Journal of Oral Biology
Download PDF
Research Article
Simulation of Soft Tissue in 3D-Printed Models for Guided Bone Regeneration Education
Wangsrimongkol Buddhapoom, Reis Natacha, Fernández-Guallart Ines,Yu Yung Cheng Paul*
Arthur Ashman Department of Periodontology and Implant Dentistry, New York University, USA
*Address for Correspondence: Cheng Yu PY, Department of Periodontology and Implant Dentistry, New York University, Clinic 5W, 345 E 24th St, New York, NY 10010, New York, USA, Tel: +1-3472792958; E-mail: ycy233@nyu.edu
Submission: 16-April-2020
Accepted: 06-June-2020
Published: 09-June-2020
Copyright: © 2020 Wangsrimongkol B, et al. This is an open access
article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
Abstract
The use of custom-made 3D-printed models extracted from the Cone
Beam Computed Tomography (CBCT) of the patient provides the dentist
with the opportunity to rehearse a surgical procedure such as implant
placement enhancing its tactile simulation in order to achieve a predictable
and successful surgical outcome. Even the fact that these models have
substantially improved the preparation and education in implant surgery,
they lack the soft tissue layers necessary for simulating important procedures
such as periosteal releasing incisions and flap primary closure. For a more
realistic surgical simulation in implant education, the soft tissue layers of the
mucoperiosteal flap have been incorporated into the existent 3D-printed
model. The purpose of this report is to represent, describe, document and
discuss the recreation of the soft tissue layers of the mucoperiosteal flap on
a custom-made 3D-printed model extracted from the CBCT of the patient
in a case used to simulate a guided bone regeneration (GBR) procedure.
Introduction
Implant dentistry is one of the most popular modalities in the
dental field due to the high predictability and success rates of implants
when compared to conventional treatment options to replace missing
teeth in complete or partially edentulous patients [1-3].
In the last few years, new methods of diagnosis, treatment
planning and execution techniques in dentistry have been developed
or improved due to the advances in technology. Examples of this are
the evolution of digital dental imaging from two-dimensional (2D)
to three-dimensional (3D) images, the creation of digital dental
impressions (intraoral scans), digital treatment planning (virtual
software), digital guidance for surgery (computer-guided surgery)
and digital 3D production (Computer-Aided Design/Computer-
Aided Manufacturing - CAD/CAM). Also, the recent advances in
digital imaging such as Cone Beam Computed Tomography (CBCT)
are improving the visualization, now with great details of the patient’s
anatomy in 3D when compared with standard radiographs, which are
taken and seen in 2D [3].
As implant dentistry is becoming more widely practiced, effective
continuous education is becoming very important, especially
regarding the fact that implant dentistry as a main subject is usually
not taught in undergraduate courses of dental schools, so clinicians
who are going to practice it find the need for learning it afterwards
either in postgraduate programs, advanced education training or
weekend courses, among others. Mainly, this education is based on
pre-clinical hands-on practice followed or not by clinical training. To
design and perform a hands-on, several materials and methods can
be used (typodonts, models from the mouth, animal jaws and human
cadavers, among others). From these, the use of 3D-printed models extracted from patient’s CBCT is becoming a well-accepted method
of education because it allows to accurately simulate the real patient
anatomy, especially in terms of hard tissues (teeth and bone), so
procedures such as implant placement can be successfully practiced
on them. However, the simulation of a complete implant surgical
procedure with all its steps (incisions design, flap elevation, osteotomy,
implant placement and suture, and in some cases, additional guided
bone/tissue regeneration and/or sinus augmentation) is not possible
in CBCT-based 3D-printed model hands-on due to a lack of soft
tissues in these models, which management is of vital importance to
achieve clinical success [4,5].
Although the use of 3D-printed models is already established
worldwide for surgical simulation in terms of education in implant
dentistry, there is still shortage in publications regarding the best
material for fabrication of soft tissues for these models. Park et al.
(2017) reported the combination of vinyl tape, sponge tape and liquid
tape to mimic the soft tissue in a 3D-printed model. However, there
is a limitation in terms of the amount of periosteal releasing and
consequential flap advancement that can be achieved in this option,
which is only 1-2 mm. In the new prototype presented in this article
it was possible to gain 5-10 mm (similar to what can be achieved in
a real patient), which is crucial for the achievement of tension-free
primary closure [6].
The purpose of this report is to represent, describe, document and
discuss the recreation of the soft tissue layers of the mucoperiosteal
flap on a custom-made 3D-printed model extracted from the Cone
Beam Computed Tomography (CBCT) of the patient in a case used to
simulate a guided bone regeneration (GBR) procedure.
Materials and Methods
The steps for producing a 3D-printed model and simulating a
surgical guided bone regeneration procedure on it are
1. Obtain a patient’s CBCT scan using a CBCT imaging
system (J. Morita, Kyoto, Japan), in which the field of view (FOV)
of the image will be selected depending on the area of interest of the
case.
