Journal of Oral Biology
Download PDF
Case Report
Case Presentations and Evolution in Concepts of Immediate Loading in Edentulous Mandible
Ki Bum Kim*,Bhupesh Mandali, Wendy CW Wang and Zahra Bagheri
- Department of Periodontology and Implant Dentistry, New York University, USA
*Address for Correspondence: Ki Bum Kim, Department of Periodontology and Implant Dentistry, New York University, Clinic 5W, 345 E 24th St, New York, NY 10010, USA, Tel: +1-212-992-7040; E-mail: kbk211@nyu.edu
Citation: Kim KB, Mandali B, Wang WCW, Bagheri Z. Case Presentations and Evolution in Concepts of Immediate Loading in Edentulous Mandible. J Oral Biol. 2018; 5(1): 6.
Copyright: © 2018 Kim KB, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Oral Biology | ISSN: 2377-987X | Volume: 5, Issue: 1
Submission: 15 January, 2018 | Accepted: 16 February, 2018 | Published: 26 February, 2018
Keywords
Immediate loading; Splinting of implants; Paralleling guide; Optimal position; Angulation of implants
Abstract
The purpose of this case series is to demonstrate an innovative paralleling device and a step by step surgical and prosthetic approach for achieving buccolingual and mesiodistal parallelism of immediately loaded implants. Clinical outcomes including success rates, indications, advantages, complications and limitations of this technique in cases using an Immediate Loading (IL) protocol will be discussed. Thirteen consecutive cases from the database that were treated with an IL protocol utilizing a paralleling device were included in this study. The treatment sites included the interforamina area in 8 totally edentulous and 5 partially edentulous mandibles. In this case series the average survival rate was 98.4% with a loading period of 6-28 months. There was one implant failure, one provisional restoration fractured and two cases with cement wash out during the follow-up period. Results of this case series demonstrated that implant placement in optimal position and angulation using the suggested IL protocol and paralleling device produces predictable results. It is also simpler, faster and more cost effective than the screw retained protocol.
Introduction
Increasing patient’s expectations and the need for a fixed dentition during implant treatment led to the development of implant immediate loading procedures with provisional fixed prostheses [1-4]. The benefits of immediate implant loading include the restoration of esthetics, improving self-esteem, shortening treatment times, eliminating issues arising from the use of removable prostheses and a more rapid post-operative functional recovery [5]. Subsequently, there is gradual reincorporation of a normal diet with a more balanced nutrition.
In 1985, Schroeder introduced a single stage approach with TPS implants in which the coronal part of the one piece solid implant was placed slightly supramucosally, led to predictable clinical results [6]. Ericsson et al were among the first to show that turned implants could osseointegrate equally well with a one-stage approach in the interforaminal area of the mandible without jeopardizing bone remodeling [7]. Even after 5 years in function, implant survival and bone remodelling were comparable in the anterior mandible [8].
Several investigators thereafter, documented high success rates with the use of immediate and early loaded implants supporting full-arch fixed restorations in the mandible [9-13]. Immediate loading results for such restorations are dependent on the number of implants, the type of prosthesis, the presence or absence of splinting, the occlusal scheme, and the jaw being restored [14]. The use of immediate loading of splinted implants to restore edentulous arches has been documented. Tarnow et al. published their experiences with the immediate loading of edentulous arches in 10 patients [3]. The group placed 107 implants, 50 of which were immediately loaded. Two failures were recorded in the mandible of the experimental group. The authors attributed the failures to removal of the provisional prostheses for evaluation of implant healing. Tarnow et al proposed that cross-arch stabilization should be attempted in edentulous arches by splinting the implants by using a single provisional restoration. In addition, they also recommended leaving the provisional intra-orally at least two months post placement.
Despite following these guidelines, immediate loading still remains a technique sensitive procedure which requires precise implant placement and fabrication of an accurate provisional restoration for loading the implants. This is especially challenging in the mandibular anterior region where the arch’s curvature is greatest and the alveolar crest is often uneven. Therefore various techniques have been introduced to make this procedure less technique sensitive, less time consuming, more accurate and more predictable. These included computer guided surgery, laboratory processed provisional, use of an Omnivac shell to fabricate cement retained provisional, use of angled abutments and use of temporary abutments to adjust the angulation during provisionalization [3,15]. These techniques are either expensive or time consuming yet not predictable. The latter of these techniques would not be necessary if implants were placed in optimal position and angulation with proper interimplant distance.
