Journal of Orthopedics & Rheumatology
Download PDF
Case Series
Scaphoid Excision and Four Corner Fusion Using Anti-Grade Headless Compression Screws in the Management of Stage I and II SNAC Wrists
Nour A Khaled*and Abed Y
- Department of Orthopedic Surgery, Faculty of Medicine, Mansoura University Hospital, Egypt
*Address for Correspondence: Nour A Khaled, Department of Orthopedic Surgery, Faculty of Medicine, Mansoura University Hospital, Egypt, E-mail: kk_nour@yahoo.com
Citation: Khaled NA, Abed Y. Scaphoid Excision and Four Corner Fusion Using Anti-Grade Headless Compression Screws in the Management of Stage I and II SNACWrists. J Orthopedics Rheumatol. 2018; 5(2): 6.
Copyright: ©2018 Khaled NA. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 5, Issue: 2
Submission: 14 August, 2018Accepted: 24 September, 2018 Published: 01 October, 2018
Abstract
Introduction: Scaphoid Nonunion Advanced Collapse (SNAC) is a common cause of traumatic wrist degeneration. Scaphoid excision and Four-Corner Fusion (4-CF) has been shown to be an effective treatment option to relieve pain and in the same time preserve a good functional range of wrist motion.
In current study, we evaluated the functional outcome of 4-CF with excision of the Scaphoid for the treatment of stage II and III SNAC wrist fixed using two converging anti-grade headless compression screws.
Methods: Between 2010 and 2017, 34 patients with SNAC stage II and III were managed by 4-CF, excision of the Scaphoid and fixation by two converging anti-grade headless compression screws. The modified Mayo wrist score system MMWS was used for clinical assessment. The average preoperative MMWS was 47.5 only patients with minimum follow up period 12 months were included in this study.
Results: After an average final follow up of 43.24 months, solid union was achieved in all cases in an average time of 70.38 days. The average postoperative MMWS was 80. It was excellent in 8 patients (23.5%), good in 11 patients (32.4%), fair in 14 (41.2%) patients and poor in 1 (2.9%) patients.
Conclusion: The 4-CF with excision of the Scaphoid using antigrade headless compression screws provides a reliable treatment option for advanced SNAC wrist stage II and III. Anti grade insertion of the screws did not have a deteriorative effect on the final outcome. This technique provides reliable functional outcome with a high rate of union and low rate of complication.
Keywords
Four-corner fusion; Limited wrist arthrodesis; SNAC; Screws; Wrist arthritis
Introduction
The Scaphoid is the corner stone articulation between both carpal rows [1].Scaphoid Fracture and nonunion results in disturbance of the normal carpal bone biomechanics resulting in abnormal movement behavior and increased stresses across the inter-carpal articulations. This when left untreated will eventually end in a progressive collapse of the carpal bone followed by development of radio-carpal osteoarthritis known as Scaphoid Nonunion Advanced Collapse (SNAC) [2,3].
The SNAC wrists pass into three sequential time related degenerative changes. In stage I, there is narrowing of the jointspace between the tip of the radial styloid process and the distal outer aspect of the Scaphoid. In stage II, the degenerative changes affect the entire radio-Scaphoid articular surface. In stage III, the degenerative changes affect the capito-lunate joint. Whatever the stage of SNAC wrist, the radio-lunate joint was always spared from the degenerative process and this provided the basic principles for the most commonly used motion preserving salvage procedures [4,5].
Before the development of motion preserving salvage procedures, total wrist fusion was generally the only reliable treatment available for end-stage SNAC wrist arthritis [3]. However, complete pain relief after total wrist fusion was not guaranteed and complete loss of wrist motion result in significant functional disability [6].
Among the different salvage procedures, Scaphoid excision and four-corner fusion (4-CF) between the lunate, capitate, hamate and triquetrum has become widely accepted treatment option for stage II or III SNAC wrist arthritis with good long term results. This technique addresses multiple aspects of the SNAC wrists. Scaphoid excision serves as a resection gap arthroplasty to solve the arthritic changes of the radio-Scaphoid joint and the mid-carpal fusion solves he mid-carpal arthritis or the instability created after excision of the Scaphoid. This would be expected to provide stable, painless wrist joint and in the same time preserve the widest feasible wrist range of otion [5-11].