2. Convert the Digital Imaging and Communications Stereolithography (STL, OsiriX Lite, Geneva, Switzerland) format.
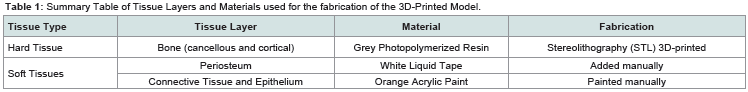
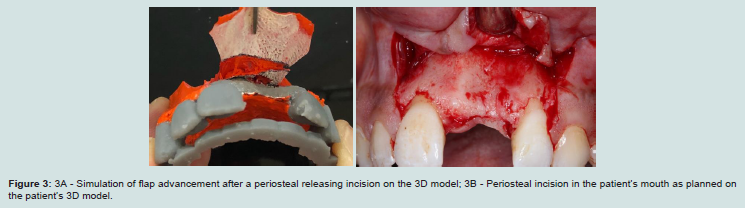
Table 1: Summary Table of Tissue Layers and Materials used for the fabrication of the 3D-Printed Model.
3. Process and print the STL file with a 3D- printer (Formlab
Form 2 Printer, Somerville, Massachusetts, USA), using a grey
methacrylic photoreactive liquid resin material that represents the
hard tissue of the 3D-printed model.
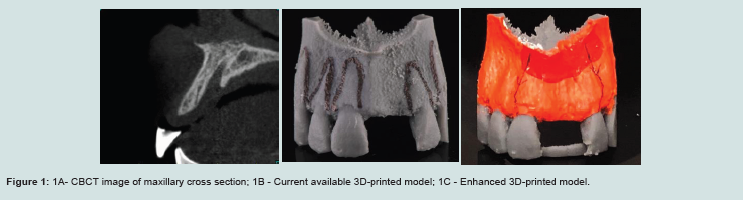
4. Add acrylic paint to simulate soft tissue layers: periosteum
is recreated with liquid tape and connective tissue and epithelium
are reconstructed with orange acrylic paint, painted manually on the
surface of the 3D-printed model (Table 1).
5. A full-thickness midcrestal incision is made between the
teeth adjacent to the defect. Two vertical incisions are made parallel
or trapezoidal until the base of the flap, widening apically for easy
coronal repositioning of the flap after augmentation with the graft
material. After passing the imaginary mucogingival junction, the
vertical incisions continue apically in a vertical or more convergent
direction.
6. The liquid tape with orange acrylic paint is then elevated
with a periosteum elevator.
7. Cortical perforation (decortication) is performed by #1 or
#2 round bur using high speed hand piece with copious irrigation.
8. Releasing incisions are made with a sharp 15C blade on
the inner apical portion of the liquid tape and orange acrylic paint,
creating a 2-3mm split-thickness dissection.
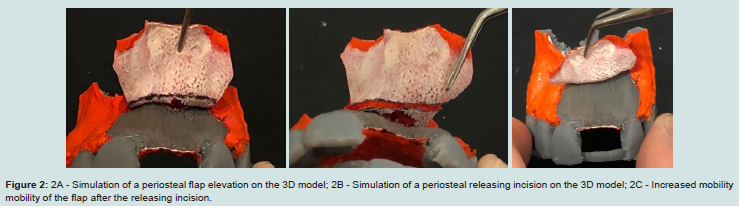
9. Tinfoil is used as a template, and in this case also as a mimic
of the collagen membrane, fitted and trimmed to the ideal shape, and
then put to the correct position. A single tack is positioned apically
through the membrane into the photopolymerized resin, and the
membrane is rotated 180 around the tack and adjusted to extend
2-3mm beyond the augmented area. The graft material is placed and
condensed to fill the defect.
10. Stabilization of the membrane and the underlying graft
material is achieved by using horizontal mattress sutures extending from the apical portion of the liquid tape to the palatal aspect of the
orange acrylic paint. Consequently, the liquid tape is then coronally
advanced together with the orange acrylic paint, allowing tensionfree
closure afterwards.
Finally, the complete adaption of the orange acrylic paint is
achieved by multiple interrupted 4-0 chromic gut sutures.
In this case, the area of interest was the anterior maxilla, an
aesthetic area where soft tissue management is usually necessary.
Figure 1A shows the patient CBCT, where it is possible to appreciate
the selected area for the guided bone regeneration (GBR) surgical
simulation. The DICOM file was processed and the STL file was
printed obtaining the patient 3D-model using a grey methacrylic
photoreactive liquid resin material to mimic the hard tissue of the
patient, as it is shown in Figure 1B. After the 3D- model was printed,
the soft tissue layers needed for simulation of soft tissue management
during GBR were fabricated using acrylic paint and white liquid tape.
In this specific prototype, orange acrylic paint was used to reproduce
the epithelium and connective tissue and liquid tape to reproduce the
periosteum, as shown in Figure 1C (the white layer was the first one
to be painted on the 3D model, and the orange layer was painted over
it [Figure 2A]). In Table 1, the description of 3D model layers can be
appreciated.
Results
In the present case report, the surgical procedure of GBR
technique was performed successfully after the dentist did simulation
and practised the surgery sequence in the enhanced 3D model.