The purpose of this case series is to introduce an innovative technique that is cost effective, fast and predictable. A paralleling device and step by step guide for surgical and prosthetic rehabilitation approach with cement retained restoration for achieving buccolingual and mesiodistal parallelism of immediately loaded implants is demonstrated. Clinical outcomes including success rates, indications, advantages, complications, and limitations of this technique in cases using an immediate loading protocol will be discussed.
Materials and Methods
Clinical data in this study was obtained from the Implant Database (ID). This data was extracted as de-identified information from the routine treatment of patients at the Ashman Department of Periodontology and Implant Dentistry at the New York University College of Dentistry (NYUCD) Kriser Dental Center. The ID was certified by the Office of Quality Assurance at NYUCD. This study is in compliance with the Health Insurance Portability and Accountability Act (HIPAA) requirements and approved by the University Committee on activities involving human subjects.
Thirteen consecutive cases from the database that were treated with an IL protocol utilizing the paralleling device were included in this study.
Patient inclusion criteria: All of the included patients had:
1) A total of 3-6 implants placed and immediately loaded on the same day of the surgery with a chair-side provisional restoration.
2) Totally edentulous mandible or partially edentulous mandible with more than 5 teeth that required extraction in the anterior mandible due to periodontal disease, fracture or failure of endodontic treatment.
3) An adequate anterior-posterior (A-P) spread that was present in the lower arch.
4) The treatment sites were limited to the interforamina area. A total of 9 edentulous and 5 partially edentulous mandibular cases were selected to be included in the study.
5) All cases need to be treated with same technique steps and device.
2) Totally edentulous mandible or partially edentulous mandible with more than 5 teeth that required extraction in the anterior mandible due to periodontal disease, fracture or failure of endodontic treatment.
3) An adequate anterior-posterior (A-P) spread that was present in the lower arch.
4) The treatment sites were limited to the interforamina area. A total of 9 edentulous and 5 partially edentulous mandibular cases were selected to be included in the study.
5) All cases need to be treated with same technique steps and device.
Patient exclusion criteria: All patients that were excluded fromthe study had:
1) Systemic diseases that could alter the tissue integration of dental implants.
2) Generalized active periodontal disease or active periapical infection in the remaining teeth.
3) Parafunctional habits.
4) Lack of compliance.
5) Bone grafts at the time of placement.
2) Generalized active periodontal disease or active periapical infection in the remaining teeth.
3) Parafunctional habits.
4) Lack of compliance.
5) Bone grafts at the time of placement.
Clinical procedures: A set protocol was established, standardized and applied to all 14 patients as follows;
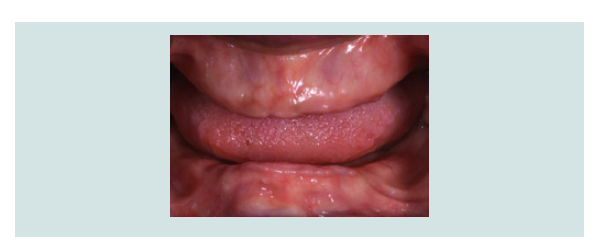
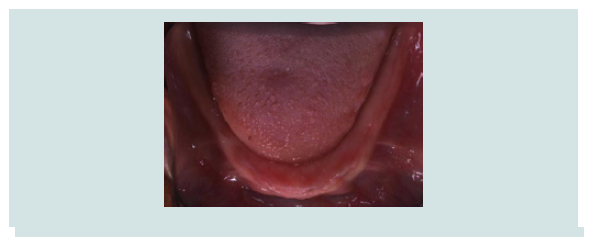
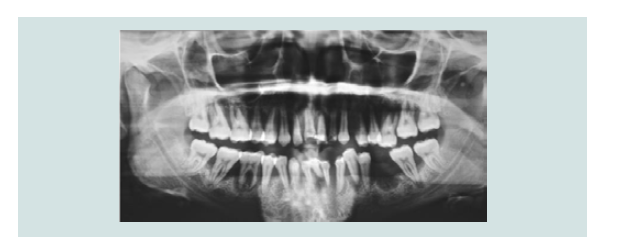
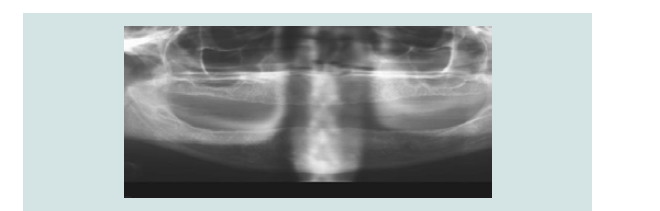
1) Clinical and radiographic examinations were made (Figures 1-5).
