Journal of Oral Biology
Download PDF
Research Article
Reproducibility of Manual Periodontal Probing Following a Comprehensive Standardization and Calibration Training Program
Bryan P. Fitzgerald1†, Charles E. Hawley1,2, Charles Q. Harrold3, J. Steven Garrett4, Alan M. Polson5 and Thomas E. Rams6
1Formerly Division of Periodontics, University of Maryland School
of Dentistry, Baltimore, Maryland, USA
2Department of Periodontology, Tufts University School of Dental
Medicine, Boston, Massachusetts, USA
3Formerly Department of Surgical Sciences, University of Colorado
School of Dental Medicine, Aurora, Colorado; presently retired,
Chandler, Arizona, USA
4Formerly Atrix Laboratories, Inc., Ft. Collins, Colorado, USA;
presently retired, Rigby, Idaho, USA
5Department of Periodontics, University of Pennsylvania School of
Dental Medicine, Philadelphia, Pennsylvania, USA
6Department of Periodontology and Oral Implantology, Temple
University School of Dentistry, Philadelphia, Pennsylvania, USA
†Deceased on November 20, 2018
*Address for Correspondence: Thomas E. Rams, Department of
Periodontology and Oral Implantology, Temple University School of Dentistry,
Philadelphia, Pennsylvania, USA; phone: (215) 707-2941/ fax: (215) 707-4223;
E-mail: trams@temple.edu
Submission: 12-May-2022
Accepted: 27-June-2022
Published: 29-June-2022
Copyright: © 2022 Fitzgerald BP, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Background: Clinical standardization and calibration training is
recommended to increase the reproducibility of periodontal probing, but
its impact on manual periodontal probing outcomes has received little
attention. This study examined the reproducibility of manual periodontal
probing performed by a periodontist after completion of a comprehensive
standardization and calibration training program.
Methods: A newly-educated periodontist was subjected to an
individualized periodontal probing standardization and calibration training
program involving approximately 24 total hours of lecture, bench-top, and
clinical instruction/evaluation. Satisfactory completion of each portion of
the training program required ≥ 95% intra-examiner agreement within
1 mm between initial and repeat measurements, and a ≥ 90% level of
exact agreement with measurements by a “gold standard” examiner. The
periodontist then evaluated bleeding on probing (BOP) and performed
duplicate measurements of probing depth (PD) and the distance between
the cementoenamel junction and gingival margin (CEJ-GM) with a manual
periodontal probe on 567 periodontal sites exhibiting ≥ 5 mm PD with BOP in
39 adults. Clinical periodontal attachment level (CAL) was calculated for each
site as (PD) - (CEJ-GM).
Results: Intra-examiner measurement error (the standard deviation for
a single measurement) was found to be 0.21 mm for PD, 0.15 mm for CEJGM,
and 0.26 mm for CAL. Replicate assessments of PD and CAL yielded
excellent exact agreement kappa scores of 0.86 and 0.87, respectively.
Greater intra-examiner measurement error was found at periodontal sites
with more gingival inflammation as measured by higher BOP index scores.
Conclusion: These findings demonstrate that a rigorous periodontal
probing standardization and calibration training program facilitates acquisition
of highly reproducible PD and CAL assessments in moderate to deep
inflamed periodontal pockets with a manual periodontal probe. Similar formal
hands-on training should be incorporated into dental education programs and
clinical research studies to improve the diagnostic performance of manual
periodontal probing of the periodontium.
Introduction
Periodontal probing provides the foundation for clinical
examination of the periodontium, helping determine periodontal
diagnosis and evaluate therapeutic outcomes in patients [1,2].
However, accurate and reproducible physical probing of the
periodontium is clinically challenging to carry out, increasing the
likelihood of probing measurement errors. Variability in clinical
examiner experience, probing force, degree of gingival tissue
inflammation, tooth root anatomy, probing depth, periodontal site
location, probe subgingival insertion angles, probe tip diameter, probe
millimeter markings, visual reading of probe markings, rounding off of probe measurements, patient cooperation, extent of subgingival
calculus, and transcription recording errors, may contribute to
periodontal probe measurement errors [1,3,4].
