Journal of Ocular Biology
Download PDF
Research Article
Expert Perspectives on the Clinical Practices and Treatment Preferences in the Management of Allergic Conjunctivitis in Indian Settings
Manjula S* and Krishna Kumar M
Department of Medical Services, Micro Labs Limited, Bangalore,
Karnataka, India
*Address for Correspondence:Manjula S, Department of Medical Services, Micro Labs Limited,
Bangalore, Karnataka, India Email Id: drmanjulas@gmail.com
Submission: 20 May, 2025
Accepted: 03 July, 2025
Published: 07 July, 2025
Copyright: © 2025 Manjula S, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited
Keywords:Allergic conjunctivitis; Seasonal Allergic Conjunctivitis;
Perennial Allergic Conjunctivitis; Antihistamines; Alcaftadine;
Fluorometholone; Loteprednol
Abstract
Objective: To assess the clinical practice and treatment
preferences in allergic conjunctivitis (AC) among ophthalmologists in
Indian healthcare settings.
Methods: This cross-sectional study included ophthalmologists practicing in India. A multiple-response questionnaire comprising 23 questions was employed to collect feedback, clinical observations, and experiences related to the management of AC and the routine use of antihistamines. The data were analyzed using descriptive statistics.
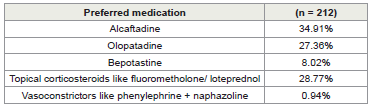
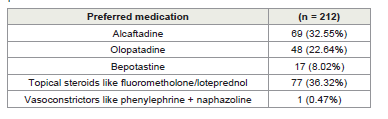
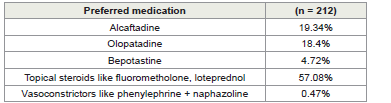
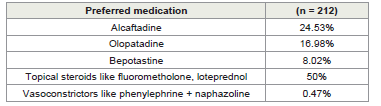
Results: The study included 212 participants, and the majority of them (34.91%) preferred alcaftadine for treating AC in children. Half (50%) of the respondents identified alcaftadine as their antihistamine of choice in routine practice. For managing AC in adults, around 36% favored topical steroids such as fluorometholone or loteprednol. In severe cases, approximately 59% preferred these topical steroids as add-on therapy. Alcaftadine was selected by 38% as the preferred treatment for seasonal AC (SAC) and perennial AC (PAC). For vernal keratoconjunctivitis (VKC), 57% favored topical steroids like fluorometholone or loteprednol, while 50% preferred them for atopic keratoconjunctivitis (AKC). In refractory cases of VKC or AKC, 43% preferred loteprednol. Additionally, more than half (52.83%) preferred alcaftadine for treating AC in lactating women.
Conclusion: This study highlights distinct clinician preferences in the management of AC. Alcaftadine was favored for children, SAC/ PAC, and lactating women, while topical steroids (fluorometholone and loteprednol) were preferred for adults and severe cases, including VKC and AKC. Loteprednol was particularly preferred in refractory VKC/AKC cases.
Methods: This cross-sectional study included ophthalmologists practicing in India. A multiple-response questionnaire comprising 23 questions was employed to collect feedback, clinical observations, and experiences related to the management of AC and the routine use of antihistamines. The data were analyzed using descriptive statistics.
Results: The study included 212 participants, and the majority of them (34.91%) preferred alcaftadine for treating AC in children. Half (50%) of the respondents identified alcaftadine as their antihistamine of choice in routine practice. For managing AC in adults, around 36% favored topical steroids such as fluorometholone or loteprednol. In severe cases, approximately 59% preferred these topical steroids as add-on therapy. Alcaftadine was selected by 38% as the preferred treatment for seasonal AC (SAC) and perennial AC (PAC). For vernal keratoconjunctivitis (VKC), 57% favored topical steroids like fluorometholone or loteprednol, while 50% preferred them for atopic keratoconjunctivitis (AKC). In refractory cases of VKC or AKC, 43% preferred loteprednol. Additionally, more than half (52.83%) preferred alcaftadine for treating AC in lactating women.
