Journal of Obesity and Bariatrics
Download PDF
Research article
Clinical Effectiveness of Different Variants of Laparoscopic Sleeve Gastrectomy in Patients with Obesity
Ruziev US
Tashkent Medical Academy, Uzbekistan
*Address for Correspondence: Ruziev US, Tashkent Medical Academy, Uzbekistan, Email id:
nodira.bakieva2221@gmail.com
Submission: 07 May, 2025
Accepted:09 June, 2025
Published:11 June, 2025
Copyright: © 2025 Ruziev US. This is an open access article
distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction
in any medium, provided the original work is properly cited.
Keywords: Bariatric Surgery; Complications, Complication Prevention; Metabolic
Complications; Obesity; Surgical Safety
Abstract
Relevance:Laparoscopic sleeve gastrectomy (LSG) remains one of the most
commonly used surgical methods for the treatment of morbid obesity. However,
variations in the technical approaches to the procedure result in significant differences
in complication profiles, metabolic safety, and sustainability of weight loss.
Objective: To compare the clinical effectiveness, safety, and long-term outcomes of three LSG techniques: standard (Classic), reinforced (Hard), and modified with a preventive program (Soft).
Materials and Methods:The study included 1,194 patients who underwent LSG between 2019 and 2022. Early and late surgical and metabolic complications, changes in body weight, BMI, and indicators such as %TWL(total body weight loss), %EWL,(>50% excess weight loss) and %EBL(endoscopic band ligation)were assessed up to 36 months postoperatively. Weight regain was defined as an increase in BMI category after 12 months. Statistical analysis included χ², t-test, and Mann–Whitney test with a significance level of p<0.05.
Results:The Soft group showed the lowest complication rate (26.85%) compared to the Hard (49.39%) and Classic (35.22%) groups (p<0.001). The incidence of metabolic disorders was 15.76% in the Soft group versus 64.34% in the Hard group. The rate of late GERD was minimal in the Soft group (1.48%). Despite a less aggressive restriction, the Soft group achieved a high level of weight reduction: %EWL – 106.9 ± 21.1%, %TWL – 49.5 ± 8.9%, %EBL – 114.2 ± 22.1% at 12 months. Weight regain was observed in 30.3% of patients in the Soft group, significantly lower than in the Classic group (62.4%) and comparable to the Hard group (24.7%).
Conclusion:The modified LSG technique with an anatomically sparing approach and an integrated complication prevention program provides an optimal balance between weight loss effectiveness and safety. It demonstrated a lower complication rate and greater weight stability in the long term, making it a preferable option for most patients with obesity.
Objective: To compare the clinical effectiveness, safety, and long-term outcomes of three LSG techniques: standard (Classic), reinforced (Hard), and modified with a preventive program (Soft).
Materials and Methods:The study included 1,194 patients who underwent LSG between 2019 and 2022. Early and late surgical and metabolic complications, changes in body weight, BMI, and indicators such as %TWL(total body weight loss), %EWL,(>50% excess weight loss) and %EBL(endoscopic band ligation)were assessed up to 36 months postoperatively. Weight regain was defined as an increase in BMI category after 12 months. Statistical analysis included χ², t-test, and Mann–Whitney test with a significance level of p<0.05.
Results:The Soft group showed the lowest complication rate (26.85%) compared to the Hard (49.39%) and Classic (35.22%) groups (p<0.001). The incidence of metabolic disorders was 15.76% in the Soft group versus 64.34% in the Hard group. The rate of late GERD was minimal in the Soft group (1.48%). Despite a less aggressive restriction, the Soft group achieved a high level of weight reduction: %EWL – 106.9 ± 21.1%, %TWL – 49.5 ± 8.9%, %EBL – 114.2 ± 22.1% at 12 months. Weight regain was observed in 30.3% of patients in the Soft group, significantly lower than in the Classic group (62.4%) and comparable to the Hard group (24.7%).
Conclusion:The modified LSG technique with an anatomically sparing approach and an integrated complication prevention program provides an optimal balance between weight loss effectiveness and safety. It demonstrated a lower complication rate and greater weight stability in the long term, making it a preferable option for most patients with obesity.
Relevance of the Problem
Obesity is a chronic disease with pronounced systemic
consequences. Bariatric surgery, including LSG, provides significant
weight loss and improvement in comorbidities but is often
accompanied by complications such as bleeding, staple line leakage,
gastroesophageal reflux disease (GERD), and others. For example,
according to a study by Dang et al. (2021) based on MBSAQIP data
from 854 centers, the number of LSG procedures increased over 4
years, yet the risk of leaks (up to 1.1%) and bleeding (2–3%) remained.
[1] Moreover, technical modifications did not always reduce the
complication rate. According to Ullah et al. (2024), early complication
rates among 185 patients were: vomiting – 23%, GERD – 7%, staple
line leak – 5.8%, wound infection – 3.2%, with zero mortality.