The 4-CF was conventionally fixed with multiple k-wires that usually require a prolonged time of immobilization until secure fusion was detected [8]. However, in order to provide adequate compression of the fusion sites with sufficient stability to allow early range of motion that would be expected to improve the functional outcome, other methods of fixation were used including headless compression screws [10], staples and circular plates [12]. However, the ideal method of fixation of the four corner fusion is still a debatable issue [12,13].
In this study, we evaluated the functional outcome of 4-CF with excision of the Scaphoid for the treatment of stage II and III SNAC wrist fixed using two converging anti-grade headless compression screws.
Patients and Methods
Between 2010 and 2017 thirty four patients with Scaphoid nonunion SNAC stage II and III were managed by 4-CF, excision of the Scaphoid and fixation by two converging anti-grade headless compression screws.
The modified Mayo wrist score system MMWS was used for clinical assessment preoperatively and in the last follow up post operatively [13,14]. The average preoperative MMWS was 47.5 (range: 10-70) and it was poor in 24 patients (70.6%) and fair Vin 10 patients. The average pre operative grip strength was 48.9% (range: 20-80%) compared to the other healthy side. The average preoperative wrist flexion was 46.5° (range: 30-65°). The average preoperative wrist extension was 41.2° (range: 30-60°). The average preoperative total arc of motion was 87.8° (range: 55-125°). The average preoperative visual analogue score (VAS) was 6.5.The average disability of the Arm, Shoulder and Hand (DASH) Score was 54.7 (range: 28-78).
All patients had radiological evaluation for evidence of nonunion of the Scaphoid with stage II or III SNAC wrists. Only patients with follow up more than 12 months were included in this study (Figure 1).
In the preoperative counseling, the benefits of the surgery, the alternative surgical options and the expected outcome were carefully explained. It is very important to clearly demonstrate that 4-CF is a motion preserving salvage procedure aiming to preserve or slightly increase the existing range of motion.
Surgical technique
In the supine position under regional or general anesthesia, the affected upper limb was supported on a side radiolucent hand surgery table and a proximal pneumatic tourniquet was applied. A 6-8 cm dorsal midline skin incision was centered over the radio-carpal joint in line with the axis of the third metacarpal bone. The subcutaneous tissue was dissected off the extensor retinaculum creating thick flaps that protect the dorsal cutaneous nerves within these flaps.
Then the retinaculum over the third dorsal compartment was incised over the course of the extensor pollicis longus tendon which was released and retracted. Through the third compartment the fourth compartment was approached creating ulnarly based retinacularflaps that can be repaired later. The extensor tendons of the forth compartment were retracted to expose the dorsal wrist capsule.
Partial wrist denervation was done by isolation of the terminal branch of the posterior interosseous nerve and neurectomy was performed by excision of a 2 cm nerve segment and cauterizing the proximal end of the nerve to avoid formation of a painful terminal neuroma.
A ligament-preserving capsulotomy was performed by dividing the dorsal wrist capsule along the dorsal intercarpal and dorsal radiocarpal ligaments creating a z-shaped capsular incision that when repaired would be expected to minimize capsular contracture, and thus help to improve final wrist range of motion [15]. A radially based capsular flap was elevated off the triquetrum and reflected exposing the carpal bones.
The articular surface between the radius and lunate (lunate fossa) was carefully inspected for arthritic changes and if normal, excision of the Scaphoid was done either in piecemeal or as one unit. This may be facilitated by insertion of a 2.5 mm schanz along the longitudinal axis of the Scaphoid and use it as a joystick to manipulate the Scaphoid. During Scaphodectomy, care should be taken to protect the volar radio-carpal ligaments including the radio-scapho-capitate and long radio-lunate ligaments as its injury may result in ulnar translocation of the remaining carpus. Radial styloidectomy may be performed if required to prevent wrist radial impingement.