2) Pre-surgical steps - Stereolithographic model is printed usingthe CBCT scan of the edentulous mandibular arch (Figure 6). Vacuum form shells and resin shells fabricated from anideal wax up or pre-existing denture, and a bite registrationon the occlusal surface of the shell with pattern resin (GCcorporation, Tokyo, Japan) to evaluate the vertical dimensionof occlusion.
3) Subjects took 2 g Amoxicillin (TEVA, USA) 1 hour priorto surgery and in those allergic to Penicillin, 600 mg ofClindamycin (Pharmaderm, Princeton, NJ) was given.
4) Mid-crestal and when necessary vertical incisions were madeafter local anesthesia infiltration (2% lidocaine 1:100,000epinephrine [Henry Schein USA]).
5) Atraumatic tooth extraction took place in cases whereimmediate implant placement was performed.
6) Full thickness mucoperiosteal flaps were reflected.
7) Alveoloplasty was performed in cases where the alveolarridge required contouring using dental bur.
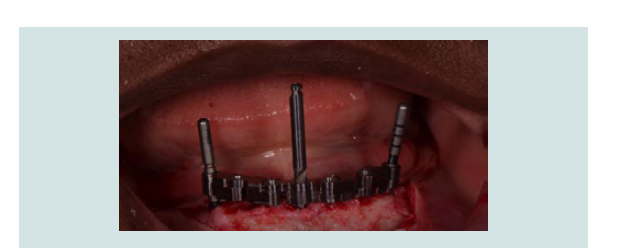
8) A total of 3-6 implants were placed in each mandible using anadjustable paralleling device. The implant placement utilizingan IL protocol featuring implant surfaces with either aResorbable Blast Media (RBM) , 4.0mm or Sandblasted, Largegrit, Acid-etched (SLA) surface in the endosseous portion(Figure 7). A crestally widened implant platform diameter of4.8 mm, a body diameter of 3.3 or 4.1 mm and a length of 12 or13 mm (Sybron XRT, Orange, CA, Straumann Standard Plus,Basel, Switzerland Nobel Biocare Branemark MkIII TiUnite,Balsberg, Switzerland) were used. Primary stability of eachimplant was achieved by undersizing the osteotomy andengaging a widened crestal platform of the implant with thecortical bone. This meant that the 2 different types of implantswere placed differently. The RBM surfaced implants with themicro thread up to the platform were placed evenly with thecrestal bone. The SLA surfaced implants were placed 2 mmmore apical than the roughened surface in order to engagethe widened neck with the crestal bone. Primary stability ofmore than 30 Ncm was confirmed for each placement using atorque driver.
9) The narrow diameter abutments (platform switchingconcept) were connected at a torque of more than 30 Ncmand wound closure was achieved using 4.0 resorbable sutures(Vicryl Ethicon).
10) A fixed provisional restoration was fabricated chair-side forcross-arch stabilization. The Omnivac shell or resin shellwas mounted to verify that the abutment fit in the template.Prefabricated plastic copings were placed on the abutmentsand a self-curing acrylic resin or Bis-acryl Luxatemp (DMG,Hamburg, Germany) was then injected into the template(Figure 10). The template was seated with bite registrationand guidance from adjacent teeth and/or the opposite jaw,and allowed to set for 4 minutes while the patient was biting inmaximum intercuspation. After the temporary prosthesis wasremoved from the abutment, excess material was trimmedoutside the mouth and occlusal adjustments were made.