Diagnosis of periodontitis is dependent upon reliable periodontal
probing. Clinical periodontal attachment level (CAL) provides a
clinical approximation of connective tissue attachment to tooth root
surfaces [1]. Manual probing can identify the coronal extent of CAL
to within ≤ 0.55 mm of histologic findings [5], but underestimates
the total root surface area affected by CAL loss [6]. CAL may be
directly measured with a periodontal probe from the cementoenamel
junction of teeth [7], but is more frequently calculated from separate
measurements of probing depth (PD) and the distance between the
cementoenamel junction and gingival margin (CEJ-GM), with CAL
= (PD) - (CEJ-GM) [3].
CAL measurements are widely recognized as the “gold standard”
for identifying progressive periodontitis in patients [1]. Lindhe
et al. designated a ≥ 3 mm change in CAL to detect progressive
periodontitis sites in untreated patients [8]. This was based on the view
that CAL changes exceeding three times the standard deviation (SD)
of replicate CAL measurements with a manual periodontal probe,
which were previously reported to be 0.82 mm on severe periodontitis
patients [9], were unlikely to be due to examiner measurement error.
Improved manual probe reproducibility may enable use of a lower
CAL change threshold for detecting progressive periodontitis and
increase the diagnostic sensitivity of manual periodontal probes.
To increase the reproducibility of periodontal probing, formal
standardization and calibration training [10], also known as examiner alignment and assessment training [11], is recommended
to identify and minimize sources of clinical examiner variation in
probing assessments. Abbas et al. reported improved reproducibility
in PD assessments after clinicians viewed a video program on
standardization of periodontal probing procedures [12].
However, the effectiveness of more extensive and rigorous
hands-on training programs is not known. To address this issue,
the present study examined the reproducibility of periodontal
probing measurements attained by a newly-educated periodontist
following the completion of a comprehensive periodontal probing
standardization and calibration training program.
Materials & Methods
This study involved a secondary retrospective analysis of
periodontal probing reproducibility data from one study site
(University of Maryland School of Dentistry, Baltimore, Maryland,
USA) participating in a previous US Food and Drug Administration
(FDA)-approved phase-3 product evaluation of 10% doxycycline
hyclate in a biodegradable drug delivery system [13]. The
reproducibility data were obtained after the study patients provided
signed informed consent, consistent with the Helsinki Declaration
of 1975, as revised in 2013, and as approved by the human subjects
institutional review board at the University of Maryland at Baltimore.
The present data analysis was also approved by the Temple University
human subjects institutional review board.
Pre-Study Examiner Standardization and Calibration Training:
A newly-educated periodontist with no research experience
(author BPF) was the single periodontist examiner for the
periodontal probing reproducibility study. Because of his relative
clinical periodontal inexperience, no baseline reproducibility
assessments of his periodontal probing technique were made. Prior
to the start of the probing reproducibility study, he underwent
individualized pre-study periodontal probing standardization and
calibration training involving approximately 24 total hours of lecture,
bench-top exercises, clinical instruction, and evaluation [10,14].
An initial half-day didactic review of periodontal data collection
principles and procedures focused on use of consistent manual
probing forces, identification of interproximal tooth contact points,
proper periodontal probe alignment, rounding-up or down rules,
appropriate reference points, identification of CEJ and GM location,
PD measurement, CAL calculation, and scoring of BOP. Following
this, laboratory bench-top probing exercises with dentiform models
depicting various types of periodontitis lesions were completed
under supervision of two “gold standard” experienced periodontists
previously documented to possess a high level of inter-examiner
reliability with each other (authors CQH and AMP). Full-mouth
clinical inter- and intra-examiner probing exercises were then
conducted on four pre-study periodontitis patients with the “gold
standard” examiners at a location extramural (University of Colorado
School of Dental Medicine, Aurora, Colorado, USA) to the probing
reproducibility study site in Baltimore. A standard UNC-15 probe
(UNC #15, Hu-Friedy, Chicago, Illinois, USA) was used throughout
the calibration exercises. Subsequently, five additional pre-study
periodontitis patients at the probing reproducibility study site were
subjected to supervised full-mouth replicate periodontal probings, with a final inter- and intra-examiner probing calibration carried out
on two more pre-study periodontitis patients at the reproducibility
study site with a “gold standard” examiner (author CQH). All of the
11 pre-study periodontitis patients exhibited a similar range of PD,
CEJ-GM distance, and BOP as patients in the subsequent probing
reproducibility study. A ≥ 95% intra-examiner agreement within 1
mm between initial and repeat measurements, and a ≥ 90% level of
exact agreement with “gold standard” examiner measurements, was
required for satisfactory completion of each portion of the pre-study
examiner standardization and calibration training program.Patients
After completion of the pre-study standardization and calibration
training program, the periodontist examiner conducted periodontal
probing reproducibility examinations on 39 systemically-healthy
adults (20 male, 19 female; aged 32-65 years; mean age 47.8 ± 8.1
(SD) years), who presented with localized to generalized severe
periodontitis (equivalent to Stage III/Grade B periodontitis) [2],
where at least two dentition quadrants had at least four periodontal
sites exhibiting ≥ 5 mm PD with BOP, of which at least two of these
sites had PD ≥ 7 mm.