Figure 1B shows the hard tissues 3D model. Figure 1C shows
the soft tissues 3D-printed model with the incisions design. Figure 2A shows flap elevation after midcrestal, mesial and distal incisions. Figure 2B shows the periosteum releasing for flap advancement. Figure 2C shows the increased mobility of the flap to achieve tensionfree primary closure. Figure 3A shows the occlusal view of the
advancement of the flap in the 3D model, similar to the one achieved in the patient’s mouth (Figure 3B).
Figure 1: 1A- CBCT image of maxillary cross section; 1B - Current available 3D-printed model; 1C - Enhanced 3D-printed model.
Figure 2: 2A - Simulation of a periosteal flap elevation on the 3D model; 2B - Simulation of a periosteal releasing incision on the 3D model; 2C - Increased mobility mobility of the flap after the releasing incision.
Discussion
Nowadays, with the advances in technology, 3D imaging
techniques are replacing 2D imaging techniques, especially in
complex cases due to the need for better details of anatomy. CBCT
scan is a 3D digital imaging technique that uses ionizing radiation
(x-ray), although when compared with conventional CT scan it
is less invasive in radiation exposure and has higher quality. The
principle of the CBCT image is that higher density of the tissue
equals to higher absorption of the radiation, so the performance in
hard tissue imaging is higher than in soft tissue. CBCT is becoming
more popular in implant dentistry due to the accurate visualization
of hard tissues needed for implant treatment planning and moreover
the possibility of virtual simulation of the implant position in relation
to neighboring structures when introducing the CBCT data into
a planning software. Magnetic Resonance Imaging (MRI) is a 3D
digital imaging technique using non-ionizing radiation, which basic
principle is the interaction between static magnetism and hydrogen
atoms. Consequently, the higher amount of hydrogen atoms in the
tissues, the higher density. Higher quantity of hydrogen atoms is
found in tissues with higher quantity of water, so the performance
in soft tissue imaging is higher than in hard tissues. In comparison
with CBCT, the imaging resolution of hard tissue is lesser, and it is
also more expensive [7-9]. Both hard and soft tissue information
are essential to produce a 3D-printed model. However, CBCT scan
is preferable to MRI because without a highly precise hard tissue
information from the real patient it is not possible to fabricate an
actual 3D-printed model for surgery simulation.
Implant placement is a very straightforward surgical procedure in cases having enough bone width and height as well as healthy
soft tissue. However, in more complex cases there is a need for
reconstructing bony and soft tissue defects. TThere are several
techniques for bone augmentation such as guided bone regeneration
(GBR) with the use of membranes in combination to autogenous
bone grafts, allografts and/or xenografts. To enhance its results bone
promoting proteins (BPPs), or platelet rich plasma (PRP) can be
used. Other techniques include inlay and onlay grafts, ridge splinting,
and distraction osteogenesis among others. On the other hand, for
soft tissue augmentation, there are also numerous techniques such
as autogenous grafts (free gingival, connective tissue grafts), or the
use of allogenic, xenogenic and synthetic materials. In all of these
techniques, soft tissue management is needed in terms of incision
making, flap elevation and suturing [10,11].
Soft tissue management is important for a proper healing of the
bone and soft tissue. Flap design with correct incisions is important
for bony defect access, sustainability of the blood supply from the
base of the flap, papillae preservation and free-tension primary
closure allowance among others. After elevating a full-thickness
mucoperiosteal flap, especially in cases of ridge augmentation, it is
imperative to either stretch the elastic fibers present in the mucosa,
or do a horizontal periosteal releasing incision in the apical part of
the flap to increase the stretchability of the tissue in order to allow
it to be advanced and cover all the surgical site, thus achieving the
so-called tension-free primary closure. Primary closure should be
tension-free in order to avoid pressure on the graft materials which
can cause postoperative swelling, as well as to allow microvascular
anastomosis for re-epithelization and fully wound closing, enhancing
the re-establishment of the blood supply [12-14].
Conclusion
The use of 3D-printed models from CBCT images had several
advantages in surgical simulation and training in the past in
comparison to standard models and other hands-on modalities.
CBCT scans are more favorable than MRI in terms of achieving
hard tissues visualization in 3D and transferring it to a 3D model.
However, the recent challenge is the addition of soft tissues into the
3D models. This new issue is required due to the importance of soft
tissue management in many procedures in implant dentistry, and thus
a proper 3D model prototype should simulate the soft tissue layers:
periosteum, connective tissue and epithelium. This new 3D model
prototype provides an excellent hands-on for educational purposes,
as it allows the practitioner to study, simulate and rehearse several
times the soft tissue management procedure until he/she the reaches
the expected level of confidence, since multiple replicas of soft tissues
layers can be fabricated. In the next coming years, with the integration
of MRI into CBCT, the production of even more realistic soft tissue
architecture for surgical simulation seems possible. However, despite
the promising results of the proposed 3D enhanced model, further
investigations at a higher level of evidence are necessary to validate
this proposed 3D model.