The degree of gastric restriction during LSG significantly
influences the rate of various complications [2]. In a study by
Haskins IN et al. (2019), the use of a calibration bougie smaller than
36 Fr was associated with an increased rate of dehydration-related
complications, prompting the authors to call for standardization of
the procedure’s technical aspects [3].
Furthermore, Diab et al. (2023) demonstrated that oversewing the
staple line significantly reduces the incidence of leaks and bleeding.
Among 1,200 patients operated on using this technique, leaks were
observed in only 0.3%..[4].
Reytor-González et al. (2025) emphasized the risk of metabolic
complications, particularly iron, vitamin B12, and calcium
deficiencies, which occurred in more than 30% of patients within 12
months after LSG without adequate support..[5].
Among the most serious complications identified in a number of
studies are thromboembolic events, with an incidence within 30 days
after surgery potentially exceeding 2%, particularly in patients with a
body mass index (BMI) >50 and metabolic syndrome.
Given the wide range of both early and long-term surgical,
metabolic, and functional complications following LSG, as well as the
persistent variability in outcomes across different surgical techniques,
the need for further multicenter, randomized, and standardized
studies becomes evident. These studies should aim to objectively
assess risks, develop optimized technical approaches, and create
personalized protocols for complication prevention [6].
Materials and Methods
This study is considered to be comparative effectiveness study
and patients were allocated according to the levels of obesity who
are required in three different types of operations including classic,
hard and soft. In order to ensure comparability for comparison
while allocating patients similar indexes of weight of patients were
made a group. The study is considered to be prospective. In order
to accomplish this study permission was taken from the Tashkent
Medical Academy of ethics committee.
This comparative study was conducted from January 2019 to
December 2022. The objective was to evaluate the clinical effectiveness
and safety of different tactical and technical approaches to LSG in
obese patients. All patients were divided into three groups based
on the technique used: standard (Classic), reinforced (Hard), and
modified with an integrated preventive program (Soft)[7]
Patients aged 18 to 65 years with obesity were included in the
study, defined as: BMI ≥40 kg/m², or BMI ≥35 kg/m² in the presence
of at least one metabolic comorbidity (arterial hypertension, type 2
diabetes, dyslipidemia, obstructive sleep apnea, etc.).
A total of 1,194 patients were included in the study: 373 underwent
the Classic technique, 415 the Hard technique, and 406 the modified
Soft technique. The mean age was 36.6 ± 10.7 years, and 88.1% were
women. Most patients were diagnosed with class III obesity, along
with common metabolic comorbidities: hypertension (68.3%), type 2
diabetes (31%), dyslipidemia (54%), NAFLD (84.8%), and obstructive
sleep apnea (57.1%).
All surgeries were performed by a single experienced team (over
2,500 LSG procedures).
Classic: resection began 4–6 cm from the pylorus, using a 36–38 Frbougie, with partial preservation of the angle of His. No stapler line reinforcement was performed.
Hard: resection began 2–3 cm from the pylorus, using a 32–34 Frbougie, with full mobilization of the gastric fundus and sero-serosal suture reinforcement.
oft: a compromise approach with a 36 Frbougie, preservation of the incisuraangularis, placement of an invaginating suture, and implementation of a personalized perioperative preventive program (hydration, acid-base monitoring, micronutrient correction, early mobilization, etc.)[8]
Outcomes were evaluated based on body weight dynamics, body mass index (BMI), %EBL (percentage of excess body loss relative to ideal weight), %EWL (percentage of excess weight loss based on BMI), and %TWL (percentage of total weight loss from baseline)[9]. Assessments were performed preoperatively and at 3, 6, 12, and 36 months postoperatively. Weight regain was defined as an increase in BMI by at least one category after 12 months of follow-up..[10].
Classic: resection began 4–6 cm from the pylorus, using a 36–38 Frbougie, with partial preservation of the angle of His. No stapler line reinforcement was performed.
Hard: resection began 2–3 cm from the pylorus, using a 32–34 Frbougie, with full mobilization of the gastric fundus and sero-serosal suture reinforcement.
oft: a compromise approach with a 36 Frbougie, preservation of the incisuraangularis, placement of an invaginating suture, and implementation of a personalized perioperative preventive program (hydration, acid-base monitoring, micronutrient correction, early mobilization, etc.)[8]
Outcomes were evaluated based on body weight dynamics, body mass index (BMI), %EBL (percentage of excess body loss relative to ideal weight), %EWL (percentage of excess weight loss based on BMI), and %TWL (percentage of total weight loss from baseline)[9]. Assessments were performed preoperatively and at 3, 6, 12, and 36 months postoperatively. Weight regain was defined as an increase in BMI by at least one category after 12 months of follow-up..[10].