The fusion site was prepared by removing the articular surfaces down to the subchondral bone of the capito-lunate, capito-hamate, triquetro-hamate and luno-triquetral joints. This can be done sharply by scalpel and completed using a small curette or small high speed burr. Multiple drill holes were created using a k-wire in the subchondral bone of the opposing surfaces of the fusion site to increase the vascularity. A 1-2 mm of articular cartilage rim should be spared at the volar and proximal aspects of the fusion site. The volar articular rim help to prevent injury of the volar wrist ligaments and proximal articualr rim helps to prevent injury the articular surface of the fused lunate and triquetrum forming the carpal surface of the radio-carpal articulation.
The reduction of the lunate in relation to capitate is the keystone to improve the final range of motion after 4-CF. A k-wire was inserted in the dorsum of the lunate in line with its longitudinal axis to be used as a joystick to help in the reduction. The lunate was brought in the radial and dorsal direction in relation to capitate. The lunate should slightly over ride the capitate in order to prevent dorsal impingement of the capitate with the radius and to increase the range of wrist extension. Pushing the wrist joint in the ulnar and dorsal direction help in the reduction of the lunate and decreases the stress created on the lunate joystick k-wire. The position of the lunate in relation to the capitate was checked under C- Arm control and preliminary fixed by a k-wire inserted in a retrograde fashion from the dorsal aspect of the capitate to the volar part of the lunate or anti-grade from the dorsal aspect of the lunate into the capitate. Then the lunate joystick k-wire was removed.
Sufficient amount of cancellous bone graft was harvested from the distal end of the radius in the ordinary way and was packed in between the four bones of the four corner fusion site. Part of the excised Scaphoid was denuded from its articular cartilage, cut into pieces and backed into the void created in the distal radius after harvesting the bone graft.
Then maximum flexion of the wrist was done to insert an antegrade guide wire of a headless screw through the center of the lunate articular surface into the center of the capitate under C-Arm control. A suitable size headless screw was inserted from the lunate to the capitate to compress the fusion site in between. Copious irrigation was used during insertion of the guide wire and during drilling to avoid thermal injury to the articular surface. The temporary k- wire was then removed.
A second guide wire was inserted by blunt dissection through a separate stab wound just below the styloid ulna from the triquetrum passing through the hamate to the capitate bone under C-Arm control. This was facilitated by radial deviation of the wrist. A suitable headless screw was inserted to compress the three bones together.
The remaining bone graft was inserted into the fusion site. It is always preferred not to over compress the fused joints by inserting sufficient bone graft in the fusion sites in order to maintain the carpal height and normal relation of the fused bones. The final position of the screws was checked by C-Arm and the final wrist passive range of motion was tested.
The z-shaped ligament sparing capsulotomy was repaired, the extensor tendons were relocated, and the extensor retinaculum edges were approximated to prevent bowstringing of the extensor tendons. The extensor pollicis longus was transposed dorsal to the extensor retinaculum. After release of the pneumatic tourniquet adequate haemostasis was done, and the skin incision was closed.
The limb was immobilized in a bulky below elbow wrist and thumb splint with the wrist in a neutral or slight extension position. Early active finger range of motion exercises was started on the first postoperative day along with pain and oedema control measures.
Two weeks after the operation, the splint and sutures were removed and a custom made removal hand and thumb splint was used for another two weeks. Passive and assisted active wrist motion was allowed as tolerated. Serial follow up x-ray were done and with evidence of radiological union, patients started hand therapy program to improve the range of motion and strength of the affected limb.
At final follow up, the functional outcome was assessed using the MMWS [14].
Tips and tricks
1. Partial wrist denervation.
2. A ligament-preserving capsulotomy in (Z) shaped mannerto minimize capsular adhesions, and thus help to improve range of motion.
3. Manipulation of Scaphoid using a wire as joystick to facilitate its excision and and no effort should be saved to protect volar radiocarpal ligaments including radioscaphocapitate ligaments.
4. Adequate careful curettage of articular cartilage of opposing surfaces of capitate, lunate triquetrum, and hamate
5. Reduction of lunate dorsal and radial to capitate to avoid dorsal impingement.
6. The position of the lunate overriding the capitate was checked under C- Arm control and temporarily fixed by a k-wire.
7. Palmar flexion of wrist to facilitate insertion of the firstheadless screw in ante grade manner from lunate to capitates.
