Journal of Oral Biology
Download PDF
Case Report
A Case Report of Resin Facing Implant Restoration in Maxillary Anterior Incisor
Hengjeerajaras P*, Kim KB, Mandali B, Hu G, Huang JT, Guallart IF, Al Khalil R and Ashman A
Department of Periodontology and Implant Dentistry, New York
University College of Dentistry, USA
*Address for Correspondence: Hengjeerajaras P, Department of Periodontology and Implant Dentistry, New York University College of Dentistry, USA
Submission: 14 April, 2019
Accepted: 11 May, 2019
Published: 15 May, 2019
Copyright: © 2019 Hengjeerajaras P, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Implant restorations may be challenging when attempting to satisfy
patients even with the recent advances in materials and techniques. In
this case report, the patient had fractured implant at the #8 site that was
removed and healed for 3 months. This resulted in a class II Siebert bone
defect. The patient followed the treatment suggested by the dentist
and achieved soft tissue esthetics but decided to choose the restoration
according to his esthetic perceptions. This report shows that the esthetic
is subjective based on a patients desire. Objective esthetic evaluation is
supported by science and research. However, the final decision concerning
esthetics is determined according to a patient’s perception. For patient’s
satisfaction the clinician, most respect the patient’s decision.
Keywords
Asymmetrical central incisor; Esthetic perception; Patient oriented
restoration; Subjective perception
Introduction
Replacement of missing anterior teeth has always been a challenge
for clinicians due to high patient esthetic demands [1]. From a patient’s
point of view, extraction and replacement of an anterior tooth can be
a very psychological and emotional experience. In the past, the choice
of treatment was based for the most part on the clinician’s assessment
of function and esthetics [2]. Although a clinician’s evaluation criteria
may be backed by science and experience, with the proliferation of
dental treatment information based on social media, patients have
become more critical and selective of their own esthetic choices [3].
Therefore, the patient must always be part of decision planning to
determine a successful outcome of treatment [4]. Moreover the
outcome of treatment is often centered on patient’s satisfaction [5].
Consequently, the growing demand and awareness of esthetics have
led to increased patient involvement in treatment planning of cases.
Esthetic criteria are often influenced by a patient’s sex, age, culture,
expectation and psychological factors [3]. This report presents a case
in which surgical and prosthetic decisions were, in large part, based
on the patient’s desires and input.
Material and Methods
The clinical data in this study was obtained from Implant Database
(ID). This data was extracted as de-identified information from the
routine treatment of patients at the Ashman Department of Period
ontology and Implant Dentistry at the New York University College of
Dentistry (NYUCD) Kriser Dental Center. The ID was certified by the
Office of Quality Assurance at NYUCD. This study is in compliance
with the Health Insurance Portability and Accountability Act
(HIPAA) requirements and approved by the University Committee
on Activities involving Human Subjects.
A 69 years old African American man was referred for #8
fractured implant to New York University College of Dentistry
Ashman Department of Period ontology and Implant Dentistry.
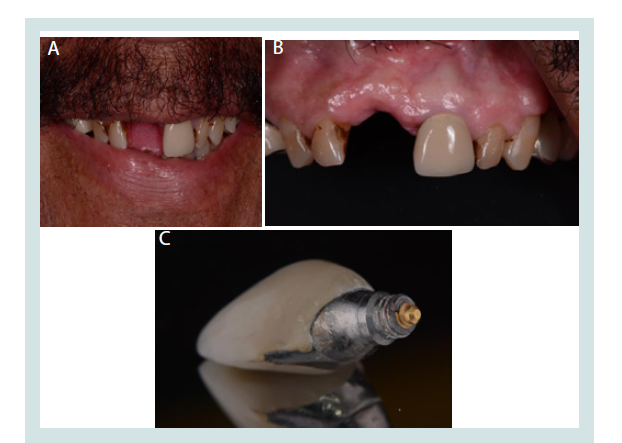
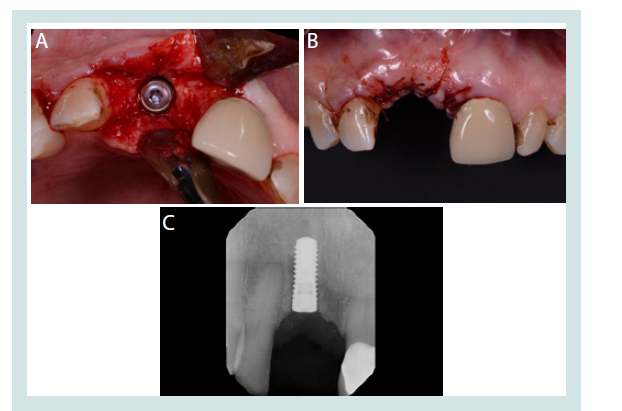
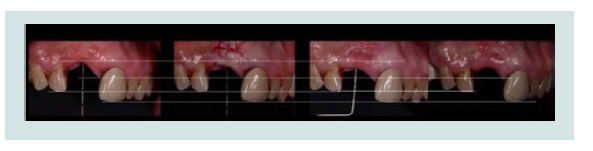
Clinical and radiographic evaluations were performed (Figure 1a-c and 2). Under local anesthesia (2% lidocaine, 1:100,000 epinephrine)
the fractured implant was removed with a trephine bur (Figure 3).