Patients were excluded if they had been treated with periodontal
root scaling within the prior two months.
Clinical Measurements:
Clinical measurements were assessed at six sites per tooth in each
study patient. PD was measured to the nearest whole millimeter from
the gingival margin to the most apical gingival tissue penetration
of the probe tip using a UNC-15 periodontal probe, with the probe
inserted with its long axis aligned parallel to the long axis of the
tooth (Figure 1A). Interproximal PD measurements were carried out
immediately adjacent to interproximal tooth contact points. If there
was no interproximal contact present, the periodontal sites were
excluded from analysis.
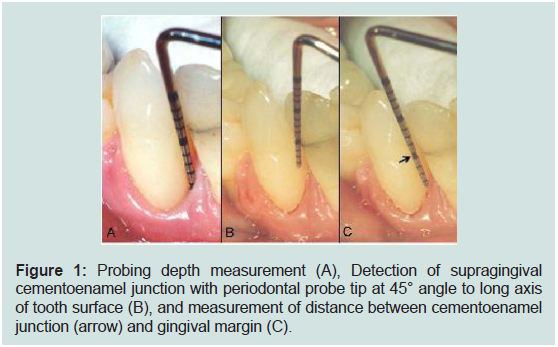
Figure 1: Probing depth measurement (A), Detection of supragingival
cementoenamel junction with periodontal probe tip at 45° angle to long axis
of tooth surface (B), and measurement of distance between cementoenamel
junction (arrow) and gingival margin (C).
BOP was scored on a 0-3 index scale after measurement of
PD. Bleeding at each periodontal site was graded as follows: 0 = no
bleeding; 1 = delayed single bleeding point, or a fine line of blood
(Figure 1B); 2 = interdental triangle becomes filled; 3 = immediate
profuse bleeding after probing [15].
The CEJ-GM distance was then determined by initially placing
the periodontal probe tip against the enamel surface coronal to the
margin of the gingiva at a 450 angle to the long axis of the tooth
(Figure 1B) [3]. When the CEJ was located subgingival to the gingival
margin, the probe tip was moved apically with minimal force into the
gingival sulcus while maintaining contact with the tooth surface. The
CEJ location was then detected by tactile sensation or by observation
of a change in the direction of the periodontal probe tip movement
during advancement from the tooth enamel to cementum. The probe
tip was moved in a coronal direction from the gingival margin if
the CEJ was located coronal to the gingival margin and difficult to
visually discern. The CEJ-GM distance was measured to the nearest
whole millimeter, with positive numbers recorded if the most coronal
aspect of the gingival tissue margin was located on enamel, and
negative values recorded when the most coronal aspect of the gingival
tissue margin was located apical to the CEJ on cementum (Figure 1C).
Only periodontal sites where the CEJ could be clinically located were
included in the present analysis, with exclusion of sites where the CEJ
was obscured by margins of dental restorations. CAL was calculated
from measurements of PD and CEJ-GM, with CAL = (PD) - (CEJGM)
[3].