8. Radial deviation of wrist to facilitate insertion of the second screw from triquetrum into hamate and capitate direction.
Results
Statistical analysis
Data entry and statistical analyses were performed using SPSS (Statistical Package of Social Sciences) version 16.0 (SPSS Inc, Chicago, IL, USA). Normality of data was first tested by one sample K-S test .Normally distributed data were summarized by mean and standard deviation (s). Non normal data were expressed in median, minimum and maximum. Paired t test was used to compare normally distributed data in matched groups. However, Wilcoxon signed rank test was used to compare none normally distributed matched groups. In addition, independent t test was used to compare means for continuous variables of each two different groups. Also, Mann- Whitney U test (z) was used to compare none normally distributed continuous variables in two different groups. P value < 0.05 was considered as statistically significant.
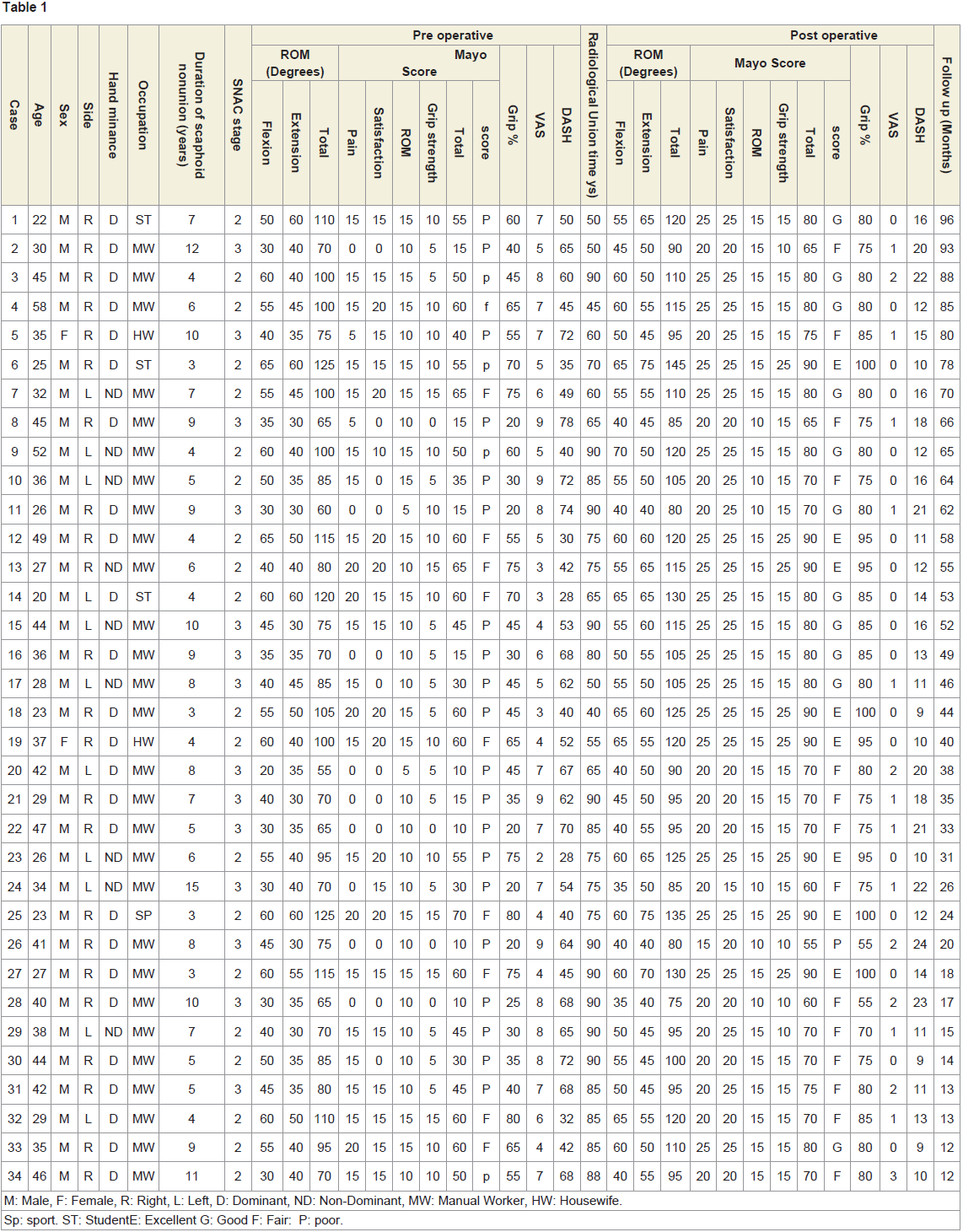
After an average final follow up of 46.3 months (range: 12- 96 months), solid union was achieved in all cases. The average time of radiological union was 70.38 days (range; 40-90 days). The average postoperative MMWS improved to 80 (range: 55-90). This improvement was statistically significant (p<0.05). It was excellent in 8 patients (23.5%), good in 11 patients (32.3%), fair in 14 patients (41.2%) and poor in 1 patient (2.9%). The average postoperative grip strength improved to 81.9% (range: 55-100%) compared to the other healthy side. This improvement was statistically insignificant (p<0.05). The average postoperative VAS improved to 0 (range: 0-3). The average postoperative DASH score improved to 14.7 (range: 9-24). The improvement in VAS and DASH was statistically significant (p<0.05). All patients returned to their pre injury activities xcept for one patient (Table 1). (Figures 2 and 3).
The average post operative wrist flexion was 52.9° (range: 35-70°), the average postoperative wrist extension was 54.1° (range: 40-75°) and the average total range of motion was 106.9° (55-90°).
Two patients developed complex regional pain syndrome and were treated by oral medications, proper physiotherapy and active hand movements. No dorsal impingement of the capitate and radius were observed among our cases.
Discussion
The consistent sparing of the radio-lunate articulation from the degenerative process in the SLAC and SNAC wrists constitute the basic principle of the two most commonly used motion preserving salvage procedures; the Proximal Row Carpectomy (PRC) and the 4-CF [7].
