Journal of Ocular Biology
Download PDF
Case Report
Treating Acquired Optic Disc Pit Maculopathy with an Ocular Hypotensive Agent
Alex L Song, Mark P. Ghassibi and Eric Shrier*
Department of Ophthalmology, SUNY Downstate Health Sciences
University, Brooklyn, NY, USA
*Address for Correspondence: Eric Shrier DO, Department of
Ophthalmology, SUNY Downstate Health Sciences University, 450 Clarkson
Ave., Room B7-302, MSC 58 Brooklyn, NY 11203, USA Tel: 718-270-1714
Email: eric.shrier@downstate.edu
Submission: 27-June-2023
Accepted: 21-July-2023
Published: 24-July-2023
Copyright: © 2023 Song AL, et al. This is an open-access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Purpose: To describe a case of glaucomatous optic disc pit maculopathy
that resolved after bimatoprost treatment.
Observations: A 63-year-old African American female with a history
of type 2 diabetes mellitus presented to the clinic after 3 months of blurry
vision in the right eye and was found to have an asymmetric cup-to-disc
ratio, and right intraretinal and subretinal fluid without leakage on fluorescein
angiography concerning for optic disc pit maculopathy. A trial of intravitreal
anti-vascular endothelial growth factor (VEGF) injection failed to resolve the
fluid. Optical coherence tomography of the ganglion cell complex showed
thinning of the ganglion cell complex concerning for previously undiagnosed
glaucoma, and the patient was started on bimatoprost. The previously noted
fluid resolved, and the patient has been quiescent for 4 years on ocular
hypotensive medication.
Conclusion: In untreated or poorly controlled glaucoma, progressive cupping of the optic nerve head may lead to the development of an acquired optic disc pit, which can produce maculopathy. This maculopathy can improve under ocular hypotensive treatment.
Conclusion: In untreated or poorly controlled glaucoma, progressive cupping of the optic nerve head may lead to the development of an acquired optic disc pit, which can produce maculopathy. This maculopathy can improve under ocular hypotensive treatment.
Introduction
A 63-year-old African American female was referred for