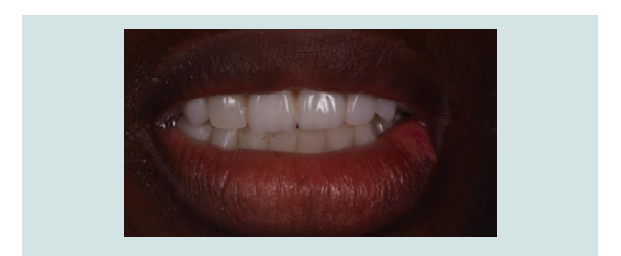
11) The provisional restoration was cemented with Polycarboxyliccement (Durelon 3M ESPE, Norristown, PA) and all implants were immediately loaded in function (Figures 11 and 12).
12) The patient presented for postoperative care at 1 week, 2 weeksand then once every month following implant placement tomonitor oral hygiene, mucosal healing, the stability of theprovisional bridge, and fixture status. The patients wereinstructed to follow a soft diet for 6-8 weeks after surgery.Each patient was prescribed antibiotics (Amoxicillin 500mg TID or Clindamycin 150 mg QID) and Chlorhexidinegluconate for 1 week following the surgery (Figure 13).
13) The provisional prosthesis was not removed to avoid an excessof micro movement until the healing period was completed.Follow up panoramic radiographs were taken.
14) After 3 months of healing period, the provisional restorationwas removed to evaluate implant mobility and periimplantsoft tissue.
15) The definitive prosthesis was fabricated after a final impressionwas obtained 3-6 months after implant placement.
2) Pre-surgical steps - Stereolithographic model is printed usingthe CBCT scan of the edentulous mandibular arch (Figure 6). Vacuum form shells and resin shells fabricated from anideal wax up or pre-existing denture, and a bite registrationon the occlusal surface of the shell with pattern resin (GCcorporation, Tokyo, Japan) to evaluate the vertical dimensionof occlusion.
3) Subjects took 2 g Amoxicillin (TEVA, USA) 1 hour priorto surgery and in those allergic to Penicillin, 600 mg ofClindamycin (Pharmaderm, Princeton, NJ) was given.
4) Mid-crestal and when necessary vertical incisions were madeafter local anesthesia infiltration (2% lidocaine 1:100,000epinephrine [Henry Schein USA]).
5) Atraumatic tooth extraction took place in cases whereimmediate implant placement was performed.
6) Full thickness mucoperiosteal flaps were reflected.
7) Alveoloplasty was performed in cases where the alveolarridge required contouring using dental bur.
8) A total of 3-6 implants were placed in each mandible using anadjustable paralleling device. The implant placement utilizingan IL protocol featuring implant surfaces with either aResorbable Blast Media (RBM) , 4.0mm or Sandblasted, Largegrit, Acid-etched (SLA) surface in the endosseous portion(Figure 7). A crestally widened implant platform diameter of4.8 mm, a body diameter of 3.3 or 4.1 mm and a length of 12 or13 mm (Sybron XRT, Orange, CA, Straumann Standard Plus,Basel, Switzerland Nobel Biocare Branemark MkIII TiUnite,Balsberg, Switzerland) were used. Primary stability of eachimplant was achieved by undersizing the osteotomy andengaging a widened crestal platform of the implant with thecortical bone. This meant that the 2 different types of implantswere placed differently. The RBM surfaced implants with themicro thread up to the platform were placed evenly with thecrestal bone. The SLA surfaced implants were placed 2 mmmore apical than the roughened surface in order to engagethe widened neck with the crestal bone. Primary stability ofmore than 30 Ncm was confirmed for each placement using atorque driver.
9) The narrow diameter abutments (platform switchingconcept) were connected at a torque of more than 30 Ncmand wound closure was achieved using 4.0 resorbable sutures(Vicryl Ethicon).
