
IV) Postoperative management:Within the 1st 24 hours, neruovascular integrity of the affected fingers and patient competency to intra-operatively educated wound care and mobilization program were confirmed, then all patients were discharged in the day after surgery after being instructed to attend weekly for clinic visit in the first month then twice monthly in the second and third months and finally once monthly till the end of follow up.
Passive digital flexion and extension was started from the first day to obtain optimal passive free motion before early active motion especially in edematous fingers.
By the third to the fifth day, after edema subsidence, patients were instructed to start early active mobilization in the form of ten repetitions hourly of midrange active flexion and extension in splint with slowly increasing the range of flexion over the first three weeks;however, it was not possible to gauge patient compliance.
In each clinic visit, wound healing and repaired tendons were assessed to early detect wound and or tendon healing complications respectively. Patients were instructed to gradually increase range of active flexion and extension but still within the splint.
Removing skin stitches was postponed to the second week in most cases to avoid skin dehiscence with active motion.
By the fifth week, the splint was discarded then gentle loading exercise and light daily activities were allowed.
After six weeks, patients have started physiotherapeutic program to release adhesions and increase finger range of motion.
After three months, resisted “strengthening” exercises and full use of the hand were allowed.
The postoperative mobilization protocol was not modified by the presence of a concomitant digital nerve injury.
Results
Surgery related data
Pain response of patients , measured using the visual analogue scale, during injecting the wide-awake anesthesia had a median score of two with a range of 0 - 4 while during the operative procedure itself the median was zero with a range of 0 - 4.
After exposing both digital flexor tendons and their fibrous sheath, it was noticed that most of FDP injury was in zone II C (44.8%) followed by zone II A or II B (41.4%) with the least cases at zone II D (13.8%). Assessment of FDS tendons revealed that 34.5% of tendons were intact; while 65.5% of tendons were torn among them only 13.8% were repaired being in zone II D.
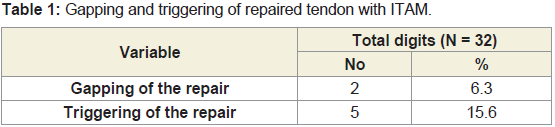
As shown in (Table 1), after applying the core suture, Intra- Operative Total Active Movement (ITAM) revealed that two fingers (6.3%) acquired gapping of the repair necessitated repeating the core suture, while five fingers (15.6%) acquired triggering necessitated trimming the edge of the repair and partial venting of the nearby pulley.
Overall results
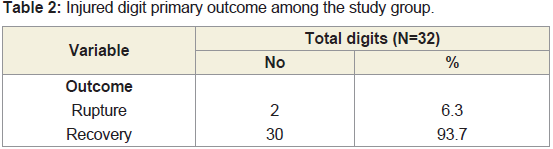
Twenty two patients with thirty two digital flexor tendon injuries included in this study were followed for at least three months with the mean follow up period 4.6 ± 2.3 Months during which tendon rupture rate “primary outcome” recovery of ROM and hand grip strength “secondary outcome” were detected.
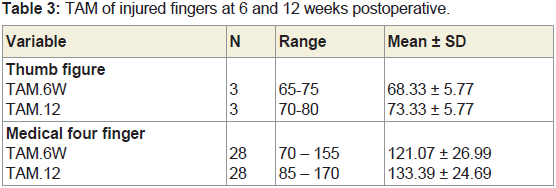
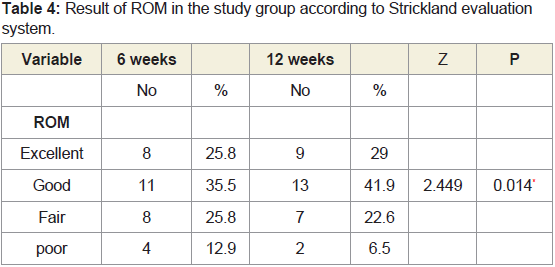
As shown in (Table 2), on contrary to 6.3% rupture rate, the overall recovery of range of motion was 93.8%. The mean values of TAM, measured according to Strickland evaluation, for the thumb finger and the medial four fingers separately were 68.33 ± 5.7 and 121.1 ± 26.99 respectively at six weeks postoperatively which increased to 73.33±5.7 and 133.4 ± 24.69 respectively at twelve weeks postoperatively. This is clearly demonstrated in (Table 3 and 4). In other words, there is significant improvement in ROM from 6 to 12 weeks post-operative.