Results
When comparing the frequency of early postoperative
complications (within 30 days) among the three LSG groups, the
most favorable results were observed in the main group using the
modified (Soft) technique (Table 6.1). The overall rate of surgical
complications in this group was only 0.25% (1 out of 406 patients),
significantly lower than in the Hard group (2.41%, 10 out of 415)
and the Classic group (1.34%, 5 out of 373). All complications in the
Soft group were isolated and technically manageable; notably, there
were no cases of bleeding from the staple line, anastomotic leaks,
pulmonary embolism, or mesenteric thrombosis.
Regarding early metabolic complications, the group with the
modified LSG technique also demonstrated a clear advantage.
The incidence of complications such as metabolic acidosis,
hypovolemia, and hypercoagulation was only 15.76% (64 out of 406)
in the Soft group, which is significantly lower compared to 64.34% in
the Hard group (267 out of 415; χ²=201.232; p<0.001) and 25.74% in
the Classic group (96 out of 373; χ²=11.849; p=0.0006 when compared
to Soft).
The difference is particularly notable for the most common
metabolic disorders: metabolic acidosis occurred in 8.62% of patients
in the Soft group, versus 14.75% in the Classic group and 39.76%
in the Hard group; hypovolemia occurred in 9.11% versus 18.23%
and 50.36%, respectively. These data clearly demonstrate that the
implementation of an optimized perioperative prevention program
in the main group significantly reduced the risk of early postoperative
metabolic destabilization following LSG.
The initial number of patients included in further analysis was
adjusted for mortality: in the Classic group, 1 out of 373 patients died
(final n=372); in the Hard group, 2 out of 415 died (final n=413); and
in the modified sleeve resection group (Soft), there were no deaths.
In the long-term follow-up period (1–36 months post-LSG), the most favorable outcomes in terms of late surgical complications were again observed in the Soft group.
The overall complication rate was 1.72% (7 out of 406 patients), compared to 2.42% (9 out of 372) in the Classic group and significantly higher at 10.41% (43 out of 413) in the Hard group. The most frequent complication was gastroesophageal reflux disease (GERD), which occurred in 6 patients (1.48%) in the Soft group, compared to 2.42% in the Classic group and 9.20% in the Hard group.
In the long-term follow-up period (1–36 months post-LSG), the most favorable outcomes in terms of late surgical complications were again observed in the Soft group.
The overall complication rate was 1.72% (7 out of 406 patients), compared to 2.42% (9 out of 372) in the Classic group and significantly higher at 10.41% (43 out of 413) in the Hard group. The most frequent complication was gastroesophageal reflux disease (GERD), which occurred in 6 patients (1.48%) in the Soft group, compared to 2.42% in the Classic group and 9.20% in the Hard group.
The outcomes for late metabolic complications also demonstrated
a clear advantage for the Soft group.
Only 4 cases (0.99%) of such complications were registered among the 406 patients, significantly lower than in the Hard group – 6.78% (28 out of 413; χ²=18.309; p=0.00001878), and lower than in the Classic group – 1.34% (5 out of 372; χ²=0.219; p=0.6401). The most common issues in the standard technique groups were deficiencies of micro- and macronutrients (0.74% in the Soft group vs. 5.08% in the Hard group), along with isolated cases of hypoglycemia (1 case in the Soft group). No cases of malnutrition were reported in the Soft group, in contrast to 3 cases in the Hard group.
The overall incidence of other complications, including gallstone disease (GSD) and psychological disorders, was also lowest in the main group.
Among patients in the Soft group, the total number of such complications was 25.12% (102 out of 406), compared to 32.53% in the Classic group and 40.68% in the Hard group.
Psychological disorders were recorded in 36 patients (8.87%) in the Soft group – nearly half the rate compared to the Classic group (15.05%) and more than two times lower than in the Hard group (21.55%). These results likely reflect the lower anatomical and functional burden on patients and better long-term adaptation due to preservation of physiological reflexes and eating behaviors.
The surgical removal of the gallbladder, is sometimes performed concurrently with bariatric surgery, particularly in patients with existing gallbladder disease or those at high risk of developing it after rapid weight loss. The presence or absence of gallstones, as well as the specific bariatric surgery procedure performed, influences the
Only 4 cases (0.99%) of such complications were registered among the 406 patients, significantly lower than in the Hard group – 6.78% (28 out of 413; χ²=18.309; p=0.00001878), and lower than in the Classic group – 1.34% (5 out of 372; χ²=0.219; p=0.6401). The most common issues in the standard technique groups were deficiencies of micro- and macronutrients (0.74% in the Soft group vs. 5.08% in the Hard group), along with isolated cases of hypoglycemia (1 case in the Soft group). No cases of malnutrition were reported in the Soft group, in contrast to 3 cases in the Hard group.
The overall incidence of other complications, including gallstone disease (GSD) and psychological disorders, was also lowest in the main group.
Among patients in the Soft group, the total number of such complications was 25.12% (102 out of 406), compared to 32.53% in the Classic group and 40.68% in the Hard group.