10) A fixed provisional restoration was fabricated chair-side forcross-arch stabilization. The Omnivac shell or resin shellwas mounted to verify that the abutment fit in the template.Prefabricated plastic copings were placed on the abutmentsand a self-curing acrylic resin or Bis-acryl Luxatemp (DMG,Hamburg, Germany) was then injected into the template(Figure 10). The template was seated with bite registrationand guidance from adjacent teeth and/or the opposite jaw,and allowed to set for 4 minutes while the patient was biting inmaximum intercuspation. After the temporary prosthesis wasremoved from the abutment, excess material was trimmedoutside the mouth and occlusal adjustments were made.
11) The provisional restoration was cemented with Polycarboxyliccement (Durelon 3M ESPE, Norristown, PA) and all implants were immediately loaded in function (Figures 11 and 12).
12) The patient presented for postoperative care at 1 week, 2 weeksand then once every month following implant placement tomonitor oral hygiene, mucosal healing, the stability of theprovisional bridge, and fixture status. The patients wereinstructed to follow a soft diet for 6-8 weeks after surgery.Each patient was prescribed antibiotics (Amoxicillin 500mg TID or Clindamycin 150 mg QID) and Chlorhexidinegluconate for 1 week following the surgery (Figure 13).
13) The provisional prosthesis was not removed to avoid an excessof micro movement until the healing period was completed.Follow up panoramic radiographs were taken.
14) After 3 months of healing period, the provisional restorationwas removed to evaluate implant mobility and periimplantsoft tissue.
15) The definitive prosthesis was fabricated after a final impressionwas obtained 3-6 months after implant placement.
Figure 1: A 25 year old female reported to NYU Department of Implantology with a chief complaint of missing upper and lower teeth. She lost her teeth due to generalised aggressive periodontitis.
Figure 4: Panoramic radiograph shows severe bone loss around all teeth in maxillary and mandibular arches indicative of aggressive generalised periodontitis.
Figure 6: Stereolithographic model of the planned alveoloplasty site. Thesurgical paralleling guide is adjusted in accordance with the plannedalveoloplasty procedure in the model prior to surgery.
Figure 7: Paralleling Guide Block (EBI, Kyungsan, Korea) placed in the osteotomy sites confirming the parallelism of the preparation of osteotomies.
Figure 9: Post implant placement and suturing the flap, temporary abutments are connected to the implants.
Figure 10: Temporary printed copings are placed on the abutments to receive the splinted provisional bridge.
Figure 11: Immediate provisional splinted restoration prevents macro-motion to avoid disruption of osseointegration.
Results
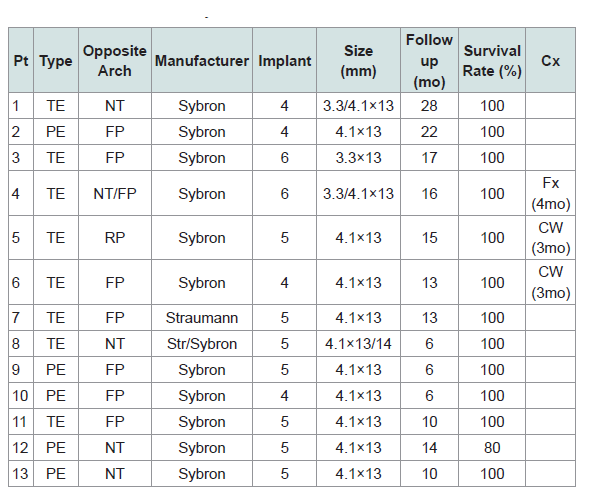
In this case series the average survival rate was 98.4% with a loading period of 6-28 months. Out of thirteen patients, twelve demonstrated 100% implant success rate. Only one implant failed in a patient whom received 5 implants with immediate placement. One provisional restoration fractured and two cases with cement wash out during the follow-up period (Table 1).
Discussion
The immediate loading (IL) of implant-supported fixed prostheses is clinically well documented with a reported 85.7-100% implant survival rate in the edentulous mandible [15]. Immediate loading of immediately placed implant has also shown a high success rate of 97.7-100% comparable to immediate loading of two stage implant as long as primary stability achieved [10,16,17]. The results of the present study indicate similar implant survival rates [18]. In this case series, a total of 63 implants were placed in 13 patients using the paralleling device and all immediately loaded. The average survival rate was 98.4% with a loading period of 6-28 months. Primary stability of more than 30 Ncm of torque was achieved by under- sizing the osteotomy and engaging the widened crestal platform of the implant with the cortical bone. There was one implant failure. This implant was placed immediately after extraction. Authors believe the failure was due to minimum primary stability and micromotion.