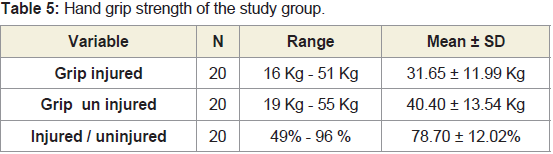
After excluding two cases with bilateral digital injuries, for absence of reference value, the mean values of injured and uninjured hand grip strength were 31.65 Kg ± 11.99 and 40.40 Kg ± 13.54 respectively with an average recovery of 78.70% ± 12.02of the injured hand grip strength in relation to the uninjured hand. This is clearly demonstrated in (Table 5).
C. Correlation between variables
In the coming figures, the collected demographic, injury related, and surgery related data have been tabulated in comparison to the final outcome and relevant statistical tests have been applied to detect studied variables of statistical significant values that could affect results.
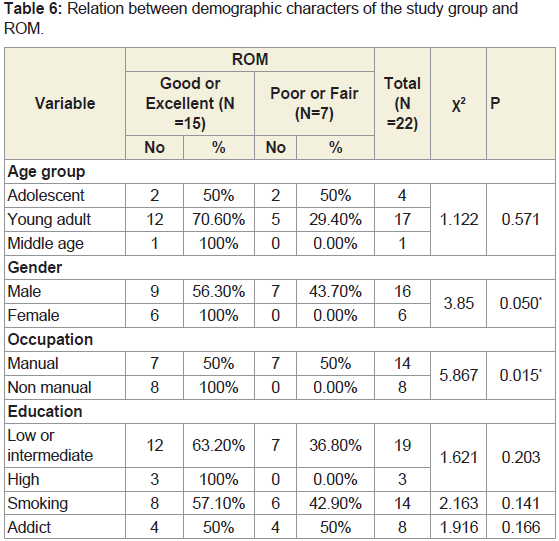
It’s obvious from (Table 6) that there’s significant association between better ROM and female gender and non- manual work, while age, level of education, smoking, and addiction have no significant statistical relation with ROM in the current study.
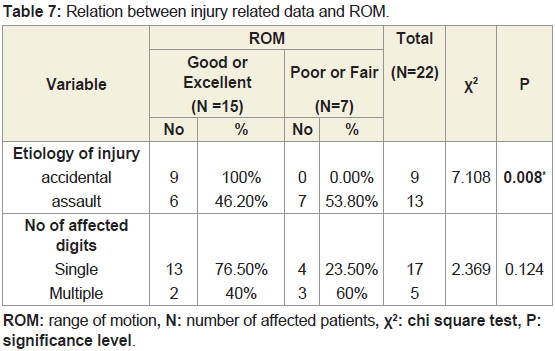
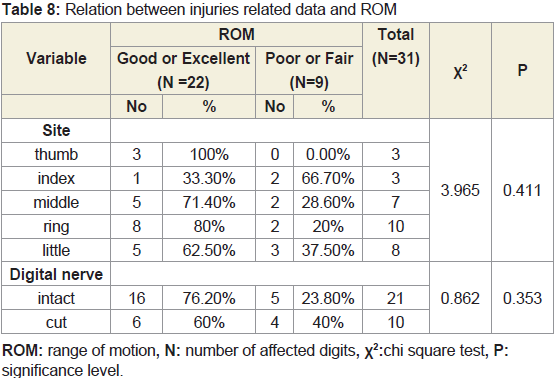
As shown in (Table 7 and 8), there is no significant statistical relation between ROM and injury related factors in the current study except for significant association between being assaulted and having bad ROM.
ROM: range of motion, N: number of affected patients, X2: chi square test, P: significance level.
ROM: range of motion, N: number of affected digits, X2:chi square test, P: significance level.