Psychological disorders were recorded in 36 patients (8.87%) in the Soft group – nearly half the rate compared to the Classic group (15.05%) and more than two times lower than in the Hard group (21.55%). These results likely reflect the lower anatomical and functional burden on patients and better long-term adaptation due to preservation of physiological reflexes and eating behaviors.
The surgical removal of the gallbladder, is sometimes performed concurrently with bariatric surgery, particularly in patients with existing gallbladder disease or those at high risk of developing it after rapid weight loss. The presence or absence of gallstones, as well as the specific bariatric surgery procedure performed, influences the
decision to remove the gallbladder. Therefore patients who had
existing gallbladder diseases and those who were at a high risk of
developing it were considered for cholecystectomy. All the other
patients who didn’t have a higher risk weren’t operated.
Regarding GSD: 37 patients (9.11%) in the Soft group required
cholecystectomy, while another 48 (11.82%) were diagnosed with
light level of gallstones therefore did not require surgery. These
rates are lower compared to the Hard group (18.89% and 13.56%,
respectively) (χ²=22.416; p=0.0000022).
A comparative analysis of body weight reduction and
maintenance dynamics, BMI changes, as well as integrated indicators
such as %EBL, %TWL, and %EWL is presented next. This includes
both short- and long-term outcomes (up to 36 months), allowing for
an objective assessment of the quality and stability of the therapeutic
effect of each technique.
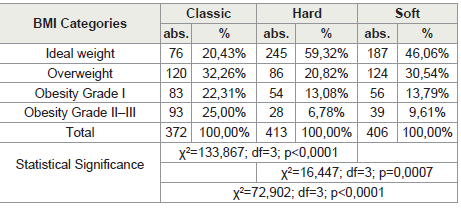
The best result in terms of BMI reduction was observed in the
Hard group, where 70.7% of patients reached their ideal BMI,
significantly higher than in the Classic group (42.2%) and the Soft
group (62.56%). However, it is important to interpret these data
considering not only the achieved outcomes but also the frequency of
associated complications typical of the reinforced technique.
In the Soft group, despite less pronounced BMI reduction compared to the Hard group, the rate of patients achieving ideal body weight was significantly higher than with the classic technique (62.56% vs. 42.2%), indicating high metabolic effectiveness of the modified approach with less gastric restriction and reduced risk of functional disorders.
The frequency of patients who remained overweight was highest in the Classic group (36.83%), while it was 23.73% in the Hard group and 25.86% in the soft group. This indicates intermediate effectiveness of the Soft technique, which balances sufficient weight loss with clinical safety.
The proportion of patients who retained class I and II obesity was lowest in the Hard group (5.33% and 0.24%, respectively), while in the Classic group, it reached 15.86% and 5.11%. In the Soft group, these rates were 9.11% and 2.46%, respectively, also demonstrating a more favorable residual obesity distribution compared to the Classic group, but without the signs of excessive aggressiveness observed in the Hard group.
In the Soft group, despite less pronounced BMI reduction compared to the Hard group, the rate of patients achieving ideal body weight was significantly higher than with the classic technique (62.56% vs. 42.2%), indicating high metabolic effectiveness of the modified approach with less gastric restriction and reduced risk of functional disorders.
The frequency of patients who remained overweight was highest in the Classic group (36.83%), while it was 23.73% in the Hard group and 25.86% in the soft group. This indicates intermediate effectiveness of the Soft technique, which balances sufficient weight loss with clinical safety.
The proportion of patients who retained class I and II obesity was lowest in the Hard group (5.33% and 0.24%, respectively), while in the Classic group, it reached 15.86% and 5.11%. In the Soft group, these rates were 9.11% and 2.46%, respectively, also demonstrating a more favorable residual obesity distribution compared to the Classic group, but without the signs of excessive aggressiveness observed in the Hard group.
In the Classic group, the average initial body weight was 133.9 ±
31.9 kg, decreasing to 108.7 ± 26.1 kg at 3 months, 81.0 ± 18.9 kg at 6
months, and 68.7 ± 13.4 kg at 12 months. In the Hard group, initial
weight was similar (132.4 ± 29.3 kg), but the weight loss was more
pronounced: 98.7 ± 24.6 kg at 3 months, 73.4 ± 16.6 kg at 6 months,
and 62.1 ± 12.3 kg at 12 months. These differences were statistically
significant compared to the Classic group (p<0.0001 at all time points
starting from 3 months).
In the main group (Soft), which used the modified LSG technique with an optimized complication prevention protocol, the initial average weight was 131.2 ± 27.6 kg. This decreased to 104.4 ± 23.9 kg at 3 months, 77.6 ± 18.7 kg at 6 months, and 65.6 ± 14.3 kg at 12 months. Compared to the Classic group, the results in the Soft group were significantly better at all time points (p<0.001), while differences compared to the Hard group were not statistically significant (p>0.05), confirming the comparable effectiveness of the modified technique in reducing body weight without excessive surgical aggression.