One provisional restoration fractured and two presented with cement wash out during the follow-up period. However in all cases the prosthesis was maintained in place during the first 2-4 months of the healing phase.
Other critical factors for implant success are achieving optimal implant position and angulation from next page. Creating a flat bony contour is the initial step to establish optimal implant position and angulation as well as to define anatomy to maximize implant fixation for immediate load prosthesis [19]. This osteoplasty creates a flat contour on which the restoration is placed. The plat contour serves multiple functions for both the surgeon and the prosthodontist. That include:
1) Establishing prosthetic restorative space.
2) Establishing a level alveolar plane and uniform implant levels.
3) Establishing alveolar width for implant diameter selection.
4) Bone reduction makes basal bone accessible for implant fixation.
5) Helps to establish arch form, implant distribution andanterior posterior spread.
6)Identifies optimal implant sites.
2) Establishing a level alveolar plane and uniform implant levels.
3) Establishing alveolar width for implant diameter selection.
4) Bone reduction makes basal bone accessible for implant fixation.
5) Helps to establish arch form, implant distribution andanterior posterior spread.
6)Identifies optimal implant sites.
In the mandible, segmental over eruption of the ridge and/or uneven alveolar crest are common findings. The ridge contouring bur is used to contour the ridge and establish a flat bony contour which helps implant placement at the same level and helps establish a prosthetic platform.
Optimal implant position in terms of ideal inter-implant distancecan be achieved if the implant is placed in the tooth position. This canbe done by using a surgical guide which is made from an ideal waxup that is prepared pre-surgically. However, implant placement alsodepends on the anatomy and morphology of bone and sometimesimplants cannot be placed in the ideal tooth position due to lackof bone availability. Computer generated surgical guide can helpoptimizing the implant placement. However it requires the use ofspecial softwares and certain expertise making the procedure costly.The technique introduced here can produce similar predictableresults while being more cost effective. A pre-operative step essentialto treatment planning the implant position is to obtain a 3Dstereolithographic model of the mandible.
Surgical templates facilitate placement of implants in the planned position and can be created with planning software using computed tomography (CT) or cone beam computed tomography (CBCT) data. Another option would be to plan and manufacture the guides on 3D stereolithographic models. Planning implant positions with computer-based methods and stereolithographic surgical templates achieves high cumulative survival rates (CSR) for implants at 1 year of follow-up [20]. In such an approach, bone reduction is first performed directly on the 3D model; drilling is performed by the oral surgeon. The surgeon then performs the implant osteotomies directly on the 3D models. This is followed by fabrication of both the bone reduction guide and the surgical guides. The 3D model allows further evaluation of the planned placement according to the anatomical structure of the patient prior to actual placement and manufacture of the guide on that basis. Aires I et al. conducted a retrospective study of implants placed and immediately loaded using 3D stereolithographic models [21]. Patients with failing dentition received implants and final multiunit abutments on the same day of surgery. In addition to the benefits to the patients, 3D modeling is viewed as being particularly user-friendly among craniofacial surgeons and highly reliable and accurate [22,23]. Three-dimensional modeling in contrast to computer planning of implant surgery does not require specific software. Furthermore, while computer planning only allows the surgeon to see the bone structure on a two-dimensional screen, 3D models enable the surgeon to physically examine the bone structure at all angles and use this information to formulate a step-by-step approach to the implant placement.
After the position of the implant has been identified, the direction/inclination of the implant must be determined. Establishing mesiodistal and buccolingual parallelism during implant placement is an important step. Adverse directions can impair the esthetics and function of the future restoration. Mesiodistal parallelism can be achieved using a surgical guide or the paralleling device. Surgical guides that are made custom based can add to the cost of the technique and their insertion require extra step. The paralleling device introduced here can be reused after sterilization, makes the technique more simple and cost effective.