Examination Procedures:
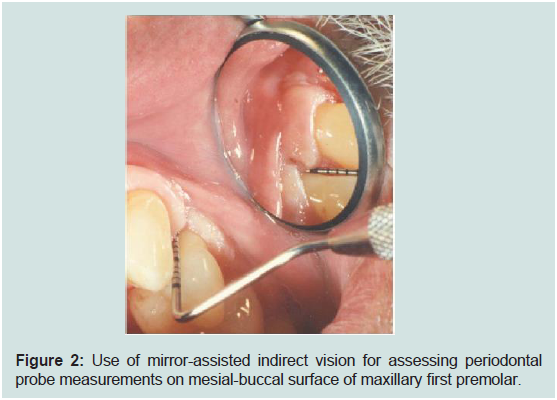
The clinical examinations were conducted by the trained and
calibrated periodontist examiner. Cotton roll isolation and air drying
were used to establish a dry field during the clinical examination
procedures, with measurement values verbally called out to a data
recording assistant for transcription. In order to standardize data
collection procedures at all periodontal sites irrespective of their
intraoral location, as required by the FDA-approved product
evaluation protocol, all clinical measurements at both facial and
lingual tooth surfaces were obtained using mirror-assisted indirect
vision (Figure 2). The clinical examination sequence on each study
patient started with a whole-mouth assessment of the Plaque Index
on all periodontal sites [16]. Then, using a UNC-15 probe, PD
measurements and scoring of the BOP index were carried out on the
maxillary right dentition quadrant. These values were evaluated by
the study site principal investigator (author CEH), independent of
the periodontist examiner, to identify periodontal sites exhibiting
a combination of PD ≥ 5 mm and BOP for probing reproducibility
assessments. The CEJ-GM distance was then measured on these
designated periodontal sites throughout the dentition quadrant. These same steps were then carried out in turn on the maxillary left,
mandibular left, and mandibular right dentition quadrants. After all
initial data collection was completed in all dentition quadrants, repeat
measurements of PD and CEJ-GM on the designated periodontal sites
in each dentition quadrant were performed, as specified by the study
center principal investigator through the data recording assistant.
Repeat assessments were initiated first in the maxillary right dentition
quadrant, followed in turn by the maxillary left, mandibular left, and
mandibular right dentition quadrants. Repeat measurements were
obtained at least 15 minutes after initial evaluations to reduce the
effect of examiner memory of initial recordings [10]. The periodontist
examiner was kept blinded to initial measurement values.
Figure 2: Use of mirror-assisted indirect vision for assessing periodontal
probe measurements on mesial-buccal surface of maxillary first premolar.
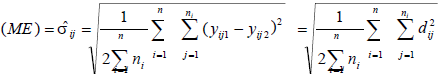
Data Analysis:
Data analysis was performed using a statistical computer software
package (Statistical Analysis System, SAS Institute, Inc., Cary, North
Carolina, USA). Mean values and the SD of differences between
initial and replicate periodontal site assessments were calculated for
PD, CEJ-GM distance, and CAL. Intra-examiner measurement error
(ME) for each of the probing assessments was estimated by calculating
the SD for a single measurement as follows [17]:Where each σij at a site level is estimable based on the difference
between replicate measurements dij (representing the difference
in replicate scores for the observed measurement, yij, for the jth
site within the ith patient; n = number of patients), and where one
assumes measurement errors are independent of patient and sitetype,
i.e., var (yijk) = σ2.
Kappa statistics were used to quantify intra-examiner agreement
beyond chance for site-based replicate assessments of PD and CAL
[18]. Exact kappa and a kappa value combining pairs of scores within
1 mm of each other were calculated for replicate assessments of PD
and CAL, as previously described [19,20], but without confidence
intervals adjusted for within-patient effects. Kappa values between
0.40 and 0.75 were considered to represent fair to good agreement,
with kappa > 0.75 indicating excellent agreement [18].
The influence of gingival inflammation on intra-examiner
reproducibility of PD, CEJ- GM distance, and CAL was evaluated by
comparing their reproducibility parameters across increasing BOP
index scores.
Patients in the lowest and highest quintile of patients ranked by
the total number of periodontal sites/patient subjected to replicate
evaluations were also compared relative to agreement attained within
1 mm for replicate PD, CEJ-GM distance, and CAL measurements.
Results
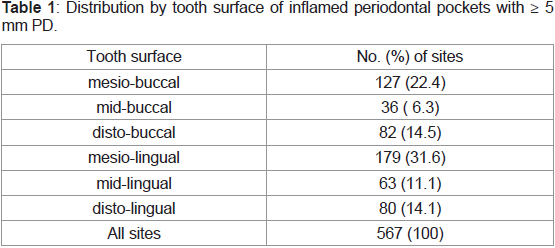
A total of 567 periodontal pockets demonstrating ≥ 5 mm PD and
BOP were evaluated in the probing reproducibility examinations, of
which 468 (82.5%) were located on interproximal tooth surfaces, with
each of the 39 study patients contributing 7-20 periodontal sites from
at least two dentition quadrants (Table 1). Among other sites in the
study patients not exhibiting ≥ 5 mm PD and BOP, 0.2% were ≥ 5 mm PD but without BOP, 70.7% were < 5 mm with BOP, and 29.1% were < 5 mm but without BOP.