The PRC is indicated in the early degenerative stages (stages I and II) when the lunate-capitate articulation is spared from the degenerative process. Several modifications of the technique of the PRC have been proposed to increase the spectrum of indication to stage III degenerative wrist including the capsular interposition and capitateprosthetic resurfacing with variable results [15,16].
Numerous studies compared the outcome of using both techniques in the degenerative wrists and stated that PRC provided better wrist range of motion, better grip strength, early return to daily activities and avoided the complications associated with the use of metallic implants (nonunion of fusion site, implant related complications) [15,17]. On the other hand, early radio-carpal arthritis developed more often with PRC and higher rate of failure were reported with young active high demand patients younger than 35 years old [18,19]. The average age of the patients in the current study was 35.6 years old and more than 80% were high demand active patients.
On the other hand, 4-CF is indicated in young active patients with advanced stage III degeneration affecting the articular surface of the capitate, where the PRC is not indicated and is expected to fail [20-23]. Fourteen patients (41.2%) in the current study had stage III SNAC wrists.
The 4-CF was conventionally fixed by using multiple K-wire fixations and later staples and headless screws were used for fixation in order to improve the fusion rate and allow early mobilization of the wrist [8,10,12]. Recently, different designs of dorsal plate fixation have been used with variable results [20,21,24].
Unacceptable high rate of complications and poor functional outcome were reported with the early introduction of the circular plate fixation. Nonunion, dorsal impingement and inability to visualize the fusion site that was obscured by the plate were the commonest reported complications [22,24]. However, several modifications have been introduced to improve the outcome of using plate fixation in 4-CF with promising results. Using locked dorsal plates, recessed plates and radiolucent plates had improved the outcome of dorsal late fixation [13,20,23,25]Several studies compared the outcome of 4-CF using conventional methods of fixation in comparison to the more expensive, more sophisticated locked dorsal plate; failed to prove the superiority of the plate fixation over conventional methods of fixation [13,25,26].
The headless compression screws gained an increasing popularity since its introduction in the fixation of 4-CF due to the simplicity of the technique, low cost compared to the dorsal plate, high rate of union, early wrist mobilization and few limited complications [10,11,27,28].