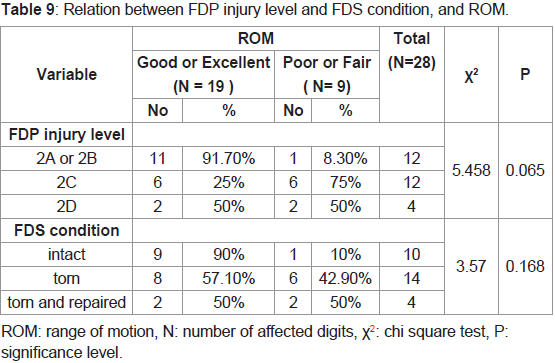
It’s obvious from (Table 9) that there’s no statistical significance between ROM and FDP injury level and FDS condition whether intact or not.
ROM: range of motion, N: number of affected digits, Χ2: chi square test, P: significance level.
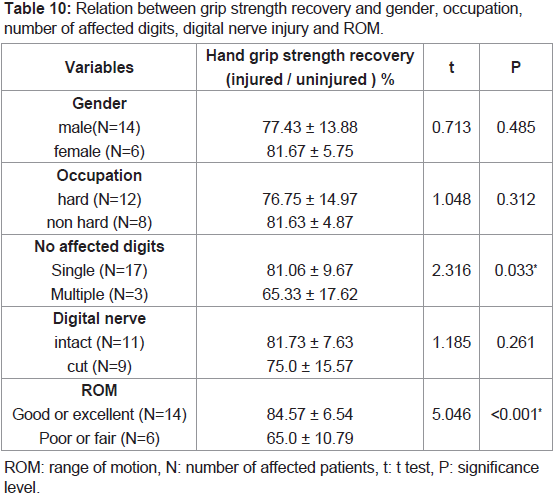
Table 9: Relation between FDP injury level and FDS condition, and ROM.Hand grip strength has no standard value, but has wide physiologic variations in normal population so its absolute value can’t be used to detect factors affecting tendon repair. Therefore, percentage of recovered hand grip strength in relation to that of the contra lateral hand was used as a reference value to exclude effect of physiologic factors and properly detect factors affecting grip strength recovery. The figures in (Table 10) summarize the relation between variables involved in this study and percentage of grip strength recovery. Strong association between single digit injuries and better ROM, and favorable grip strength recovery is well noticed as demonstrated in figures.
ROM: range of motion, N: number of affected patients, t: t test, P: significance level.
Table 10: Relation between grip strength recovery and gender, occupation, number of affected digits, digital nerve injury and ROM.D. Complications
The overall incidence of complications was 18.8% (6 digits) in the form of tendon rupture (6.3%, 2 digits), superficial wound infection (9.4%, 3 digits) and poor ROM (6.3%, 2 digits) with single digit having both wound infection and poor ROM. There were no other complications whether related to anesthesia and local epinephrine injection or related to iatrogenic neuro-vascular injury. Also there were no other postoperative complications like deep wound infection or complex regional pain syndrome.
Discussion
Comparison between the results of current study and other studies from the literature is difficult and because the results of flexor tendon repair is influenced by many factors such as patient age, cause and severity of injury, case selection, preoperative delay, technique of repair, postoperative rehabilitation program and the patient compliance [2].
However, great effort was exerted to find comparable studies that, to high extent, match with current study making this comparison meaningful. In this study, patients with acute flexor tendon injuries in zone II were managed by primary repair using wide awake technique. Rehabilitation was done by using early active motion protocol and results were expressed according to original Strickland evaluation system. This figure is quite similar to Caulfield et al., 2008, Sandow and McMahon 2011, Braga-Silva and Kuyven 2005, Starnes et al., 2012, Al-Qattan, 2011 and Klein 2003 in the way that they did primary repair of flexor tendons in zone II, used early active motion protocol and adopted original Strickland evaluation system to express their results [6-11]. However, these studies are different in the way that they operated their patients using the conventional anesthetic method either general or brachial block anesthesia. As a result, another study done by Higgins et al., 2010 was involved, despite being slightly different from the previously mentioned studies, to compare our experience in the recently introduced wide awake technique with the literature [12].