evaluation of possible central serous chorioretinopathy in the right
eye. The patient noted blurred vision in the right eye for 3 months
without interval improvement. Past medical history was significant
for type 2 diabetes mellitus treated with metformin. She denied any
previous known ocular history.
Best corrected visual acuity was 20/100 in the right eye and
20/30 in the left eye. Intraocular pressure was 14 mmHg in each eye
(Goldmann applanation tonometry). There was no relative afferent
pupillary defect (RAPD). Anterior segments were both unremarkable
with no signs of significant ocular surface diseases, or corneal edema.
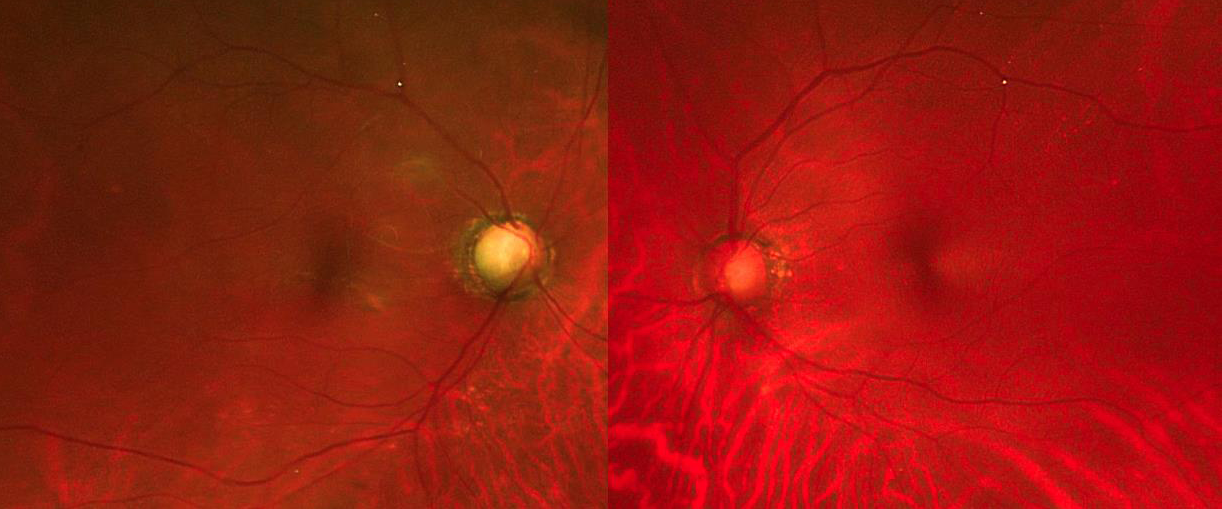
Mild nuclear sclerotic cataractswere noted bilaterally.The fundus of
the right eye compared to the left eye was notable forasymmetry in
the cup-to-disc (C:D) ratio and subretinal fluid nasal to the fovea
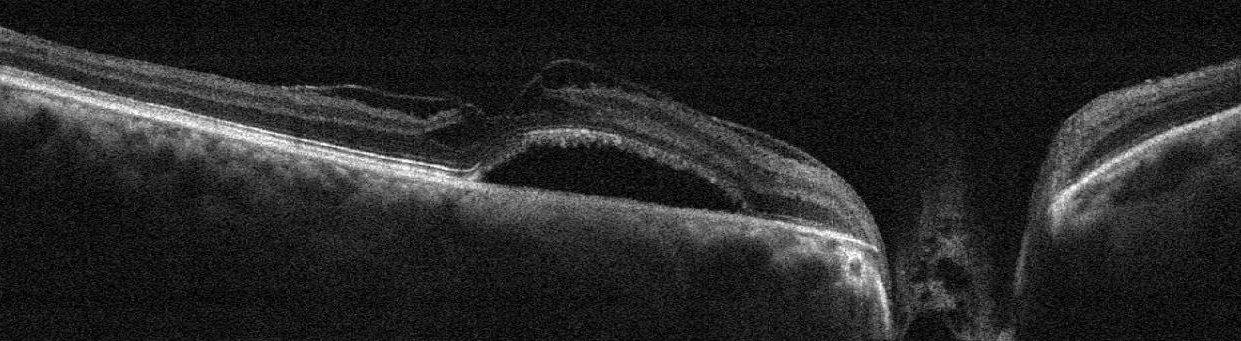
[Figure 1]. The optical coherence tomography (OCT) performed
through the right eye demonstrated the elevation nasal to the foveal
center, and the cross-sectional view was notable for subretinal fluid
and intraretinal fluid with macular schisis and deep cupping [Figure 2].
Fluorescein angiography did not show leakage or filling defects.
At this time, the differential diagnoses for the subretinal fluid
involving the macula and the optic nerve head included optic nerve
pit, pathologic myopia, morning glory deformity, and papillorenal
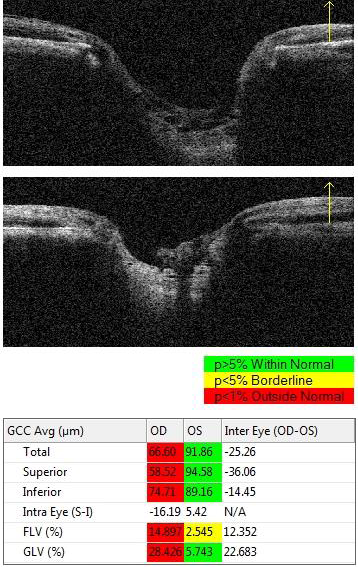
syndrome. OCT of the ganglion cell complex was obtained [Figure 3].
The images were notable for thinning of the nerve fiber layer
(NFL), ganglion cell complex (GCC), and inner plexiform layer (IPL)
more pronounced in the right eye than the left eye. This suggested
that the patient may have had a previously undiagnosed glaucoma,
and the decision was made to start bimatoprost. The patient followed
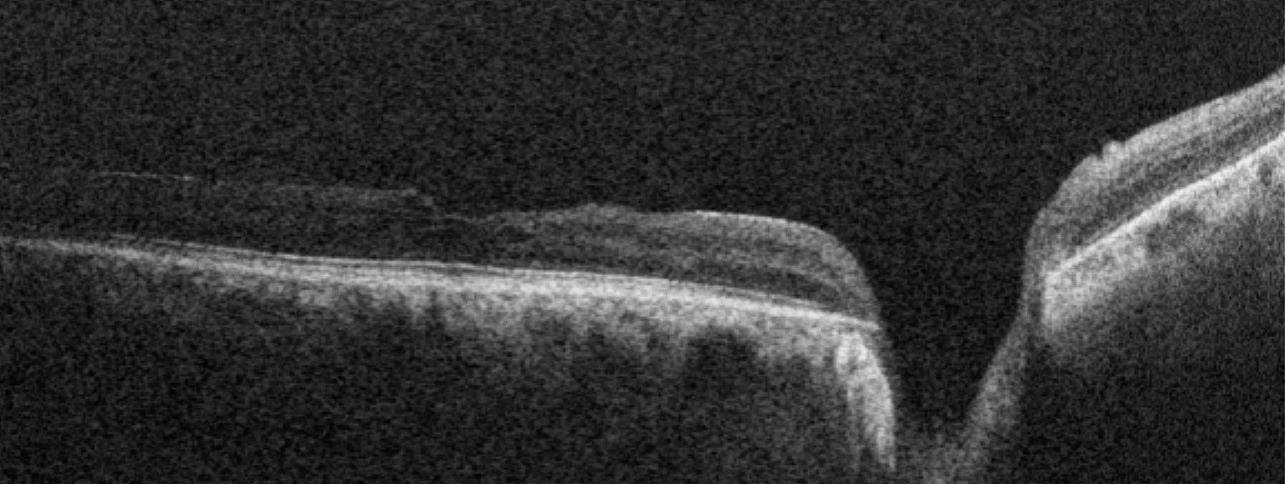
up 3 months later while on bimatoprost. The visual acuity improved
to 20/50 and OCT showed resolution of the subretinal fluid and
improvement in macular schisis and intraretinal fluid [Figure 4].
