Journal of Orthopedics & Rheumatology
Massive Abdominal Lymphadenopathy as a Manifestation of Connective Tissue Diseases. Report of Two Cases and Review of the Literature
Georgios Yiannopoulos1, Dimitrios Daoussis1, Helen Kourea2, Christina Kalogeropoulou3 and Andrew P. Andonopoulos1*
- Department of Pathology, University of Patras School of Medicine, 265 04 Rion, Patras, Greece
- Department of Radiology, University of Patras School of Medicine, 265 04 Rion, Patras, Greece
*Address for Correspondence: Andrew P. Andonopoulos MD, FACP, Professor of Internal Medicine and Rheumatology, University of Patras School of Medicine — Division of Rheumatology 265 04 Rion, Patras, Greece, Tel: +30.2613.603483; Fax: +30.2610.993982; E-mail: andandon@upatras.gr
Citation: Yiannopoulos G, Daoussis D, Kourea H, Kalogeropoulou C, Andonopoulos AP. Massive Abdominal Lymphadenopathy as a Manifestation of Connective Tissue Diseases. Report of Two Cases and Review of the Literature. J Orthopedics Rheumatol. 2013;1(1): 4.
Copyright © 2013 Yiannopoulos G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 1, Issue: 1
Submission: 25 October 2013 | Accepted: 26 November 2013 | Published: 03 December 2013
Abstract
In this report, massive abdominal lymphadenopathy of the reactive type, related to the underlying disease activity, was described in a patient with systemic lupus erythematosus and another one with mixed connective tissue disease. The diagnosis of this very rare clinical presentation was made after appropriate and meticulous work up that ruled out other possibilities such as infectious or lymphoproliferative diseases. Clinicians should be aware of this rare occurence and, when faced with such a picture, they should appropriately rule out other more serious pathologies, before administering moderate steroid doses targeting the underlying disease.Keywords
Massive abdominal lymphadenopathy; Systemic lupus erythematosus (SLE); Mixed connective tissue disease (MCTD); Reactive lymphadenitisAbbreviations
CTD: Connective Tissue Disease; ANA: Antinuclear Antibodies; anti-dsDNA antibodies: Anti-Double Stranded DNA Antibodies; SACE: Serum Angiotensin Converting Enzyme; CT: Computed Tomography; HRCT: High Resolution Computed Tomography; IBD: Inflammatory Bowel Disease; ILD: Interstitial Lung Disease; PPD: Purified Protein DerivativeIntroduction
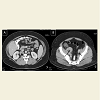
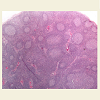
Lymphadenopathy is a relatively common manifestation of connective tissue diseases (CTD), particularly rheumatoid arthritis [1-4], and systemic lupus erythematosus (SLE) [4-7]. The clinically palpable nodes are predominantly located in the axillary and cervical areas and are usually non tender and discrete, varying in size from a few millimeters to 3-4 centimeters. However, massive abdominal/retroperitoneal lymphadenopathy, as a manifestation of the disease itself, is extremely rare and very few cases have been described so far [8,9]. When such a massive lymphadenopathy, especially in the abdomen, is encountered in a CTD patient, the physician’s main concern is to rule out infectious causes [10-16], granulomatous diseases [17], but also malignant, and rarely benign [18-22], lymphoproliferative disorders. We present herein two patients with CTD, one with SLE and the other with mixed connective tissue disease (MCTD), in whom massive abdominal lymphadenopathy was directly related to activity of the underlying disease and not to another cause. The purpose of this presentation, besides reporting a very rare manifestation of CTD activity, is the sensitization of the physician to this rare occurrence which should be included in the differential diagnosis of similar cases, without of course underestimating the importance of prompt and appropriate study to rule out other more serious possibilities.2nd Case: A 47 year old Caucasian lady was diagnosed with MCTD 11 years ago, on the basis of interstitial lung disease (ILD), symmetric polyarthritis, myositis with elevation of muscle enzymes and compatible electromyographic findings, Raynaud’s