The patient rejected a flipper or a clear vacuum formed retainer due
to financial issue on missing #8siteat that moment. An analysis of
esthetics of the upper incisors was performed. Three options were
considered including 1) A new implant supported crown, 2) A fixed
bridge #7-#9, 3) A removable denture. These three options were
presented to the patient. The patient desired a new implant and fixed
restoration. Following three months of healing, the horizontal ridge
was intact with 2mm vertical defect. A crestal incision was performed
and a full thickness flap was elevated. Straumann implant osteotomy
protocol was followed. A new implant (Straumann 4.1×12 mm
Roxolid SLActive) was placed without surgical guide (Figure 4a-c).
The cover screw was placed and the flap was sutured with 4-0 chromic
gut (Henry Shein, Melville, NY). A clear vacuum formed retainer was
delivered with resin filled on #8 for an esthetic reason. Five weeks
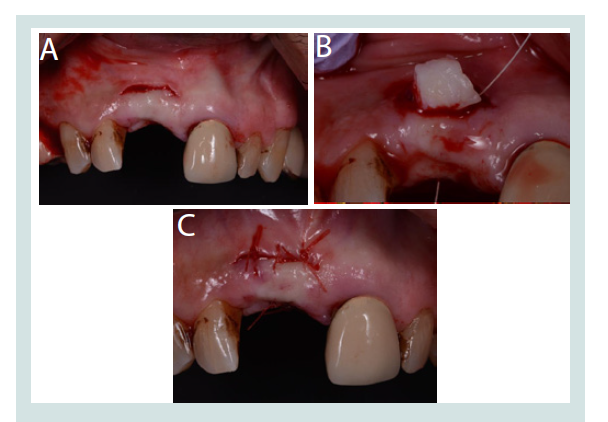
after following implant surgery (Figure 5), options of augmenting
the soft tissue or using pink porcelain were presented to the patient.
The patient chose soft tissue augmentation. The patient agreed with
the diagnosis and treatment plan. A soft tissue subepithelial graft
obtained from maxillary tuberosity was inserted with a tunneling
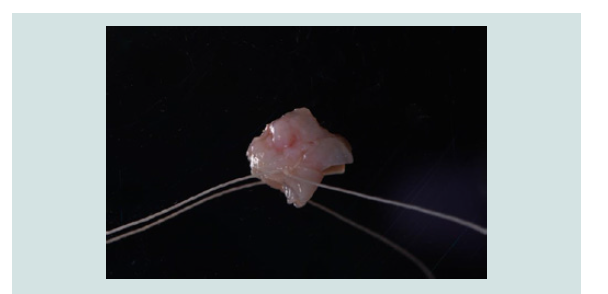
procedure which increased vertical dimension (Figure 7a-c and 8). Deepithelialized connective tissue was prepared for tunneling
graft. After soft tissue healing, the increased vertical dimension of
soft tissue was gained (Figure 9 and 10). Five weeks after soft tissue
grafting, second stage surgery was done by positioning the flap
apically to further improve the dimensions of the mid buccal tissue
and provisional crown on upper right central incisor implant (#8) was
placed. Soft tissue healing and contouring with provisional crown was
done after two months following the soft tissue grafting (Figure 11).
Figure 4: A: Occlusal view of new implant placement. B: After suture. C: Periapical radiograph after implant placement.