In the main group (Soft), which used the modified LSG technique with an optimized complication prevention protocol, the initial average weight was 131.2 ± 27.6 kg. This decreased to 104.4 ± 23.9 kg at 3 months, 77.6 ± 18.7 kg at 6 months, and 65.6 ± 14.3 kg at 12 months. Compared to the Classic group, the results in the Soft group were significantly better at all time points (p<0.001), while differences compared to the Hard group were not statistically significant (p>0.05), confirming the comparable effectiveness of the modified technique in reducing body weight without excessive surgical aggression.
Discussion
A comparative analysis of BMI reduction dynamics in the Classic,
Hard, and Soft groups confirmed significant differences during the
first year after LSG.
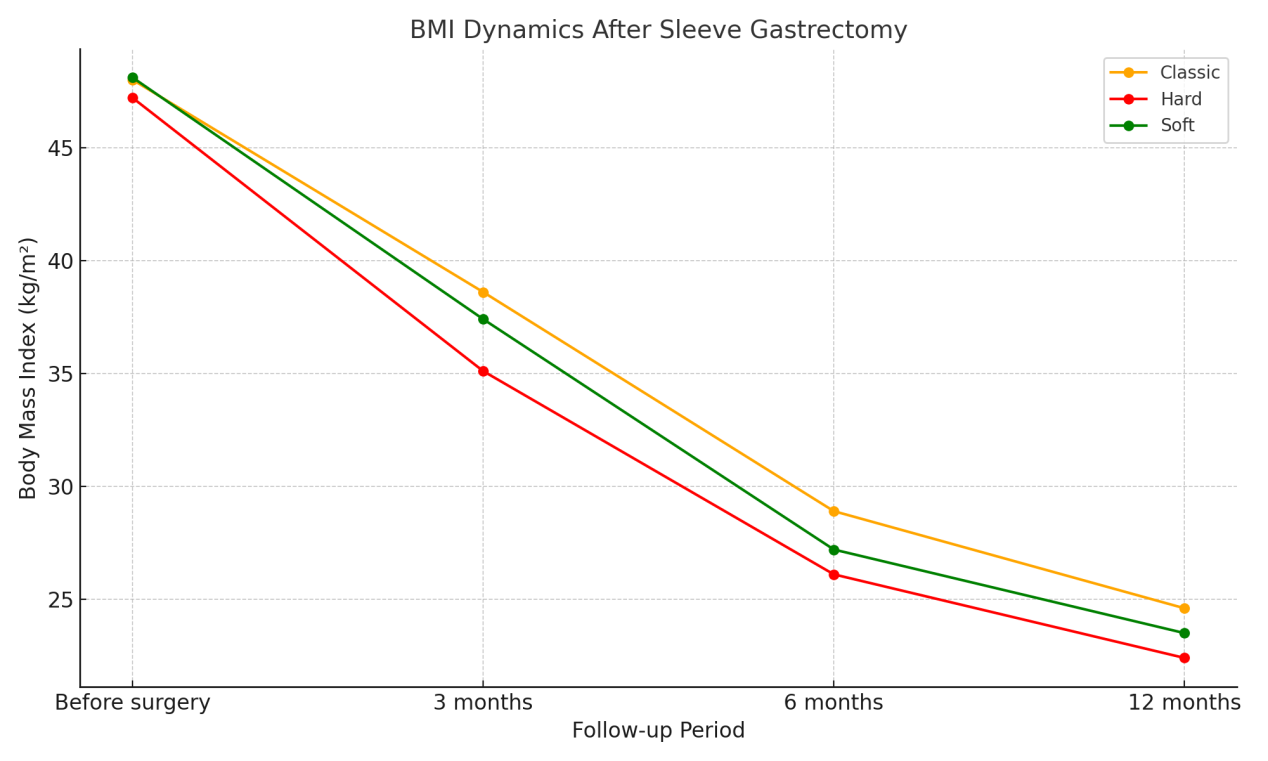
In the Classic group, the initial BMI averaged 48.0 ± 7.5 kg/m², decreasing to 38.6 ± 6.7 at 3 months, 28.9 ± 5.3 at 6 months, and 24.6 ± 3.9 at 12 months. In the Hard group, BMI reduction was more intense: from 47.2 ± 6.9 to 22.4 ± 3.8 kg/m² over one year, with significant differences compared to Classic at all time points (p<0.0001 from month 3). In the main group (Soft), using the modified LSG technique, the initial BMI was 48.1 ± 7.1 kg/m², dropping to 38.3 ± 6.8 at 3 months, 28.5 ± 5.2 at 6 months, and 24.1 ± 4.1 kg/m² at 12 months see [Figure 1].