In current study, we used two converging anti-grade headless compression screws to stabilize and compress the 4-CF fusion site. Thus, reducing the costs and using the minimal hardware to fix the bones, facilitated the imaging and the verification of state of the fusion. Increasing the number of the screws used in the fusion site increased the incidence of complications related to the prominence of the screws leading to irritation of the soft tissues that usually occurred ith the dorsal plates where 8 screws were used for fixation [26].
Several techniques for screws insertion in 4-CF have been described in the literature. Retrograde insertion of the screws from capitate into the lunate has been described to avoid violation of the lunate articular surface [11,29,30]. Other studies using the anti-grade insertion of the screws from the lunate into the capitates, argued that the screw placement in cartilage of the lunate does not injure its surface due to the small diameter of the screws producing a small hole in the lunate articular surface that is progressively filled by fibrinous tissue as reported in anti-grade screw placement in proximal Scaphoid fractures [31,32]. In the current study, we used anti-grade converging insertion from the lunate into the capitate and from the triquetrum through the hamate into the capitate compressing all the four bones of the 4-CF together. We used copious saline irrigation during drillingto minimize the thermal injury to the articular cartilage [33]. The antigrade screw insertion is technically easier and provided better direct compression of the fusion site. The anti-grade direct insertion of the screws from the small lunate into the larger capitate is technically less demanding than the retrograde insertion were the entry point of the screw is not visible [10].
In the current study, all cases united in an average time of 70.38 days, which is within the limit of the range reported in the literature (ranging between 1 and 4.5 months) [8,11,20,33-35]. The high rate of union in a relatively shorter time reported in our study could be attributed to the stable compression of the fusion site provided by the converging screws, adequate meticulous preparation of the fusion site and adequate graft harvested from the distal radius. The reported nonunion rate in the literature range from 0% to 63%, depending on the surgical technique and the method of fixation used [7,8,10,11,25-31,33,34].
The functional outcome was evaluated both preoperatively and at the final follow-up using the MMWS [14]. The average postoperative MMWS significantly improved from 47.5 preoperatively to 80 postoperatively (P <0.05). Excellent and good results were achieved in 55.88% of patients. The average VAS improved significantly from 6.5 preoperatively to postoperatively (P <0.05). The average DASH score improved significantly from 54.7 (range: 28-78) preoperatively to 14.7 (range: 9-24) postoperatively (P <0.05).The improvement of the grip strength from an average preoperative value of 48.9% (range: 20-80%) to an average postoperative value of 81.9% (range: 55-100%) of the contra-lateral healthy side observed in this study correlates well with other published reports although it was statistically significant [8,11,24,28].
The average total arc of motion of the wrist in this study improved from an average 87.8° preoperatively to an average of 106.9° postoperatively, which was better compared to the 49° to 80° reported in the literature [11,24,28]. The main improvement was in the range of postoperative wrist extension. The early mobilization protocol adapted in this study along with ligament sparing capsulotomy and meticulous surgical technique as regard relation between lunate and capitate helped to improve the final total arc of motion [16,32,36,37].
El Mowafi et al. in their study using the MMWS reported that the improvement in subjective parameters (pain and patient satisfaction) greatly affected the final functional score more than the objective parameters (the wrist range of motion and the grip strength) [8]. In current study, in addition to improvement in pain and patient satisfaction, improvement of the grip strength affected the final outcome.
Few insignificant complications occurred in the current study. Two patients (5.88%) developed reflex sympathetic dystrophy and were treated by oral medications, proper physiotherapy and active hand movements. We did not encounter hardware related complications (screw breakage, screw backing out through lunate) nor capitate radial impingement. In Ozyurekoglu et al. study screw penetration of the lunate proximal cortex occurred in 2 cases (6%) the same was reported by Gaston et al. reported the rate of complications in the literature varies between 9% up to 40% [5,8,11,38].
In our study, we did not have to abort the salvage 4-CF and convert it to total wrist fusion in any of our patients after an average follow up of 46.3 months (range: 12-96 month). Sixteen patients (47.05%) in our study were followed up more than four years. The reported rates of conversion of 4-CF to total wrist fusion in the literature varies from 2.4% to 29% [11,26,27]. Trail et al. in a long follow up study (9 years and 4 months (range 3-19 years)) reported that 6 out of 110 patients (5.5%) required total wrist fusion that was done within the first two years after the initial operation [36].