After placement of a provisional crown, the patient was given
several options for the final crown according to the ideal ways. The
suggested options were 1) Single all ceramic crown, 2) Single PFM
crown and 3) Two (two centrals), Four (lateral to lateral) or Six (canine
to canine) anterior crowns according 4) one implant supported crown (#8) and five laminate veneers (#6,#7,#9,#10,#11) to smile designs.
However, after listening to all treatment options, patient chose #8
single restoration and suggested metal crown with labial composite
window. The patient already has his suggested implant crown on his
upper left first premolar (site #12) (Figure 12). This kind of treatment
in dentistry has been used in pediatric dentistry for esthetic sp crown
or in esthetic pontic of fixed bridge on posterior teeth. Finally, the
metal crown with labial composite window was installed on #8 site (Figure 13).
Figure 7: A: Incision for tunneling technique. B: Grafting deepithlized
connective tissue. C: Suture after tunneling technique.
Figure 11: Provisional crown on upper rightcentral incisor( #8), Two months
after soft tissue graft.
Figure 12: Patient already has the metal implant crown with labial composite
window on upper left 1st premolar (#12).
Discussion
The notion of aesthetics in dental treatment may be similar or very different from clinician and patient point of view [6]. According
to the study of Burgueño-Barris, even esthetics is very different
within the group of dentists [7]. In general, the average person is less
sensitive to aesthetic differences in dental treatment than dentists [8].
Despite this aesthetic difference between the dentists and the patients,
most patients choose teeth that mimic the shade and shape of the
surrounding teeth when deciding the type of the anterior prosthesis
[9]. However, some patients make different decisions than ordinary
patients for other reasons, such as their religious, cultural, educational
background, and economic background [10].
In this patient, the mesio-distal width of #9 is 10.2 mm, and #8 is
11.2 mm. The height difference between the apical gingival line of #9
and #8 is 2 mm, #8 is higher than #9 and there is a periodontal defect
at #8. When informed the patient of these differences, the patient
readily understood these differences. When options of single implant
crown, fixed crown bridges, and removable dentures are given as
a treatment of #8, the patient selected single implant crown. The
patient also agreed with the soft tissue augmentation treatment for
#8. Patient was given a choice to pick palate or maxillary tuberosity as
a donor site for his soft tissue graft, patient chose to go with maxillary
tuberosity as it is less pain full procedure compared to the graft from
palate.
Patient selected the resin facing metal crown compared to type
of crowns presented by the dentist to him. The patient already has
a resin facing metal implant crown as a treatment method for #12
in a general local dental clinic. The background for the making the
choice of having resin facing metal implant crown on #12 is, the
ceramic chipped on the PFM crown which he had earlier on the same
tooth. When a new treatment is required after #8 implant fractured,
the treatment options were selected by the clinician for implant
treatment. However, the final selection of the type of crown was
chosen by the patient as resin-facing metal crown. When he smiled or
talked after treatment, the metal was exposure, but the patient did not
concern about this exposure of metal on #8. Even he considered this
exposure metal as strong image of himself.
Recently, there is no report on using resin facing crown or
implant crown in adult. According to the study of [11], the study
described that the composite resins and thermoplastics are bonded
to the metal. This type of pre veneered crown was developed to serve
as a convenient, durable, reliable, and esthetic solution to the difficult
challenge of restoring severely carious primary incisors. Moreover,
reported that the resistance to fracture and attrition is good in pre
veneered stainless steel crowns [12]. The main disadvantage is the
resin shades which give an artificial look. The study by reported that
stainless steel crowns are a highly retentive restoration [10]. However,
there was a high prevalence of facing failure with about 1/3 of the
facings showing complete or substantial facing loss. Facing failures
occurred most commonly at the resin-resin and resin-metal interface.
According to Jamil’s report, there is a case in which the Amazon
tribe required similar treatment methods for religious reasons [14].
According to preference studies on the types of anterior prosthesis in
general patients, all ceramic, PFM, are preferred to treatments similar
to surrounding teeth. This is also the way suggested by dentists. It
should be understood that most aesthetic criteria may not apply in
all cases when applying the selection criteria of anterior maxillary
prostheses with aesthetic needs in dental treatment.
Conclusion
In this case, we can understand that the patient may not choose
the treatment from the opinions presented by the experts but from
his esthetic criteria by means of the popularization of information
about the aesthetic part of dental care and the factors related to age,
race, sex, and economic situation. Also, many dental professionals
should keep in mind that the patients can make subjective choices of
aesthetics in their own treatment.