Next, the effectiveness of weight reduction 12 months post-LSG was analyzed according to three key metrics: %EWL (Excess Weight Loss), %TWL (Total Weight Loss), and %EBL (Excess BMI Loss). In the Classic group, the average %EWL was 68.4 ± 15.2%, %TWL was 35.3 ± 9.7%, and %EBL was 72.5 ± 16.3%. In the Hard group, these values were higher: %EWL – 71.9 ± 13.7%, %TWL – 38.6 ± 8.5%, and %EBL – 75.6 ± 14.9%.
However, the highest effectiveness was observed in the Soft group, where weight reduction reached 106.9 ± 21.1% for %EWL, 49.5 ± 8.9% for %TWL, and 114.2 ± 22.1% for %EBL, which significantly exceeded the results in both other groups (p<0.001).
Weight regain, defined as a deterioration in BMI category compared to the 12-month result, was recorded in 62.4% (232 out of 372) of patients in the Classic group, 24.7% (102 out of 413) in the Hard group, and 30.3% (123 out of 406) in the Soft group.
The most stable long-term weight maintenance outcomes were observed in the Hard group (75.3%), while the Soft group demonstrated a stability rate of 69.7%, significantly higher than that of the Classic group (37.6%, χ²=80.5; p<0.0001), but not statistically different from the Hard group (χ²=3.22; p=0.073).
In the Classic group, the initial BMI averaged 48.0 ± 7.5 kg/m², decreasing to 38.6 ± 6.7 at 3 months, 28.9 ± 5.3 at 6 months, and 24.6 ± 3.9 at 12 months. In the Hard group, BMI reduction was more intense: from 47.2 ± 6.9 to 22.4 ± 3.8 kg/m² over one year, with significant differences compared to Classic at all time points (p<0.0001 from month 3). In the main group (Soft), using the modified LSG technique, the initial BMI was 48.1 ± 7.1 kg/m², dropping to 38.3 ± 6.8 at 3 months, 28.5 ± 5.2 at 6 months, and 24.1 ± 4.1 kg/m² at 12 months see [Figure 1].
Next, the effectiveness of weight reduction 12 months post-LSG was analyzed according to three key metrics: %EWL (Excess Weight Loss), %TWL (Total Weight Loss), and %EBL (Excess BMI Loss). In the Classic group, the average %EWL was 68.4 ± 15.2%, %TWL was 35.3 ± 9.7%, and %EBL was 72.5 ± 16.3%. In the Hard group, these values were higher: %EWL – 71.9 ± 13.7%, %TWL – 38.6 ± 8.5%, and %EBL – 75.6 ± 14.9%.
However, the highest effectiveness was observed in the Soft group, where weight reduction reached 106.9 ± 21.1% for %EWL, 49.5 ± 8.9% for %TWL, and 114.2 ± 22.1% for %EBL, which significantly exceeded the results in both other groups (p<0.001).
Weight regain, defined as a deterioration in BMI category compared to the 12-month result, was recorded in 62.4% (232 out of 372) of patients in the Classic group, 24.7% (102 out of 413) in the Hard group, and 30.3% (123 out of 406) in the Soft group.
The most stable long-term weight maintenance outcomes were observed in the Hard group (75.3%), while the Soft group demonstrated a stability rate of 69.7%, significantly higher than that of the Classic group (37.6%, χ²=80.5; p<0.0001), but not statistically different from the Hard group (χ²=3.22; p=0.073).
When patients were categorized by BMI at 12–36 months postop,
20.4% of patients in the Classic group achieved ideal weight,
compared to 59.3% in the Hard group and 46.1% in the Soft group.
The proportion of patients with grade 2–3 obesity was highest in the Classic group (25.0%), whereas it was substantially lower in the Hard and Soft groups — 6.8% and 9.6%, respectively.
Statistically significant differences were found among all three groups (Classic vs. Hard: χ²=133.9; p<0.0001; Hard vs. Soft: χ²=16.4; p=0.0007; Classic vs. Soft: χ²=72.9; p<0.0001) see [Table 1].
A supplementary analysis assessed weight regain between 12 and 36 months among patients who experienced a reversal in obesity status — i.e., transitioned to a higher BMI category (e.g., from normal weight to overweight or from grade I to grade II obesity).
This approach allowed an objective evaluation of the degree of metabolic “rebound” after reaching maximum weight loss.
In the Classic group, the average decrease in previously achieved %EWL was 28.9 ± 20.2%, comparable to the Hard group (30.2 ± 18.9%; p=0.523) and not significantly different from the Soft group (32.9 ± 23.4%; p=0.094).
A similar trend was observed for %EBL, with decreases of 30.7 ± 22.2% (Classic), 31.9 ± 20.5% (Hard; p=0.632), and 35.3 ± 25.8% (Soft; p=0.095), none of which reached statistical significance.
The proportion of patients with grade 2–3 obesity was highest in the Classic group (25.0%), whereas it was substantially lower in the Hard and Soft groups — 6.8% and 9.6%, respectively.