Therefore, given the clinical course, our diagnosis for the patient was
glaucomatous optic disc pit maculopathy that subsequently resolved
after starting a prostaglandin analog. Throughout the clinical course,
the corneal clarity remained clear.
Discussion
An optic disc pit (ODP) can be acquired as a result of localized
glaucomatous damage [1]. A known complication of an ODP is
maculopathy. It has been reported that an optic disc pit can resolve after
starting ocular hypotensive medicationand that ODP maculopathy
may resolve spontaneous or after posterior vitreous detachment [1,2].
however, this case is the first to show a reversal of glaucomatous ODP
associated maculopathy after topical ocular hypotensive medication,
Figure 1: Color Fundus Photography of Both Eyes: It is notable for asymmetry
in the cup-to-disc (C:D) ratio.
Figure 2: Cross-sectional view of the optical coherence tomography (OCT):
Both subretinal fluid and intraretinal fluid with macular schisis are present with
deep cupping of the optic nerve in the right eye.
Figure 3: OCT map of the ganglion cell complex: Thinning of the ganglion
cell complex is more pronounced in the right eye (top) than in the left eye
(middle). Focal loss volume (FLV) measures the average amount of focal
loss over the entire GCC.
Figure 4: Cross-sectional view of the optical coherence tomography (OCT):
An improvement in the subretinal fluid, intraretinal fluid, and macular schisis
is noted in the right eye.
more specifically, a prostaglandin analog. The patient had previously
documented posterior vitreous detachment, seen in the OCT images,
which implied that changes in the vitreoretinal or vitreo-papillary
interface did not have an effect.
Histologically, optic disc pit is a herniation of dysplastic retinal
tissue through a defect in the lamina cribosa, extending posteriorly
to the subarachnoid space, and may be congenital or acquired [3].
The major complication is optic disc pit maculopathy with fluid
accumulating in the macula [4]. OCT will show a serous retinal detachment with a schisis
cavity and a coexisting detachment of the outer layer of the retinal
pigment epithelium with both IRF and SRF [4]
Once the maculopathy develops, it often begins with a progressive
macular schisis, with fluid that extends through the external limiting
membrane to cause a subfoveal macular detachment and acute vision
loss. Classic treatment options include barrier laser, gas tamponade,
and surgical treatment including PPV and macular buckling, all
of which aim to close the communication between the pit and the
subretinal or intraretinal space. No technique has been proven to be
superior to one other and often multiple treatments are needed to
achieve the reattachment of the retina [5].
The optic disc pit is not always congenital, but can also be
acquired. This is thought to occur especially in patients with
glaucoma where lamina cribosa is altered as part of the glaucomatous
optic nerve damage, which then can lead to a focal formation of the
optic disc pit [6-9]. While this is not the most common presentation
for patients with glaucoma, there had been studies [10] that found a
higher prevalence of acquired optic disc pit in people with normaltension
glaucoma, and successful reversal of those pits with IOP
lowering drops [1,11,12]. In our case, we postulate that an increase in
the uveoscleral outflow from bimatoprost may have altered the tissue
remodeling through glial cell activation to facilitate the closure of
optic disc pit as well as the resolution of the subretinal and intraretinal
fluid.
Conclusion
investigation of both the optic nerve and the macula. In untreated
or poorly controlled glaucoma, progressive cupping of the optic nerve
head may lead to the development of an acquired optic disc pit, which
can produce maculopathy if untreated.
Patient Consent:
Consent to publish the case report was not obtained. This report
does not contain any personal information that could lead to the
identification of the patient.