However, in another long follow up study, Bain and Watts reported that the function of the wrist, the scores for pain [37], and the range of motion were comparable when evaluated at 1year or at 10 years after 4-CF. Neubrech et al. reported the same findings in even a longer follow up study with a mean follow up 13.6 years (range: 10-19 years) indicating the durability of the result of the 4-CF and that the result did not deteriorate with time [38].
Conclusion
The 4-corner fusion with excision of the Scaphoid using antigrade headless compression screws provides a reliable treatment option for advanced SNAC wrist stage II and III. Anti-grade insertion of the screws did not have a deteriorative effect on the final outcome. This technique provides a reliable functional outcome with a high rate of union and low rate of complication.
References
- Weber ER (1980) Biomechanical implications of scaphoid waist fractures. Clin Orthop Relat Res 149: 83-89.
- Oka K, Moritomo H, Murase T, Goto A, Sugamoto K, et al. (2005) Patterns of carpal deformity in scaphoid nonunion: a 3-dimensional and quantitative analysis. J Hand Surg Am 30: 1136-1144.
- Laulan J, Marteau E, BacleG (2015) Wrist osteoarthritis. Orthop Traumatol Surg Res 101(1 Suppl): S1-S9.
- Gelberman RH, Cooney WP 3rd, Szabo RM (2000) Carpal instability. J Bone Joint Surg Am 82: 578-594.
- Shin AY (2001) Four-corner arthrodesis. J Am Soc Surg Hand 1: 93-111.
- Sauerbier M, Trankle M, Linsner G, Bickert B, Germann G (2000) Midcarpal arthrodesis with complete scaphoid excision and interposition bone graft in the treatment of advanced carpal collapse (SNAC/SLAC wrist): operative technique and outcome assessment. J Hand Surg Br 25: 341-345.
- Ozyurekoglu T, Turker T (2012) Results of a method of 4-corner arthrodesis using headless compression screws. J Hand Surg Am 37: 486-492.
- Hernekamp JF, Reinecke A, Neubrech F, Bickert B, Kneser U, et al. (2016) Four-corner fusion: comparison of patient satisfaction and functional outcome of conventional K-wire technique vs. a new locking plate. Arch Orthop Trauma Surg 136: 571-578.
- Smith BS, Cooney WP (1996) Revision of failed bone grafting for nonunion of the scaphoid. Treatment options and results. Clin Orthop Relat Res 327: 98-109.
- Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP 3rd, et al. (1989) Scaphoid malunion. J Hand Surg Am 14: 679-687.
- Luegmair M, Houvet P (2012) Effectiveness of four-corner arthrodesis with use of a locked dorsal circular plate. Clin Orthop Relat Res 470: 2764-2770.
- Wyrick JD, Stern PJ, Kiefhaber TR (1995) Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg Am 20: 965-970.
- Laulan J, Bacle G, de Bodman C, Najihi N, Richou J, et al. (2011) The arthritic wrist. II-the degenerative wrist: indications for different surgical treatments. Orthop Traumatol Surg Res 97(4 Suppl): S37-S41.
- Wall LB, Didonna ML, Kiefhaber TR, Stern PJ (2013) Proximal row carpectomy: minimum 20-year follow-up. J Hand Surg Am 38: 1498-1504.
- Di Donna ML, Kiefhaber TR, Stern PJ (2004) Proximal row carpectomy: study with a minimum of ten years of follow-up. J Bone Joint Surg Am 86: 2359-2365.
- Shindle MK, Burton KJ, Weiland AJ, Domb BG, Wolfe SW, et al. (2007) Complications of circular plate fixation for four-corner arthrodesis. J Hand Surg Eur 32: 50-53.
- Bedford B, Yang SS (2010) High fusion rates with circular plate fixation for four-corner arthrodesis of the wrist. Clin Orthop Relat Res 468: 163-168.