Statistically significant differences were found among all three groups (Classic vs. Hard: χ²=133.9; p<0.0001; Hard vs. Soft: χ²=16.4; p=0.0007; Classic vs. Soft: χ²=72.9; p<0.0001) see [Table 1].
A supplementary analysis assessed weight regain between 12 and 36 months among patients who experienced a reversal in obesity status — i.e., transitioned to a higher BMI category (e.g., from normal weight to overweight or from grade I to grade II obesity).
This approach allowed an objective evaluation of the degree of metabolic “rebound” after reaching maximum weight loss.
In the Classic group, the average decrease in previously achieved %EWL was 28.9 ± 20.2%, comparable to the Hard group (30.2 ± 18.9%; p=0.523) and not significantly different from the Soft group (32.9 ± 23.4%; p=0.094).
A similar trend was observed for %EBL, with decreases of 30.7 ± 22.2% (Classic), 31.9 ± 20.5% (Hard; p=0.632), and 35.3 ± 25.8% (Soft; p=0.095), none of which reached statistical significance.
However, a significant advantage of the Hard group was revealed
in total weight loss (%TWL): 15.1 ± 7.3% vs. 13.2 ± 6.7% in the Classic
group (p=0.030), whereas the comparison with the Soft group (14.3 ±
7.9%) showed no significant difference (p=0.468).
Analysis of weight regain (%) among relapsing patients showed significantly greater increases in the Hard group (32.3 ± 15.1%) than in the Classic (25.2 ± 11.8%; p<0.001) and Soft groups (28.3 ± 15.3%; p=0.047). The difference between the Soft and Classic groups (3.1%) was borderline significant (p=0.058).
Thus, despite similar %EWL and %EBL values among regressing subgroups, the Hard group demonstrated the greatest weight regain and marked reduction in long-term outcome stability.
In the main group (Soft), where a refined LSG technique was combined with a comprehensive complication prevention program, the lowest total rate of postoperative complications was achieved — 26.85%, significantly lower than in the Hard group (49.39%; p<0.001) and much lower than in the Classic group (35.22%).
The Clavien-Dindo Classification (CDC) is a system for classifying
Analysis of weight regain (%) among relapsing patients showed significantly greater increases in the Hard group (32.3 ± 15.1%) than in the Classic (25.2 ± 11.8%; p<0.001) and Soft groups (28.3 ± 15.3%; p=0.047). The difference between the Soft and Classic groups (3.1%) was borderline significant (p=0.058).
Thus, despite similar %EWL and %EBL values among regressing subgroups, the Hard group demonstrated the greatest weight regain and marked reduction in long-term outcome stability.
In the main group (Soft), where a refined LSG technique was combined with a comprehensive complication prevention program, the lowest total rate of postoperative complications was achieved — 26.85%, significantly lower than in the Hard group (49.39%; p<0.001) and much lower than in the Classic group (35.22%).
The Clavien-Dindo Classification (CDC) is a system for classifying
surgical complications based on the type of intervention required
to address them. It’s a widely used system in the field of surgery to
categorize complications, from minor deviations from the standard
to life-threatening events and even death. The CDC system provides a
standardized way to report and compare the severity of complications
across different surgical procedures and settings[11].
According to the Clavien-Dindo classification,the Soft group had the most favorable complication profile:
Grade II complications occurred in only 2.46%, Grade III in 9.11%, and there were no fatal outcomes (Grade V).
In contrast, the Hard group showed Grade II and III complications in 15.90% and 19.52% of cases, respectively, with a mortality rate of 0.48%.
In the Classic group, these figures were 3.75%, 10.99%, and 0.27%, respectively.
Based on the analysis of postoperative weight dynamics, it was observed that during the first 12 months after surgery, the best results in terms of weight and BMI reduction were achieved in the Hard group, where body weight decreased from 132.4 ± 29.3 kg to 62.1 ± 12.3 kg, and BMI from 47.2 ± 6.9 kg/m² to 22.4 ± 3.8 kg/m² (p<0.0001 compared to the Classic group).
However, the main group (Soft) also showed notable outcomes: body weight decreased from 134.8 ± 27.4 kg to 64.2 ± 13.7 kg, and BMI from 47.4 ± 7.3 to 23.2 ± 3.9 kg/m² (p<0.0001), which is comparable to the Hard group but with a lower risk of complications.
In terms of excess weight loss metrics (EWL, TWL, EBL), the Soft group held an intermediate yet stable position, showing %EWL of 70.1 ± 14.9%, %TWL of 37.1 ± 8.7%, and %EBL of 74.2 ± 15.1% at 12 months post-op. These values significantly exceeded those of the Classic group (p<0.05) and were only slightly lower than those of the Hard group, again accompanied by a lower complication rate.
An analysis of BMI indicators over the 12–36 month period demonstrated that the Soft technique provides more stable weight control compared to the Classic group.