Conclusion: This study highlights distinct clinician preferences in the management of AC. Alcaftadine was favored for children, SAC/ PAC, and lactating women, while topical steroids (fluorometholone and loteprednol) were preferred for adults and severe cases, including VKC and AKC. Loteprednol was particularly preferred in refractory VKC/AKC cases.
Introduction
Allergic conjunctivitis (AC) is a common ocular condition,
affecting up to 40% of the population, and is frequently seen by
ophthalmologists and cornea specialists. Its global prevalence has
risen over the past decade, making it one of the most commonly
encountered conditions in clinical practice. However, prevalence
rates vary widely across and within countries, likely due to the
heterogeneous nature of the disease and differences in ethnicity,
allergen exposure, and environmental risk factors. [1,2] It can
significantly impact work performance, educational productivity, and
overall quality of life. The resulting economic burden is substantial,
highlighting the need for targeted health and welfare policies to
address these challenges.[2]
AC affects 6–30% of the general population and up to 30% of
children, either alone or alongside allergic rhinitis.[2] It is a leading
cause of ocular morbidity in children and adolescents, increasingly
recognized as one of the most common pediatric eye disorders.
Seasonal and perennial AC (SAC and PAC) account for 74–95%
of cases, while the less common but more severe forms, vernal
keratoconjunctivitis (VKC) and atopic keratoconjunctivitis (AKC),
pose greater clinical challenges.[3]
The majority of AC cases require pharmacological management.
Dual-acting agents, which both block histamine receptors and
stabilize mast cells, are safe and effective in alleviating the signs and
symptoms associated with AC. [4] Alcaftadine is a multi-action
antiallergic agent that functions as an inverse agonist at H1, H2,
and H4 histamine receptors and also possesses mast cell-stabilizing
and anti-inflammatory properties. Its antihistaminic action helps
relieve itching associated with the early phase of ocular allergic
reactions, while its ability to stabilize mast cells inhibits the release
of pro-inflammatory mediators such as cytokines and lipid-derived
substances involved in the late-phase allergic response. These
combined mechanisms make alcaftadine an effective therapeutic
option for managing AC.[5]
Patients with severe AC often require potent anti-inflammatory
treatments, such as topical corticosteroids and immunomodulators.
Corticosteroids exert both anti-inflammatory and antiproliferative
effects as part of their therapeutic action.[4] They act by inhibiting
multiple components of inflammation, including edema, fibrin
deposition, capillary dilation, leukocyte migration, capillary and
fibroblast proliferation, collagen deposition, and scar formation.
[6] Fluorometholone is effective in managing superficial inflammatory
conditions of the eye.[7] Loteprednol etabonate (LE) is a corticosteroid
that differs structurally from traditional ketone corticosteroids like
prednisolone, featuring a chloromethyl ester substitution at the
carbon-20 position instead of a ketone group. This unique structural
modification is believed to enhance its safety profile, particularly by
reducing the risk of intraocular pressure (IOP) elevation.[8]
This study aimed to evaluate the perspectives of current clinical
management of AC among ophthalmologists in India, with a focus on
disease demographics, preferred pharmacological approaches across
different patient populations.
Methods
We carried out a cross-sectional study among ophthalmologists
from routine healthcare settings across India from June 2024 to
December 2024. The study was conducted after receiving approval
from Bangalore Ethics, an Independent Ethics Committee, which was
recognized by the Indian Regulatory Authority, the Drug Controller
General of India.