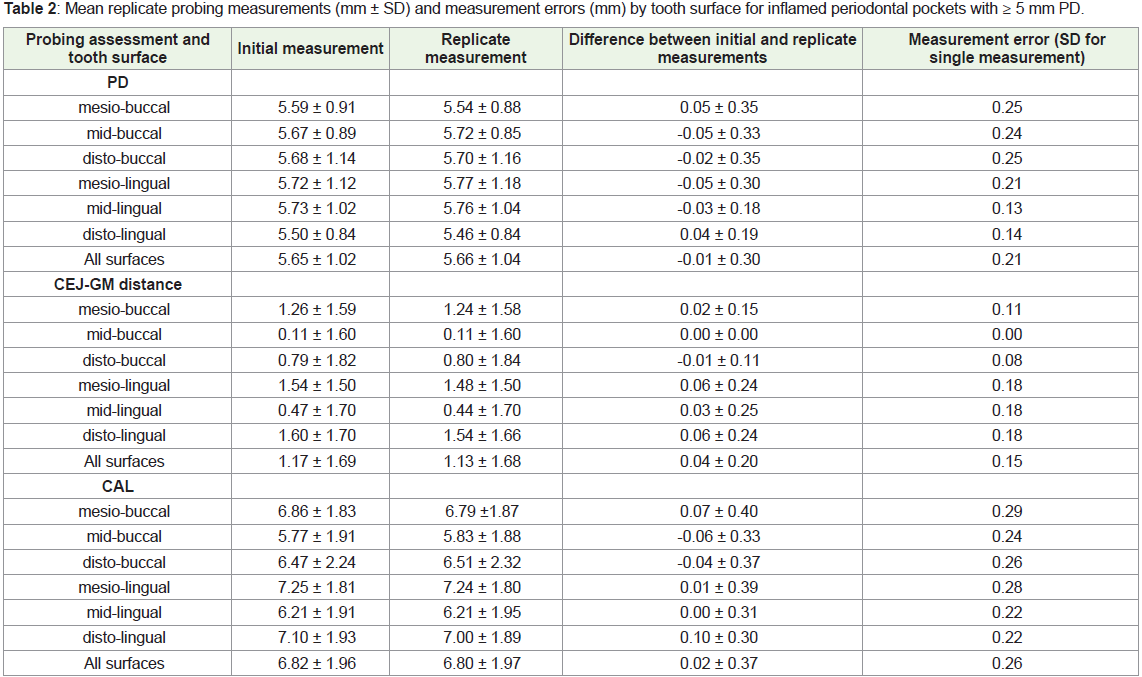
Table 2 presents the mean initial and replicate measurements
for PD, CEJ-GM distance, and CAL for the 567 periodontal pockets.
PD values averaged 5.7 mm (range 5-14 mm), with mean differences
among various tooth sites found to be ≤ 0.10 mm between replicate
values for PD, CEJ-GM distance, and CAL. The SD for single
measurements (intra-examiner measurement error) of PD, CEJ-GM
distance, and CAL was 0.21 mm, 0.15 mm and 0.26 mm, respectively
(Table 2).
Table 2: Mean replicate probing measurements (mm ± SD) and measurement errors (mm) by tooth surface for inflamed periodontal pockets with ≥ 5 mm PD.
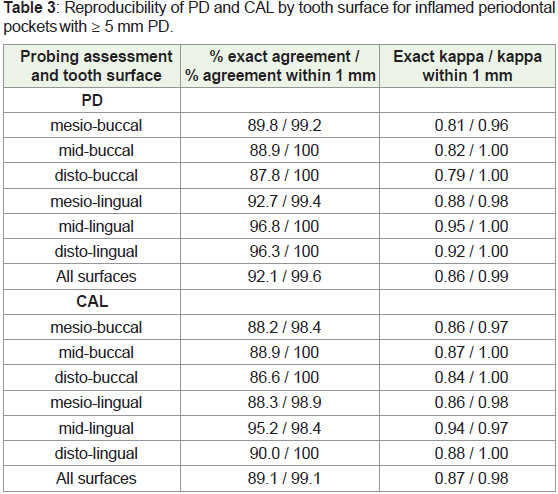
Table 3 reveals that exact agreement was found for 92.1%
of replicate PD measurements, and for 89.1% of replicate CAL
assessments, with both parameters attaining agreement within 1 mm
for more than 99% of examined periodontal sites. Kappa values for
exact intra-examiner agreement were 0.86 for PD (0.99 for agreement
within 1 mm), and 0.87 for CAL (0.98 for agreement within 1 mm).