The proportion of patients maintaining normal body weight was 46.1% in the Soft group, compared to only 20.4% in the Classic group (p<0.0001). In the Hard group, this rate was higher (59.3%) but accompanied by more pronounced fluctuations in body weight among some patients.
According to the Clavien-Dindo classification,the Soft group had the most favorable complication profile:
Grade II complications occurred in only 2.46%, Grade III in 9.11%, and there were no fatal outcomes (Grade V).
In contrast, the Hard group showed Grade II and III complications in 15.90% and 19.52% of cases, respectively, with a mortality rate of 0.48%.
In the Classic group, these figures were 3.75%, 10.99%, and 0.27%, respectively.
Based on the analysis of postoperative weight dynamics, it was observed that during the first 12 months after surgery, the best results in terms of weight and BMI reduction were achieved in the Hard group, where body weight decreased from 132.4 ± 29.3 kg to 62.1 ± 12.3 kg, and BMI from 47.2 ± 6.9 kg/m² to 22.4 ± 3.8 kg/m² (p<0.0001 compared to the Classic group).
However, the main group (Soft) also showed notable outcomes: body weight decreased from 134.8 ± 27.4 kg to 64.2 ± 13.7 kg, and BMI from 47.4 ± 7.3 to 23.2 ± 3.9 kg/m² (p<0.0001), which is comparable to the Hard group but with a lower risk of complications.
In terms of excess weight loss metrics (EWL, TWL, EBL), the Soft group held an intermediate yet stable position, showing %EWL of 70.1 ± 14.9%, %TWL of 37.1 ± 8.7%, and %EBL of 74.2 ± 15.1% at 12 months post-op. These values significantly exceeded those of the Classic group (p<0.05) and were only slightly lower than those of the Hard group, again accompanied by a lower complication rate.
An analysis of BMI indicators over the 12–36 month period demonstrated that the Soft technique provides more stable weight control compared to the Classic group.
The proportion of patients maintaining normal body weight was 46.1% in the Soft group, compared to only 20.4% in the Classic group (p<0.0001). In the Hard group, this rate was higher (59.3%) but accompanied by more pronounced fluctuations in body weight among some patients.
The rate of weight regain after two years of follow-up was lowest
in the Hard group (24.7%), slightly higher in the Soft group (30.3%),
and highest in the Classic group (62.4%) (p<0.001).
However, in the Soft group, the extent of weight regain was less pronounced: weight gain averaged 28.3 ± 15.3% compared to 32.3 ± 15.1% in the Hard group, and the decrease in achieved %EWL was 32.9 ± 23.4% versus 30.0 ± 19.0% (p>0.05).
Similar comparative researches were held in several institutions such as National Institute of Diabetes and Digestive and Kidney Diseases and the bulletted findings mentioned below were from the same study[10]
However, in the Soft group, the extent of weight regain was less pronounced: weight gain averaged 28.3 ± 15.3% compared to 32.3 ± 15.1% in the Hard group, and the decrease in achieved %EWL was 32.9 ± 23.4% versus 30.0 ± 19.0% (p>0.05).
Similar comparative researches were held in several institutions such as National Institute of Diabetes and Digestive and Kidney Diseases and the bulletted findings mentioned below were from the same study[10]
• Most participants maintained their weight loss. Three to
7 years after surgery, participants who had gastric bypass
surgery regained an average of 3.9 percent of their body
weight, and participants who had gastric band surgery
regained on average of 1.4 percent of their body weight.
• High cholesterol was less common after gastric bypass and gastric band surgery.
• Diabetes and high blood pressure were less common after gastric bypass surgery. Over time, diabetes reoccurred in some patients, but numbers of new cases were low.
• Alcohol use disorders increased after gastric bypass surgery but not after gastric band surgery.
• Pain and physical function improved after bariatric surgery.
Although gastric sleeve is now the most common type of bariatric surgery, it was less common when the LABS study took place. Outcomes for gastric sleeve surgeries are not included in the results.
• High cholesterol was less common after gastric bypass and gastric band surgery.
• Diabetes and high blood pressure were less common after gastric bypass surgery. Over time, diabetes reoccurred in some patients, but numbers of new cases were low.
• Alcohol use disorders increased after gastric bypass surgery but not after gastric band surgery.
• Pain and physical function improved after bariatric surgery.
Although gastric sleeve is now the most common type of bariatric surgery, it was less common when the LABS study took place. Outcomes for gastric sleeve surgeries are not included in the results.
Conclusion
These findings confirm the advantages of the proposed modified
(Soft) technique, which combines anatomically precise dissection
preserving the incisura angularis and formation of a stable gastric
sleeve lumen, along with a comprehensive perioperative program to
prevent metabolic complications.
This approach provides weight loss and maintenance outcomes comparable to those of the Hard group, while significantly reducing the frequency of surgical, metabolic, and psychological complications.
This approach provides weight loss and maintenance outcomes comparable to those of the Hard group, while significantly reducing the frequency of surgical, metabolic, and psychological complications.