Our sample consisted of 22 patients (32 digits) whose mean age was 28.7 years (range between 16-41 years) with male: female ratio of 2.7:1. The sample size in current study is close to that described by Braga-Silva and Kuyven, 2005 (82 patients, 82 digits) more than that described by Starnes et al., 2012 (21 patients, 24 digits), more than that described by Al-Qattan 2011 (5 patients, 20 digits)[8-10]. Observing the mean age and gender distribution in current study which goes with the study described by Starnes et al., 2012 (mean age: 42 ± 3, male to female: 2.4:1), predominance of young male category is noticed [9]. This can be explained by the fact that this category is more active and more liable to injury.
The most common category met in this study was non-highly educated (86.4%) and manual workers (63.6%). When comparing to what Starnes et al., 2012 described that non university graduates represented 62% of his patients, while manual workers represented only 29%, we can conclude that these figures are socially dependent and can be explained by the fact that they are more exposed to work related injuries.
Pain response of patients, measured using the visual analogue scale, during injecting the wide-awake anesthesia had a median score of two with a range of 0-4 while during the operative procedure itself the median was zero with a range of 0-4 meaning that the technique is nearly painless which is so hopeful pushing the author to continue using it being satisfactory for patients.
In this study, the locally injected epinephrine was highly effective and adequately sufficient to give bloodless field during the whole procedure with no need to another hemostatic method whether applying tourniquet or using diathermy and with no single case of epinephrine related complications.
In the current study, tendon repair was done using 3/0 prolene cruciate single cross stitched locked four strand core suture followed by 5/0 prolene simple continuous epitendenous suture. This goes with what Barrie et al., 2001 in his biomechanical study about the effect of suture locking and suture caliber on fatigue strength of flexor tendon repairs concluded that four strand cross-stitch locked repair with a 3-0 suture had significantly improved fatigue strength and holding capacity compared with the other repairs tested (2 & 4 strand repair either non locked or locked using either 3/0 or 4/0 sutures) [13].
All FDP tendons in the current study were injured and repaired. As regard FDS tendons, 34.5% were intact; while 65.5% were torn. Non-repairing injured FDS tendons was preferred in this study to avoid adhesion with repaired FDP tendons especially under the narrow tunnel of A2 bullae (zone IIC) that can’t be completely vented , and due to difficulty of repairing the thin sheet like FDS tendon close to its insertion at zones IIA and B. As a result, only 13.8 % of FDS tendons in current study were repaired being in zone IID where FDS tendons are cord like, easily repaired, and located under A1 bullae that can be safely vented completely giving a wide compartment with less risk of adhesion with repaired FDP tendons.
Except for repairing FDS tendons in zone IID, this study is similar to the study described by Al-Qattan, 2011 who recommended only repair of FDP tendons as he used bulky core suture in his study [10]. This opinion is to some extent also supported by Tang, 1994 who recommended only FDP tendon repair in zone IIC [14]. However, studies described by Caulfield et al., 2008, Sandow and McMahon 2011, Braga-Silva and Kuyven, 2005, Starnes et al., 2012, and Klein, 2003 adopted repair of all injured FDS tendons [6-10].
Having an optimal rehabilitation protocol is still questionable. Chesney et al., 2011 in their systematic review of flexor tendon rehabilitation protocols in zone II found that early active motion protocol had superior results to Kleinert or combined Kleinert and Duran protocols in studies that used original Strickland system to evaluate ROM [14,15]. However, they concluded that weak evidence support both early active motion protocols and protocols that combine passive mobilization and active extension as providing superior results with regard to range of motion while maintaining an acceptably low rate of tendon rupture.
Using the wide awake technique provides an optimal opportunity to test repair strength through ITAM making the surgeon much more comfortable to initiate early active motion. Besides, rising trend toward using early active rehabilitation protocol in case of strong repair using four or more strand repairs is recently supported in literature. As a result, this study as well as all previously mentioned studies adopted early active rehabilitation protocol with slight differences among them.
Tendon rupture is an unfavorable outcome that requires return to the operating room for re-repair whether primary or secondary. In this study, tendon rupture rate was 6.3% ( two digits) which is very close to studies described by Braga-Silva and Kuyven, 2005 and Klein, 2003 (rupture rate: 6.1%, 5% respectively) [8,10], but slightly more than what described by Sandow and McMahon, 2011 and Higgins et al. 2010 (rupture rate: 3.9%, 3.3% respectively) [7,11]. Starnes et al. 2012 and Al-Qattan, 2011 had 0% rupture rate [9,10].