phenomenon and high titre anti-U1RNP Abs. During the first 2 years after diagnosis, she had received six monthly IV cyclophosphamide pulses and IV methylprednisolone pulses, for treatment of her ILD with favourable response (improvement of pulmonary function and HRCT picture). In early 2005, during an episode of diarrhea, which lasted for 10 days, appropriate investigation including endoscopy did not show findings suggestive of inflammatory bowel disease (IBD) or another specific pathology. This disappeared without modification of her low dose steroid treatment (5mg of prednisone daily). For the next 5 years on regular follow up on an outpatient basis, she had been feeling well on this regimen. In April 2010, she presented with mild-moderate arthritis in the small joints of her hands and atypical abdominal pain, accompanied by elevated serum indices of inflammation. SACE level was normal. Because of the previously suspected IBD, a new lower gastrointestinal endoscopy was performed which was unrevealing. An abdominal CT though showed multiple enlarged lymph nodes, with a diameter more than 3cm along the iliac vessels bilaterally (Figure 3). No other pathology of the abdominal organs was seen, while a chest CT showed no significant findings. In order to exclude a lymphoproliferative process - that might have been related to the previously administered cyclophosphamide - or a specific infection such as extrapulmonary tuberculosis - in view of a positive PPD skin test that the patient exhibited-, she underwent laparoscopic lymph node biopsy. The histologic diagnosis was reactive lymphadenitis with follicular hyperplasia (Figure 4). Appropriate stains and cultures did not reveal any infectious agent, whereas immunohistochemistry ruled out a lymphoproliferative process. On the basis of the above, the whole picture was attributed to the patient’s underlying CTD. She improved immediately after increasing the dose of prednizone to 20 mg/d with prompt resolution of the arthritis and disappearance of the abdominal pain. At the same time, the patient was placed on antituberculous chemoprophylaxis for six months with isoniazid because of the positive PPD skin test. Since then she has remained asymptomatic with gradual decrease of prednisone dose to 5 mg/d, whereas an abdominal MRI has shown reduction in the size of the lymph nodes.
Discussion
We have presented two cases of massive abdominal lymphadenopathy of which, one was observed in a patient with SLE and the other in a patient with MCTD. The lymphadenopathy was proven to be related directly to the underlying CTD, since a meticulous search for any other possible cause was unrevealing. The purpose of this presentation was mainly to report a seemingly very rare occurrence, since such lymphadenopathy has been only twice reported in SLE [8,9] and never in MCTD. This, despite the act that clinically palpable lymphadenopathy is a well recognized manifestation of rheumatoid arthritis and systemic lupus erythematosus [1-7]. In rheumatoid arthritis, the axilla is the most common site of palpable lymphadenopathy, most likely because these nodes drain the inflamed joints of the upper extremities. In SLE, lympadenopathy may be more generalized and is more common in children. It has been suggested that in both diseases, lymph node enlargement accompanies disease activity [4].References
- Fleming A, Dodman S, Crown JM, Corbett M (1976) Extra-articular features in early rheumatoid arthritis. Br Med J 1: 1241-1243.
- Hart FD (1987) Lymphadenopathy in rheumatoid patients. Ann Rheum Dis 46: 645-646.
- Kondratowicz GM, Symmons DP, Bacon PA, Mageed RAK, Jones EL (1990) Rheumatoid lymphadenopathy: a morphological and immunohistochemical study. J Clin Pathol 53: 106-113.
- Calguneri M, Ozturk MA, Ozbalkan Z, Akdogan A, Ureten K, et al. (2003) Frequency of lymphadenopathy in rheumatoid arthritis and systemic lupus erythematosus. J Int Med Res 31: 345-349.
- Dubois EL, Tuffanelli DL (1964) Clinical manifestationsof systemic lupus erythematosus. Computer analysis of 520 cases. JAMA 190: 104-111.