A convenient sampling technique was used, and an invitation
was sent to leading ophthalmologists in managing AC in the month
of March 2024 for participation in this Indian survey. About 212
ophthalmologists from major cities of all Indian states, representing
the geographical distribution, shared their willingness to participate
and provide necessary data. The questionnaire booklet titled ASTER
(Alcaftadine Expert Perspective Study in Allergic Conjunctivitis) was
sent to ophthalmologists who were interested in participating in this
study. A 23-item questionnaire assessed treatment preferences for
AC, including medication choices for various patient groups (adults,
children, pregnant women), management strategies for different
subtypes (SAC/PAC, VKC, AKC), approaches to refractory cases, and
the use of adjunctive therapies. Participants were allowed to skip any
questions they did not wish to answer, with unanswered questions
considered unattempted. Clinicians were instructed to complete the
questionnaire independently without consulting colleagues. Written
informed consent was obtained from all participants prior to the
study.
Statistical analysis:
The data were analyzed using descriptive statistics, with categorical
variables expressed as percentages to illustrate their distribution. Each
variable’s frequency and corresponding percentage were reported
to provide a comprehensive overview. To visually represent the
distribution of categorical variables, pie and bar charts were generated
using Microsoft Excel, version 2409, build 16.0.18025.20030.Results
The study included 212 participants. Nearly half of the clinicians
(46.23%) reported managing more than 25 patients with SAC or PAC
per month. The majority (47.17%) indicated that SAC or PAC affects
males and females equally. More than half (58.49%) identified the
age group 6 to 18 years as the most commonly affected. About 36%
observed a higher incidence in urban areas. A substantial proportion
(59.91%) noted that SAC or PAC cases are most frequently
encountered during the summer months. Approximately 60% of
respondents also reported that SAC or PAC is the most frequently
encountered form of AC in their practice. Over half of the participants
(51.42%) indicated that 5 to 25% of their patients with SAC or PAC
also present with systemic allergic conditions. An equal proportion
(38.68%) either opted for a comprehensive panel of investigations,
including serum IgE, eosinophil count, and skin testing or chose not
to rely on any laboratory tests.
Nearly half of the experts (49.53%) indicated that 10–25% of
their patients with SAC or PAC also present with refractive errors.
As per 41% of clinicians, compound myopic astigmatism is the most
frequently associated refractive error in these patients. Approximately
35% of respondents preferred alcaftadine for treating pediatric AC.
Half of the clinicians (50%) expressed a preference for alcaftadine
as the antihistamine of choice. The majority of clinicians (36.32%)
preferred topical steroids such as fluorometholone or loteprednol for
managing AC in adults (Table 2).
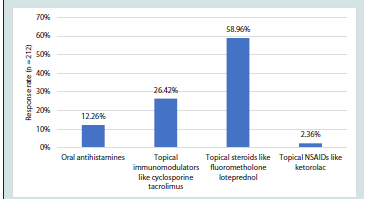
A substantial number of clinicians (58.96%) favored topical
steroids such as fluorometholone or loteprednol as add-on therapy
in cases presenting with severe signs and symptoms of AC (Figure
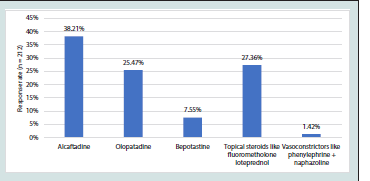
1). The majority of clinicians (38.21%) indicated alcaftadine as their
preferred drug for managing SAC or PAC (Figure 2). Most clinicians
(57.08%) selected topical steroids such as fluorometholone or
loteprednol as their preferred treatment option for VKC (Table 3).
Half of the clinicians (50%) indicated topical steroids such as
fluorometholone or loteprednol as their preferred treatment for AKC
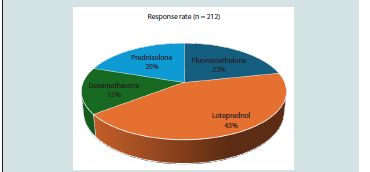
(Table 4). According to 43%, loteprednol is their preferred topical
steroid in refractory cases of VKC/AKC (Figure 3). Over half of the
clinicians (53.77%) favored continuing steroid therapy for more than
two weeks in refractory cases of VKC/AKC. More than half of the
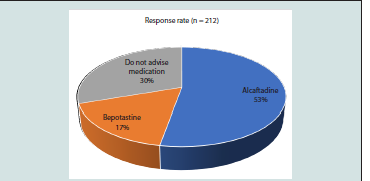
clinicians (52.83%) preferred prescribing alcaftadine for treating AC
in lactating women (Figure 4).