These kappa values all exceeded the threshold required (kappa > 0.75)
to indicate excellent intra-examiner agreement [18].
Table 3: Reproducibility of PD and CAL by tooth surface for inflamed periodontal
pockets with ≥ 5 mm PD.
Among specific tooth surfaces, lingual surfaces generally yielded
lower intra-examiner measurement error values and higher kappa
scores, as compared to buccal tooth surfaces for both PD and CAL
(Table 2,3).
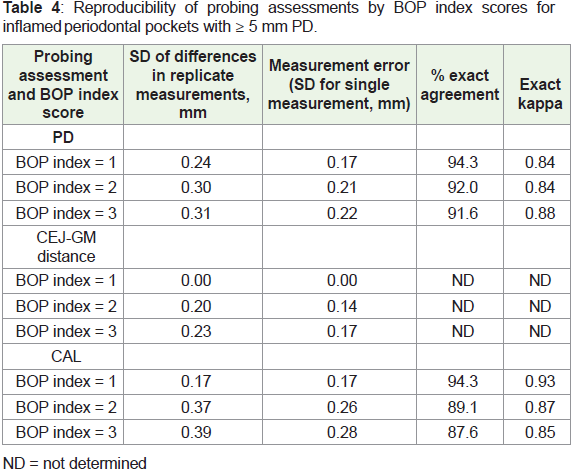
Table 4 shows the influence of BOP index scores on the
reproducibility of PD, CEJ-GM distance, and CAL assessments.
Higher BOP index scores were associated with greater intra-examiner
measurement error for all of the probing evaluations carried out, and
decreased kappa values for CAL (Table 4).
Table 4: Reproducibility of probing assessments by BOP index scores for
inflamed p eriodontal pockets with ≥ 5 mm PD.
All PD and CEJ-GM replicate measurements, and all but two
CAL replicate measurements (one in each patient group), were within
1 mm of each other in patients where only a few periodontal sites
were subjected to replicate evaluations (lowest quintile; 7-12 sites
per patient; 89 total sites in 8 patients), as well as in patients where
a higher number of periodontal sites were scored twice (highest
quintile; 18-20 sites per patient; 155 total sites in 8 patients).
Discussion
The present study findings demonstrate that a manual periodontal
probe visually read to the nearest whole millimeter may provide
highly reproducible PD and CAL measurements on moderate to
deep inflamed periodontal pockets when employed by a rigorously
trained and calibrated periodontist. These findings agree with and
extend previous studies of manual probes [9,20-24], where most
replicate CAL measurements were made on periodontal sites with
shallow to moderate probing depths, and variable levels of gingival
health and inflammation. In contrast, the present study evaluated
only moderate to deep (5-14 mm) periodontal pockets with BOP,
which are clinically more challenging to physically probe and subject
to greater periodontal probe variation.
A remarkably low SD for a single CAL assessment of 0.26 mm
(intra-examiner error) was attained in the present study. This
value is strikingly better than the SD of single CAL assessments, as
calculated by Yang et al. [25], that range from 0.54 mm to 0.69 mm
for manual periodontal probes [9,22,26,27], and similar to values of
0.20 mm to 0.31 mm found for a controlled-force probe used with an
acrylic occlusal reference stent [25,28]. However, a controlled-force
periodontal probe with automated CEJ detection was reported to
provide a lower intra-examiner error of approximately 0.12 mm [29].
Several reasons may account for the markedly better CAL
reproducibility achieved in the present study as compared to previous
investigations of manual periodontal probes [9,3,20-24,26,27]. Only
a single periodontist performed replicate CAL assessments in the
present study, in contrast to Haffajee et al. where three different
examiners were used [9]. Evaluations in the present study were
under ideal clinical examination conditions, as compared to a replication study conducted outdoors with portable dental chairs
and no compressed air or suction [20]. An extensive and welldefined
pre-study standardization and calibration training program
was completed by the periodontist in the present study, whereas
most previous studies did not conduct or failed to report details of
any examiner training and calibration exercises. The periodontist in
the present study may also have been particularly gifted with regard
to the patience and temperament needed to carry out accurate and
reproducible replicate probing, and an ability to apply a uniform
probing force at standardized probe insertion angles, properly
identify the CEJ on subgingival tooth surfaces, and accurately read
probe markings.