- Shapira Y, Weinberger A, Wysenbeek AJ (1996) Lymphadenopathy in systemic lupus erythematosus: prevalence and relation to disease manifestations. Clin Rheumatol 15: 335-338
- Quismorio FP Jr (2002) Hematologic and lymphoid abnormalities in systemic lupus erythematosus. In: Dubois’ Lupus Erythematosus. (6thedn), Lipincott Williams & Wilkins, Philadelphia, Baltimore, New York, London, Buenos Aires, Hong Kong, Sydney, Tokyo.
- Kitsanou M, Andreopoulou E, Bai MK, Elisaf M, Drosos AA (2000) Extensive lymphadenopathy as the first clinical manifestation of systemic lupus erythematosus. Lupus 9: 140-143.
- Tuinman PR, Nieuwenhuis MBB, Groen E, Kersten MJ (2011) A young woman with generalised lymphadenopathy. Neth J Med 69: 284 & 288.
- Bhandarkar DS, Shah RS, Katara AN, Shankar M, Chandiramani VA, et al. (2007) Laparoscopic biopsy in patients with abdominal lymphadenopathy. J Min Access Surg 3: 14-18.
- Suri S, Gupta S, Suri R (1999) Computed tomography in abdominal tuberculosis. Br J Radiol 72: 92-98
- Abdallah M, Larbi T, Hamzaoui S, Mezlini E, Harmel A, et al. (2011)Abdominal tuberculosis: a retrospective series of 90 cases. Rev Med Interne 32: 212-217.
- Neumann MP, Eng MH, Rholl KS, Swedo GJ, Meranze SG (1992)Disseminated histoplasmosis diagnosed by percutaneous needle biopsy of a retroperitoneal lymph node. A case report. Acta Cytol 36: 527-528.
- Franca CM, Cavalcante EG, Ribeiro AS, Oliveira GT, Litvinov N, et al. (2012) Disseminated histoplasmosis in a juvenile lupus erythematosus patient. Acta Reumatol Port 37: 276-279.
- Sang-Hyon K, Sung-Dong K, Hae-Rim K, Chong-Hyeon Y, Sang-Heon L, et al. (2005) Intraabdominal cryptococcal lymhadenitis in a patient with systemic lupus erythematosus, J Korean Med Sci 20: 1059-1061.
- Tapia O, Villaseca M, Araya JC (2010) Mesenteric cryptococcal lymphadenitis: report of one case. Rev Med Chil 138: 1535-1538
- Warshauer DM, Lee JKT (2004) Imaging manifestations of abdominal sarcoidosis. AJR 182: 15-28.
- Sodhi KS, Suri S, Nijhawan R, Kang M, Gautam V (2005) Rosai- Dorfman disease: unusual cause of diffuse and massive retroperitoneal lymphadenopathy. Br J Radiol 78: 845-847.
- Alganatish JT, Houghton K, Bond M, Senger C, Tucker LB (2010) Rituximab treatment in a child with Rosai-Dorfman disease and systemic lupus erythematosus. J Rheumatol 37: 1783-1784.
- Santana A, Lessa B, Galrao L, Lima I, Santiago M (2005) Kikucci-Fujimoto’s disease associated with systemic lupus erythematosus: Case report and review of the literature. Clin Rheumatol 24: 60-63.
- Vijayaraghavan R, Chandrashekar R, Belagavi CS (2011) Kikucci-Fujimoto’s disease involving mesenteric nodes: a report and review of the literature. BMJ Case Rep doi: 10.1136/bcr.10.2011.4945.
- Kojima M, Nakamura S, Itoh H, Yoshida K, Asano S, et al. (1997) Systemic lupus erythematosus (SLE) lymphadenopathy presenting with histopathologic features of Castleman’s disease. Pathol Res Pract 193: 565-571.
- Radin R (1995) HIV infection: analysis in 259 consecutive patients with abnormal CT findings. Radiology 197: 712-722.