Figure 4: Distribution of responses to preferred antihistamine for treatment
of AC in lactating women
A large proportion of clinicians (75.94%) opted for a combination
of adjunctive measures, including artificial tears and cold compresses,
in the management of AC. Most of the experts (82.08%) observed
that <5% of pregnant women in their practice present with AC.
The majority of clinicians (43.40%) reported that they do not prefer
using a steroid with an antibiotic combination in the treatment of
conjunctival inflammation associated with allergy.
Discussion
The present study results offer a comprehensive overview of
real-world practices in the management of allergic conjunctivitis,
highlighting clinician preferences for managing various forms
of AC across different patient populations. When treating AC in
children, clinicians demonstrated a clear preference for alcaftadine,
with a majority selecting it as their primary treatment option. This
preference extended to the broader category of antihistamine
selection, where half of all surveyed clinicians identified alcaftadine as
their antihistamine of choice. Furthermore, the majority of clinicians
preferred alcaftadine for managing SAC/PAC and in lactating women
with AC.
Several studies in the literature support these preferences. A Phase
III study by Torkildsen et al. involved 58 healthy volunteers aged 10
and older with a history of AC. Alcaftadine 0.25% demonstrated
significant efficacy in reducing ocular itching, conjunctival redness,
and other symptoms of AC at both 15 minutes and 16 hours postadministration,
with no significant safety concerns reported.[9] A
pooled analysis of two multicenter randomized clinical trials by
McLaurin et al. supports the use of alcaftadine 0.25% ophthalmic
solution for preventing ocular itching associated with AC. Compared
to olopatadine 0.2%, alcaftadine 0.25% provided greater relief of
itching 16 hours after administration and was significantly more
effective than placebo and was generally well tolerated.
[10]
Real-world evidence from India also supports these findings.
A study conducted in Northern India by Singh et al. reported that
alcaftadine 0.25% eye drops provided favorable outcomes with fewer
adverse effects. Once-daily administration of alcaftadine 0.25% was
more effective in relieving symptoms of AC compared to twice-daily
olopatadine 0.1% eye drops.[11] Similar findings were reported by
another Indian study by Rajdan et al.[12] Sen et al. found that oncedaily
alcaftadine 0.25% eye drops demonstrated greater efficacy than
once-daily olopatadine 0.2% in relieving the signs and symptoms of
AC.[13] Similarly, Gowda et al. reported that alcaftadine 0.25% was
more effective than olopatadine hydrochloride 0.1% in reducing the
severity of AC.[14]
Greiner et al. demonstrated that treatment with alcaftadine 0.25%
ophthalmic solution led to a significant improvement in symptoms,
with mean reductions of more than 1 unit in ocular itching and
approximately 1 unit in conjunctival redness compared to placebo.