It has been reported that the critical factors for successful IL are implant stability upon insertion and cross arch splinting via a rigid implant supported bridge to decrease micromotion less than 50-150 nm at the bone-implant interface [24]. If three or more implants are placed in a tripod or a cross-arch configuration, splinting a provisional bridge as soon as possible after implant placement reduces lateral forces on implants and allows more favorable axial forces [3,25,26].
Temporization in IL can be accomplished using different techniques. These include use of an Omnivac shell to prepare chairside cement retained provisional, use of a premade resin shell to fabricate a cement-retained provisional, use of lab processed provisional or conversion of an existing denture into a screw-retained provisional [18]. Since the late 1990’s, cement-retained restorations have been the preferred method with high success rates while aiding IL restorative time reduction [19,27]. Screw-retained restorations are more technique sensitive and time consuming when fabricated chairside. Moreover, cost is increased due to the additional laboratory and clinical components, and it is difficult to obtain non-passive bridgework [28]. Parallel alignment avoids use of angled abutment or abutment adjustment [29]. Bony stress is concentrated in the cervical area of an implant, therefore cervical cortical bone serves as the major anchoring point for an implant [3,29]. Parallel implant placement also reduces the stresses at the implant and bone interface since the implant does not have a PDL which acts as a shock absorber in teeth. A midline guide pin and a paralleling device may be used to obtain good parallelism. Other factors for successful provisionalization with an IL protocol include careful cementation. Permanent cementation is recommended because the prosthesis must remain fixed during the first 8 to 12 weeks post-surgically otherwise implant stability and osseointegration may be compromised. Additional care must be taken to limit cement extrusion beyond the abutment restoration margin and into the periimplant mucosal tissues because residual cement may cause inflammation and compromise bone and soft tissue healing [30].
Conclusion
Results of this case series demonstrated that implant placement in optimal position and angulation can be easily achieved using the suggested innovative immediate loading technique using paralleling device producing predictable results. Employing a cement retained provisional restoration with this technique is simpler, faster and more cost effective than the screw-retained protocol. Nevertheless, future prospective studies with long-term follow-up and an increased number of cases are necessary to further evaluate this technique.
References
- Schnitman PA, Wohrle PS, Rubenstein JE (1990) Immediate fixed interim prostheses supported by two- stage threaded implants: methodology and results. J Oral Implantol 16: 96-105.
- Balshi TJ, Wolfinger GJ (1997) Immediate loading of Brånemark implants in edentulous mandibles: a preliminary report. Implant Dent 6: 83-88.
- Tarnow DP, Emtiaz S, Classi A (1997) Immediate loading of threaded implants at stage 1 surgery in edentulous arches: ten consecutive case reports with 1- to 5-year data. Int J Oral Maxillofac Implants 12: 319-324.
- Horiuchi K, Uchida H, Yamamoto K, Sugimura M (2000) Immediate loading of Brånemark system implants following placement in edentulous patients: a clinical report. Int J Oral Maxillofac Implants 15: 824-830.
- Castellon P, Block MS, Smith MB Finger IM (2004) Immediate loading of the edentulous mandible: delivery of the final restoration or a provisional restoration--which method to use? J Oral Maxillofac Surg 62 (9 Suppl 2): 30-40.
- Buser D, Weber HP, Brägger U (1990) The treatment of partially edentulous patients with ITI hollow-screw implants: presurgical evaluation and surgical procedures. Int J Oral Maxillofac Implants 5: 165-175.
- Ericsson I, Randow K, Glantz PO, Lindhe J, Nilner K (1994) Clinical and radiographical features of submerged and nonsubmerged titanium implants. Clin Oral Implants Res 5: 185-189.
- Ericsson I, Randow K, Nilner K, Petersson A (1997) Some clinical and radiographical features of submerged and non-submerged titanium implants. A 5-year follow-up study. Clin Oral Implants Res 8: 422-426.
- Grunder U (2001) Immediate functional loading of immediate implants in edentulous arches: two-year results. Int J Periodontics Restorative Dent 21: 545-551.
- Capelli M, Zuffetti F, Del Fabbro M, Testori T (2007) Immediate rehabilitation of the completely edentulous jaw with fixed prostheses supported by either upright or tilted implants: a multicenter clinical study. Int J Oral Maxillofac Implants 22: 639-644.