In our study, one of the tendon ruptures occurred one week after repair as the patient discarded the back slab. This patient had his tendon re-repaired like primary cases. The other patient had multiple finger injuries. This patient gave a history of jerky movement perceived by his index finger six weeks after repair, after which he complained of pain and marked limitation on motion in this finger in contrary to the other two fingers whose ROM was improving. However, he was presented to us at our follow up clinic four weeks later on. This patient was explored and had two-stage tendon graft. Apart from those two patients, who didn’t follow the strict precautions they perceived after repair and had well documented rupture events that were accidentally induced postoperatively, rupture rate can be considered zero in this study [16,17].
Significant increase in TAM and results of Strickland score from 6 to 12 weeks after repair indicates the importance of extending follow up and rehabilitation program up to 3 months to follow improvement in ROM.
References
- Griffin M, Hindocha S, Jordan D, Saleh M, Khan W (2012) An overview of the management of flexor tendon injuries. Open Orthop J 6: 28-35.
- Strickland JW (1995) Flexor tendon injuries: I. Foundations of treatment. J Am Acad Orthop Surg 3: 44-54.
- Youha SA, Lalonde DH (2014) Update/review: changing of use of local anesthesia in the hand. Plast Reconstr Surg Glob Open 2: e150.
- Fitzcharles-Bowe C, Denkler K, Lalonde D (2007) Finger injection with high-dose (1: 1,000) epinephrine: does it cause finger necrosis and should it be treated? Hand 2: 5-11.
- Goggins T, Syme D, Murali SR (2014) Acute flexor tendon injury and rehabilitation of hand injuries. J Orthop Trauma 28: 219-224.
- Caulfield RH, Maleki-Tabrizi A, Patel H, Coldham F, Mee S, et al. (2008) Comparison of zones 1 to 4 flexor tendon repairs using absorbable and unabsorbable four-strand core sutures. J Hand Surg Eur Vol 33: 412-417.
- Sandow MJ, McMahon M (2011) Active mobilisation following single cross grasp four-strand flexor tenorrhaphy (Adelaide repair). J Hand Surg Eur Vol 36: 467-475..
- Braga-Silva J, Kuyven CR (2005) Early active mobilization after flexor tendon repairs in zone two. Chir Main 24: 165-168.
- Starnes T, Saunders RJ, Means KR Jr (2012) Clinical outcomes of zone II flexor tendon repair depending on mechanism of injury. J Hand Surg Am 37: 2532-2540.
- Al-Qattan MM (2011) Zone 2 lacerations of both flexor tendons of all fingers in the same patient. J Hand Surg Eur Vol 36: 205-209.
- Klein L (2003) Early active motion flexor tendon protocol using one splint. J Hand Ther 16: 199-206.
- Higgins A, Lalonde DH, Bell M, McKee D, Lalonde JF (2010) Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg 126: 941-945.
- Barrie, KA, Tomak SL, Cholewicki J, Merrell GA, Wolfe SW (2001) Effect of suture locking and suture caliber on fatigue strength of flexor tendon repairs. J Hand Surg Am 26: 340-346.
- Tang JB (1994) Flexor tendon repair in zone 2C. J Hand Surg Br 19: 72-75.
- Chesney A, Chauhan A, Kattan A, Farrokhyar F, Thoma A (2011) Systematic review of flexor tendon rehabilitation protocols in zone II of the hand. Plast Reconstr Surg 127: 1583-1592.
- Lalonde D, Bell M, Benoit P, Sparkes G, Denkler K, et al. (2005) A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie Project clinical phase. J Hand Surg Am 30: 1061-1067.
- Chowdhry S, Seidenstricker L, Cooney DS, Hazani R, Wilhelmi BJ (2010) Do not use epinephrine in digital blocks: myth or truth? Part II. A retrospective review of 1111 cases. Plast Reconstr Surg 126: 2031-2034.