[15] A meta-analysis of 12 randomized controlled trials (1,064
patients) found alcaftadine more effective than olopatadine. Although
symptom scores were similar on day 3, alcaftadine significantly
reduced ocular symptoms by day 7 and 14 and improved conjunctival
hyperemia by day 14.) [16]
In adult patients with AC, the treatment approach shifts notably
toward topical steroids, with a majority of clinicians preferring
fluorometholone or loteprednol. A randomized controlled trial
by Li et al. demonstrated that fluorometholone was effective in
managing chronic AC in adults, providing faster symptom relief
than pranoprofen, particularly in younger patients.[17] Fujishima
et al., 0.02% fluorometholone significantly improved both subjective
symptoms, such as itching, watering, discharge, and foreign body
sensation, and objective signs, including conjunctival injection,
edema, papillae, and corneal involvement, after one week of treatment
in patients with AC.[18] Ilyas et al. found that loteprednol etabonate
0.2% is a safe topical steroid for long-term use in the treatment of
both SAC/PAC.[19] A meta-analysis by Wu et al. involving eight
studies found that topical loteprednol significantly improved signs
and symptoms of AC compared to placebo. Loteprednol showed
efficacy comparable to olopatadine and fluorometholone, with higher
improvement rates in clinical signs (RR = 1.53) and symptoms (RR
= 1.29).[8]
The preference for topical steroids becomes more pronounced in
cases presenting with severe signs and symptoms, where nearly 59%
of clinicians in the current survey indicated these as their preferred
add-on therapy. For more severe forms, such as VKC and AKC,
fluorometholone or loteprednol were favored, with 57% and 50% of
clinicians selecting these options, respectively. In refractory cases of
VKC/AKC, loteprednol was identified as the preferred topical steroid
by the majority of clinicians.
A randomized controlled trial by Chen et al. reported that
both fluorometholone alone and in combination with azelastine
are effective in relieving the signs and symptoms of severe allergic
conjunctival disease.[4] The combination of sodium cromoglycate and
fluorometholone eye drops resulted in a 100% therapeutic response
in patients with AC. [20] Tahir et al. suggested that fluorometholone
may be a more effective treatment option for severe VKC. Among
individuals with a baseline severity score of ≥6, fluorometholone
achieved an effectiveness rate of 90.7%, compared to 72.1% for
cyclosporine.[21] Gupta et al. demonstrated a progressive and
statistically significant reduction in symptoms such as itching, watery
discharge, and photophobia from day 7 to day 30 with the use of
fluorometholone in patients with VKC.[22] Deep et al. demonstrated
that loteprednol was more effective than bepotastinebesilate in
treating patients with VKC. Loteprednol showed significantly greater
improvement in symptoms such as itching, tearing, photophobia, and
clinical signs, including upper tarsal papillae, limbal involvement,
keratitis, and discharge.[23] Oner et al. reported that loteprednol was
effective in the short-term treatment of patients with VKC and was
not associated with any side effects during this period.[24]
By highlighting distinct patterns in medication choices, such
as the preference for alcaftadine in children and lactating women,
and topical steroids like fluorometholone and loteprednol in adults
and severe cases, the study provides valuable, practical guidance
for ophthalmologists and allergists. The study utilized a carefully
designed and validated questionnaire, ensuring that expert opinion
was rooted in evidence-based practices. However, several limitations
of the study should be acknowledged. As a survey-based investigation,
it relies on clinicians’ reported preferences rather than objective
clinical outcomes or randomized controlled trials. The geographic
distribution and areas of specialization of the respondents are not
clearly defined, which may limit the generalizability of the findings.
Additionally, the reliance on expert judgment introduces the potential
for reporting bias, as individual perspectives and preferences could
have influenced the reported conclusions. These limitations should
be considered when interpreting the results, and further research is
needed to validate and expand upon the findings.
Conclusion
The study highlights distinct patterns in clinician preferences for
managing AC, with alcaftadine emerging as the preferred treatment
for children, SAC/PAC, and lactating women. For adults and more
severe presentations, including VKC and AKC, topical steroids,
particularly fluorometholone and loteprednol, were clearly preferred.
Loteprednol was specifically favored for refractory cases of VKC and
AKC.
Acknowledgement
We would like to thank all the ophthalmologists who were actively participating in this study.
Disclosure of compliance with ethical principles:
The study was conducted after receiving approval from Bangalore
Ethics, an Independent Ethics Committee, which was recognized by
the Indian Regulatory Authority, Drug Controller General of India.