Journal of Oral Biology
Download PDF
Review Article
Dental Care of Transgenders on Long- Termhormone Therapy
Geraldine Weinstein*
Division of General Dentistry, University of Connecticut School of Dental Medicine, USA
*Address for Correspondence: Geraldine Weinstein, Division of General Dentistry, 263 Farmington Ave, Suite LM031, Farmington, CT USA 06030-3811, USA, E-mail: gweinstein@uchc.edu
Submission: 21 May, 2019;
Accepted: 12 June, 2019;
Published: 14 June, 2019
Copyright: © 2019 Weinstein G, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Recent studies in the United States have noted that there are over
a million individuals who identify as transgenders and have begun the
process of hormone therapy. Such therapy regiments allow the individual
to transform from the birth gender to the desired gender. The time frame
of the hormone therapy extends over a lifetime and can have some health
consequences for the individual. It is therefore paramount to the dentist’s
understanding what the health risks of a transgender on hormonal therapy
can be in order to make appropriate decisions in these patients’s dental
treatment.
Introduction
In the Hippocratic Oath at Dental School Graduation, we swear
to “first do no harm” to our patients. It follows that we shall not
discriminate regardless of race, sex or gender. It is incumbent upon
us to continuously learn about our patients so that we shall always
treat them safely and provide them with compassionate care. In
the Lesbian, Gay, Bisexual & Transgender (LGBT) community, the
Transgenders are perhaps the group that requires significant review
of their medical history when they present for dental treatment. In
the event of hormone therapy in transgender individuals, there are a
number of issues that require consideration.
1.4 million people in the United States identify themselves as
Transgender in a study done in 2016. It is noted in the literature that
a large number of these individuals experience discrimination that
lead to barriers for access to healthcare [1]. By definition, transgender
is defined as an individual who identifies with the opposite sex
to which they were assigned at birth. A transgender male (also
known as transmen, female to male or FTM) is an individual who
is assigned to the female sex at birth but desires to be identified as
a male. A transgender female (also known as transwoman, male
to female or MTF) is an individual who is assigned the male sex at
birth but desires to be identified as a female. Over the past decades,
some of these individuals have taken over the counter hormones to
transform themselves to the opposite sex [2]. In more recent years, safely monitored hormone therapies are utilized by physicians to
assist transgenders, clinical guidelines have been established by the
Endocrine Society. Some transgender individuals will complete
the transformation with sex reassignment surgery which would be
completed in multiple steps [3].
The American Psychiatry Association has ruled that individuals
who identify as transgenders do not have a pathologic illness! This
misunderstood population often experiences discrimination on many
levels [4]. This may lead them to unemployment and subsequently
no healthcare insurance. Additionally, education of health care
professionals regarding the care of transgenders is minimal [5]. This
is especially true in today’s dental schools. While local laws do not
always protect transgenders from discrimination [6,7], it is incumbent
upon us as dentists to learn more about this group of human beings in
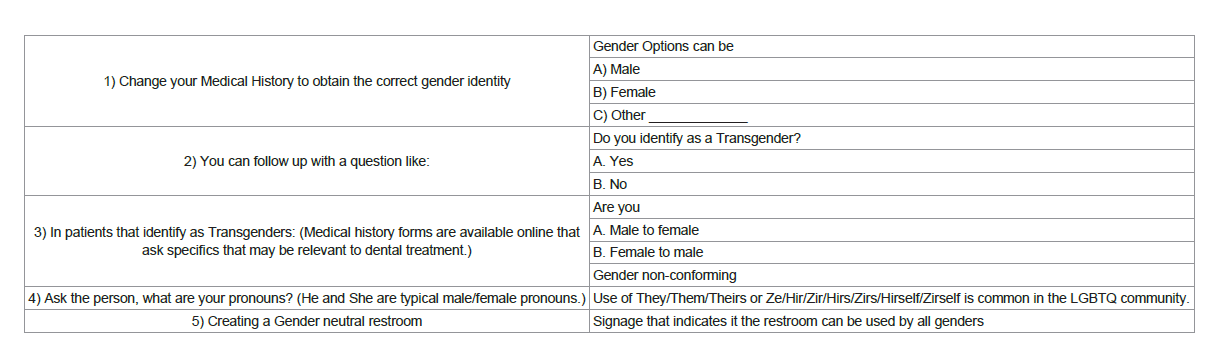
order to be a part of the solution not the problem (Table 1) [8].