- Kendall CB, Brown TR, Millon SJ, Rudisill LE Jr, Sanders JL, et al. (2005) Results of four-corner arthrodesis using dorsal circular plate fixation. J Hand Surg Am 30: 903-907..
- Merrell GA, McDermott EM, Weiss AP (2008) Four-corner arthrodesis using a circular plate and distal radius bone grafting: a consecutive case series. J Hand Surg Am 33: 635-642.
- Rhee PC, Shin AY (2013) The rate of successful four-corner arthrodesis with a locking, dorsal circular polyether-ether-ketone (PEEK-Optima) plate. J Hand Surg Eur Vol 38: 767-773.
- Rodgers JA, Holt G, Finnerty EP, Miller B (2008) Scaphoid excision and limited wrist fusion: a comparison of K-wire and circular plate fixation. Hand (N Y) 3: 276-281.
- Collins ED, NollaJ (2008) Spider plate fixation: no significant improvement in limited wrist arthrodesis. Tech Hand Up Extrem Surg 12: 94-99.
- Greenberg A, Shreve M, Bazylewicz D, Goldstein R, Sapienza A (2013) Early motion following 4-corner arthrodesis using cannulated compression screws: a biomechanical study. J Hand Surg Am 38: 2180-2187.
- Ball B, Bergman JW (2012) Scaphoid excision and 4-corner fusion using retrograde headless compression screws. Tech Hand Up Extrem Surg 16: 204-209.
- Henry M (2009) Internal headless compression screw method for 4-corner fusion. J Hand Microsurg 1: 45-49.
- Mamede J, Adeodato SC, Leal RA (2017) Four-corner arthrodesis: description of surgical technique using headless retrograde crossed screws. Hand (NY) 13: 156-163.
- Martus JE, Bedi A, Jebson PJ (2005) Cannulated variable pitch compression screw fixation of scaphoid fractures using a limited dorsal approach. Tech Hand Up Extrem Surg 9: 202-206.
- Goubier JN, Teboul F (2007) Capitolunate arthrodesis with compression screws. Tech Hand up Extrem Surg 11: 24-28.
- Houston DA, Amin AK, White TO, Smith ID, Hall AC (2013) Chondrocyte death after drilling and articular screw insertion in a bovine model. Osteoarthritis Cartilage 21: 721-729.
- Korus LJ, Ball B, Morhart M (2013) Exclusion of the hamate in 4-corner fusion:technique and outcomes of a novel approach to intercarpal arthrodesis. Tech Hand Up Extrem Surg 17: 102-105.
- Van Amerongen EA, Schuurman AH (2009) Four-corner arthrodesis using the quad memory staple. J Hand Surg Eur 34: 252-255.
- Dvinskikh NA, Blankevoort L, Strackee SD, Grimbergen CA, Streekstra GJ (2011) The effect of lunate position on range of motion after a four-corner arthrodesis: a biomechanical simulation study. J Biomech 44: 1387-1392.
- Hernandez-Soria A, Das De S, Model Z, Lee SK, Wolfe SW (2016) The effect of capitate position on coronal plane wrist motion after simulated 4-corner arthrodesis. J Hand Surg Am 41: 1049-1055.
- Gaston RG, Greenberg JA, Baltera RM, Mih A, Hastings H (2009) Clinical outcomes of scaphoid and triquetral excision with capitolunate arthrodesis versus scaphoid excision and four-corner arthrodesis. J Hand Surg Am 34: 1407-1412.
- Dacho A, Grundel J, Holle G, Germann G, Sauerbier M (2006) Long term results of midcarpal arthrodesis in the treatment of scaphoid nonunion advanced collapse (SNAC-Wrist) and scapholunate advanced collapse (SLAC-Wrist). Ann Plast Surg 56: 139-144.
- Trail IA, Murali R, Stanley JK, Hayton M, Talwalkar S, et al. (2015) The long-term outcome of four-corner fusion. J Wrist Surg 4: 128-33.
- Bain GI, Watts AC (2010) The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg Am 35: 719-725.
- Neubrech F, Muhldorfer-Fodor M, Pillukat T, Schoonhoven JV, Prommersberger KJ, et al. (2012) Long-term results after midcarpal arthrodesis. J Wrist Surg 1: 123-128.