- Tealdo T, Bevilacqua M, Pera F, Menini M, Ravera G, et al. (2008) Immediate function with fixed implant-supported maxillary dentures: a 12-month pilot study. J Prosthet Dent 99: 351-360.
- Maló P, Rangert B, Nobre M (2005) All-on-4-immediate-function concept with Brånemark system implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res 7 Suppl 1: S88-S94.
- Chiapasco M, Gatti C, Rossi E, Haefliger W, Markwalder TH (1997) Implant-retained mandibular overdentures with immediate loading. A retrospective multicenter study on 226 consecutive cases. Clin Oral Implant Res 8: 48-57.
- Ostman PO (2008) Immediate/early loading of dental implants. Clinical documentation and presentation of a treatment concept. Periodontol 2000 47: 90-112.
- Peñarrocha M, Boronat A, Garcia B (2009) Immediate loading of immediate mandibular implants with a full-arch fixed prosthesis: a preliminary study. J Oral Maxillofac Surg 67: 1286-1293.
- Szmukler-Moncler S, Salama H, Reingewirtz Y, Dubruille JH (1998) Timing of loading and effect of micro motion on bone-dental implant interface: review of experimental literature. J Biomed Mater Res 43: 192-203.
- Romanos G, Froum S, Hery C, Cho SC, Tarnow D (2010) Survival rate of immediately vs delayed loaded implants: analysis of the current literature. J Oral Implantol 36: 315-324.
- Misch CM (2004) Immediate loading of definitive implants in the edentulous mandible using a fixed provisional prosthesis: the denture conversion technique. J Oral Maxillofac Surg 62 (9 Suppl 2): 106-115.
- Romanos GE, Nentwig GH (2008) Immediate loading using cross-arch fixed restorations in heavy smokers: nine consecutive case reports for edentulous arches. Int J Oral Maxillofac Implants 23: 513-519.
- Malo P, de Araujo Nobre M, Lopes A (2007) The use of computer-guided flapless implant surgery and four implants placed in immediate function to support a fixed denture: preliminary results after a mean follow-up period of thirteen months. J Prosthet Dent 97 (6 Suppl): S26-S34.
- Aires I, Berger J (2016) Planning implant placement on 3D stereolithographic models applied with immediate loading of implant-supported hybrid prostheses after multiple extractions: a case series. Int J Oral Maxillofac Implants 31: 172-178.
- D'Urso PS, Atkinson RL, Lanigan MW, Earwaker WJ, Bruce IJ, et al. (1998) Stereolithographic (SL) biomodelling in craniofacial surgery. Br J Plast Surg 51: 522-530.
- Rosenfeld AL, Mandelaris GA, Tardieu PB (2006) Prosthetically directed implant placement using computer software to ensure precise placement and predictable prosthetic outcomes. Part 3: stereolithographic drilling guides that do not require bone exposure and the immediate delivery of teeth. Int J Periodontics Restorative Dent 26: 493-499.
- Rangert B, Jemt T, Jörneus L (1989) Forces and moments on Branemark implants. Int J Oral Maxillofac Implants 4: 241-247.
- Rangert BR, Sullivan RM, Jemt TM (1997) Load factor control for implants in the posterior partially edentulous segment. Int J Oral Maxillofac Implants 12: 360-370.
- Jensen OT, Adams MW, Cottam JR, Parel SM, Phillips WR 3rd (2011) The all on 4 shelf: mandible. J Oral Maxillofac Surg 69: 175-181.
- Bocklage R (2002) Rehabilitation of the edentulous maxilla and mandible with fixed implant-supported restorations applying immediate functional loading: a treatment concept. Implant Dent 11: 154-158.
- Cooper L, De Kok IJ, Reside GJ, Pungpapong P, Rojas-Vizcaya F (2005) Immediate fixed restoration of the edentulous maxilla after implant placement. J Oral Maxillofac Surg 63 (9 Suppl 2): 97-110.
- Pierrisnard L, Renouard F, Renault P, Barquins M (2003) Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res 5: 254-262.
- Pauletto N, Lahiffe BJ, Walton JN (1999) Complications associated with excess cement around crowns on osseointegrated implants: a clinical report. Int J Oral Maxillofac Implants 14: 865-868.