Hormone Therapy in Male to Female (Transgender female)
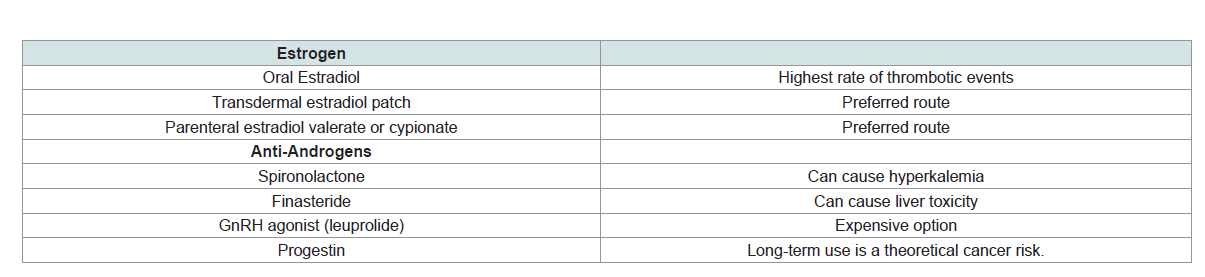
Transgender females undergo hormone therapy utilizing a
combination of exogenous estrogen and anti-androgen therapy. The
combination will stimulate a decrease in male pattern hair growth,
change body fat distribution and induce breast tissue formation.
In addition, the hormone combination will decrease testicular size
and erectile function. There is an interval of 18-24 months of time
on hormone therapy for transgender females to experience the maximum amount of change [9]. While the literature reports that
hormone therapy is safe when monitored closely, long-term use may
pose certain risks. In the transgender female, venous thrombosis is a
concern that may be related to estrogen hormone therapy, specifically
ethinyl estradiol which is recommended not to be used in transgender
care [10]. In the 2012 study by Wierckx et al. transgender females
on estrogen hormones for 11+ years had a 6% incidence of venous
thromboembolism (VTE) [11]. Routes of administration of estrogens
include oral, transdermal and parental (subcutaneous, intramuscular).
Formulations of estrogen via transdermal patch or parenteral route
are preferred to decrease the risk of thrombotic events [9,12].
In studies by Wierckx et al. (2013) transgender adults on hormone
therapy have exhibited increased incidence of type 2 diabetes [13].
Similarly, Gooren et al. (2008), noted fasting insulin in transgender
women to be elevated [14]. In the largest reported cohort study of
Transgenders, Nota et al. followed transwomen on estrogen (non
ethinylestradiol) and anti- androgens for an average of twenty two
years. Transwomen compared to men and women who are not on
hormone replacement have a higher incidence of stroke, myocardial
infarction and venous thromboembolism (Table 2) [19].
Hormone Therapy in Female to Male (Transgender Male)
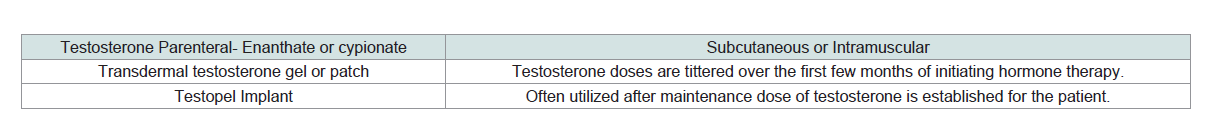
Transgender males undergo testosterone regimens to transition
from female sex assigned at birth to male. Testosterone replacement
therapy will allow for lowering of the voice, male pattern hair
growth, atrophy of the ovaries and muscle and fat redistribution and
clitoral enlargement [10]. Some undesirable effects that have been
observed have been increased systolic blood pressure, decreased HDL
cholesterol and increased triglycerides [20]. In a study by Nota et al.