It is additionally possible that the periodontist recalled initial
measurement values when performing replicate evaluations,
particularly in patients where a small number of periodontal sites
were examined twice. However, the standardized examination
protocol, where assessments of other parts of the dentition and at least
15 minutes transpired between replicate site measurements, helped
mitigate against this possibility. The high probe reproducibility
found in patients with many sites scored twice (highest quintile of
sites/patient; where examiner recall is less likely), was similar to
patients where replicate evaluations were performed on only a few
sites (lowest quintile of sites/patient; where examiner recall is more
likely), suggesting that examiner performance in the present study
was not predominately due to recall bias. However, it remains to be
established if other dental professionals can attain and maintain over
time similar levels of probing reproducibility when exposed to the
standardization and calibration training program employed in the
present study. If so, then longitudinal monitoring of CAL in clinical
practice and periodontal research studies may be reliably performed
with a manual probe, instead of a controlled-force probe with an
acrylic occlusal reference stent, since comparable levels of intraexaminer
error are found between them (0.26 mm with manual probe
in this study versus 0.20-0.31 mm previously reported with controlled force
probe [25,28]). Better periodontal probe reproducibility may
also help reduce sample sizes needed in clinical research studies to
identify statistically significant differences between outcome variables
scored with a manual probe [30].
Importantly, the excellent probe reproducibility attained by the
periodontist in the study patients corresponded as well or better with
reproducibility levels achieved in the pre-study standardization and
calibration training program. This supports the concept that examiner
performance attained during standardization and calibration training
is a critical determinant of a clinician’s subsequent reliability in
making accurate and consistent periodontal measurements in clinical
practice settings and research studies.
Of the clinical components used to calculate CAL, there was
less intra-examiner error for a single measurement of the CEJ-GM
distance (0.15 mm) than for PD (0.21 mm), even though the CEJ
may be difficult to locate in subgingival and interproximal locations
[1,3,26]. However, CEJ-GM distance measurements are generally
smaller values possessing less potential variability than usually larger
PD measurements, and are not influenced by gingival inflammation
in adjacent soft tissues. In contrast, PD values show more variability
as a result of varying periodontal probe tip penetration into inflamed
gingival connective tissues subjacent to the junctional epithelium [31,32]. The present study findings that PD and CAL measurements
on moderate to deep periodontal pockets are less reproducible
with higher BOP index scores (reflecting greater levels of gingival
inflammation) are consistent with these histologic observations
[31,32].
The increased degree of reproducibility in PD and CAL
measurements on lingual as compared to buccal tooth surfaces
in the present study (Tables 2 and 3) is likely related to unique
methodological procedures required by the FDA-sanctioned
phase-3 clinical product evaluation protocol, where measurements
were made using mirror-assisted indirect vision on both buccal
and lingual tooth surfaces, an approach not otherwise employed in
clinical practice. This unusual clinical examination approach posed
technical performance difficulties for the periodontist examiner on
buccal tooth surfaces, particularly mesio-buccal sites. In comparison,
greater reproducibility in PD and CAL measurements is reported for
buccal tooth sites in previous studies [20,22,23], where examiners
employed direct visualization for buccal tooth surfaces and mirrorassisted
indirect vision for lingual surfaces, which likely enhanced
and hindered probe readings, respectively.
Conclusion
A newly-educated periodontist, after completing a rigorous
periodontal probing standardization and calibration training
program, was able to obtain highly reproducible PD and CAL
assessments in moderate to deep inflamed periodontal pockets using
a manual periodontal probe. Similar formal hands-on training should
be incorporated to a greater extent into dental education programs
and clinical research studies to improve the diagnostic performance
of manual periodontal probing of the periodontium.
Acknowledgement
All authors declare that they have no conflicts of interest relative
to this study. Dr. Bryan P. Fitzgerald died during preparation of this
article, but was instrumental in contributing to the design of the study,
methods used, acquisition of the study data, writing and revising
the initial draft and its intellectual content, and serving as primary
author/presenter of a research abstract on the study findings. Support
for this research was provided by intramural funds from the National
Institute of Dental and Craniofacial Research, National Institutes of
Health, Bethesda, Maryland, USA, and by Atrix Laboratories, Inc.,
formerly in Ft. Collins, Colorado, USA.