1358 transgender men have been observed to have increased risk of
Myocardial Infarction compared to women who are not on hormone
therapy [19]. It is assumed that this is a result of the effect of hormone therapy on cardiovascular risk factors. Confounding factors such as
smoking and psychosocial stressors were not included in the study.
The transgender male has been found in general to have increased
incidence for type 2 diabetes [13]. The mechanism of the effect of
hormone replacement on glycemic control and/or insulin resistance
is not fully understood in the transgender population.
A baseline bone mineral density is recommended in Transgender
men on testosterone [21]. Osteoporosis screening is the standard of
care in transgender men ten years after initiation of hormone therapy
[21]. The levels of estrogen in transgender men are lower than female
controls which leads to Osteopenia [11]. In transmen that are noncompliant
with their estrogen therapy, a decrease in bone mass was
noted (Table 3) [22].
Summary: Dental Implications for Transgender Care
As in patients with underlying medical conditions, the transgender
patient should have regular follow up with the physician and be in
good metabolic control [23]. The physician should monitor hormonal
levels, check complete blood counts, liver function test, lipid panel
and hemoglobin HbA1C on a regular basis. In patients that have a
predisposition to thrombosis (including those that have had a history
of thrombosis), these patients may be on an anticoagulant [15]. In
such patients, it may be prudent to have a conversation with the
patient’s physician when planning surgical or invasive dental work
especially if the patient is on multiple antithrombotic/antiplatelet
medications [16]. Transgender patients that smoke and/or have
hypertension are at increased rate of thrombosis [1324].
Screening for diabetes is essential in high risk patients like
transgenders. For years the existence of periodontal disease has been
known to have a direct relationship with Diabetes [17]. Severity of
Chronic Periodontal disease complicates metabolic control and
ultimately Diabetes Mellitus [18]. The ability of the patient to heal
may be compromised after procedures involving the soft tissues and
extensive oral surgery. For example, implant placement in a poorly
controlled diabetic has been shown to have a higher rate of failure
[25]. In patients that have already been diagnosed with Diabetes,
monitoring of their Hemoglobin A1c to levels below 7.0 % is essential
prior to invasive dental procedures [26]. In patients that smoke and
have Diabetes, the risk for severe chronic periodontitis is greater.
Smoking cessation counseling should be enforced.
In some transgender individuals, unusual sexual practices and
behavior may put them at high risk for sexually transmitted disease
[12]. Careful examination of the oral cavity is essential to screen for
signs and symptoms of sexually transmitted disease [16]. A number
of these lesions may be viral like Herpes Simplex Virus 1 & 2 or
Human Papilloma Virus (HPV) [27]. In adolescents to young adults,
discussion of the HPV vaccine is essential as it has shown efficacy
in preventing oral and pharyngeal cancers caused by HPV [28]. In
patients that have been diagnosed with HIV/AIDS, opportunistic
infections can manifest in the oral cavity. In such cases, systemic
treatment should be coordinated with the patient’s physician [29].
The number or transgender individuals in the United States
may continue its upward trend in the future. Dentists in all types
of practices should be prepared to do due diligence by asking the
questions and get a clear understanding of the transgender patient’s
medical history. Such clarity will allow us to provide safe and timely
dental treatment to patients who have experienced many of life’s
battles.
Acknowledgement
“The author would like to acknowledge Dr. Efthimia Ioannidou for
her support and guidance on preparing this manuscript”.
References
18. Mealey BL (2006) Periodontal disease and diabetes: A two way street. J Am
Dent Assoc 137: S26-S31.