Journal of Obesity and Bariatrics
Download PDF
Case Report
*Address for Correspondence: Zvi Perry, MD, MA, Surgery ward A, Soroka University Medical Center, P.O.B 151, Beer-Sheva 85025, Israel E-mail: zperry1@gmail.com
Citation: Perry ZH, Glazer Y, Teich N, Atiass S, Rivin M, et al. Why do Patients who Underwent Laparoscopic Adjustable Gastric Banding Surgery, Decide to Remove their Band, a Retrospective Cohort Study. J Obes Bariatrics. 2015;2(2): 5.8.
Copyright © 2015 Perry ZH, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Obesity and Bariatrics | ISSN: 2377-9284 | Volume: 2, Issue: 2
Submission: 20 November 2015| Accepted: 11 December 2015 | Published: 16 December 2015
Why do Patients who Underwent Laparoscopic Adjustable Gastric Banding Surgery, Decide to Remove their Band, a Retrospective Cohort Study
Zvi H. Perry1,2*, Yair Glazer1, NadavTeich4, Shahar Atiass1, Michael Rivin1, Solly Mizrahia3 and Eliezer Avinoh1
- 1Surgery Ward A, Soroka University Medical Center, Beer-Sheva, Israel
- 2Department of Epidemiology and Health Services Evaluation, Ben-Gurion University of the Negev, Beer-Sheva, Israel
- 3Head Surgery Ward A, Soroka University Medical Center, Beer-Sheva, Israel
- 4Thoracic Surgery Ward, Beilinson Hospital, Israel
*Address for Correspondence: Zvi Perry, MD, MA, Surgery ward A, Soroka University Medical Center, P.O.B 151, Beer-Sheva 85025, Israel E-mail: zperry1@gmail.com
Citation: Perry ZH, Glazer Y, Teich N, Atiass S, Rivin M, et al. Why do Patients who Underwent Laparoscopic Adjustable Gastric Banding Surgery, Decide to Remove their Band, a Retrospective Cohort Study. J Obes Bariatrics. 2015;2(2): 5.8.
Copyright © 2015 Perry ZH, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Obesity and Bariatrics | ISSN: 2377-9284 | Volume: 2, Issue: 2
Submission: 20 November 2015| Accepted: 11 December 2015 | Published: 16 December 2015
Abstract
Background: Obesity is becoming more and more prevalent in western society. It is estimated that obesity will become a serious burden to society in the next century. Surgery has been shown to be the most effective method for treating morbid obesity. Laparoscopic gastric banding (LGB) is a common restrictive type of bariatric surgery in Israel. Despite the success of the surgery, some patients choose after a period of time to remove the band.Objective: To map the characteristics of LGB patients who chose to remove the band without an objective medical reason. In addition, to assess the rate of complications, quality of life and degree of weight loss among patients who decided to remove the band in comparison to patients who didn’t remove the band.
Methods: A retrospective case - control study among patients who underwent LGB surgery in Surgery ward A at the Soroka Medical center. We have recruited 360 patients to the study, who were operated in the years 2006-2011. Patients who chose to remove the band were compared to patents who did not remove it. Data was collected from the hospital computerized patient data system. In addition a telephone interview was completed at least two years after the band placement, and at least a year after its removal in the cases group. Demographic and physiological data were collected. A quality of life assessment was performed by a Bariatric Analysis and Reporting Outcome System (BAROS) questionnaire.
Results: The group of patients that removed the band where older and had the band for a longer period on average. Weight and BMI on the day of the interview was distinctly higher in the band removal group, which were at least a year after removal of the band. However the total weight lost, lowest weight and minimal BMI reached did not differ between the two groups. Immediate and long term complications rates were higher with the band removers. The leading reasons stated by the patients for band removal were: frequent vomiting, eating discomfort and band-related complications.
Conclusions: Band removers were not found to be different from non-removers pre-band characteristics or general surgical result. Two main differences were noted: the removal group had a higher rate of complications, and secondly the subjective feeling of intolerance to the band was stated as the main reason for band removal. Given these findings we learn about the importance of the band effect on the patient’s quality of life. A Patient who does not adjust to the band’s effects on quality of life is prone to remove it, even though the band fulfills its main role of weight loss. We recommend improving patient preparation and support before and after the operation by a multidisciplinary team designed to help the patient adjust to life with the band.
Keywords
Laparoscopic adjustable gastric banding surgery; Morbid obesity; Bariatric surgeryBackground
Morbid Obesity is a worldwide epidemic, and is believed to become the largest public health burden of the 21st century [1]. Obesity has been found associated with varied illness states, including HTN, diabetes, OSA, IHD and cancer [2-5]. The usage of diet, weight reduction medications, eating habit modifications or pharmacotherapy has been found to be inefficient, while surgical treatment is considered the only proven treatment to reduce and maintain the weight loss [6] in short and long term [7]. Surgical treatment is the recommended therapy for obese patients who are BMI 40 and higher, or for patients with BMI 35 and co-morbid related illnesses. One surgical solution is the Laparoscopic gastric banding (LGB), which is a minimal invasive procedure, considered to be strictly a restrictive operation, and has been found to be a safe and efficient treatment for the long term morbidly obese patient [8]. The mortality of this procedure is low (0.1%), and it is able to lower 50% of the excess body weight [9]. LGB patients show a dramatic improvement in co-morbid illness of obesity, like HTN, diabetes and dyslipidemia. Morbidity includes LGB slippage (movement of the band from its original place), Erosion (the band is eroding the stomach due to repeated movement of the band) and band malfunction (mainly a leakage of the substance used to inflate the band) [10,11].Due to complications like these, some patients decide upon removal of the band, and in the current study we have tried to evaluate this sub-set of patients who decided to remove their band entirely, even though they had no medical indication for this. We have defined medical indication for band removal as one of 3 situations - Band erosion, Band infection and band malfunction. Thus, our study population included patients who had their bands removed not due to these situations.
Due to the fact we are today the leading center in Israel who uses LGB, it was only logical that we will try to understand this phenomena and these patients.
Patients and Methods
Between the years 2000-2011 a single team of surgeons had operated on over 8000 morbid obese patients. We have used a retrospective case-control study design, in which the cases were patients who were operated upon by our surgical team and decided to remove their band, with no medical indication (i.e., - no erosion, no indication of band infection, etc.). Our control group was patients who were operated upon by our surgical team and did not remove their band in the study period. One must stress that due to our large coverage of Israel, we were able to reach most of our patients, and thus we believe that our sample is truly representative of our population.Procedure
The study was evaluated and approved by the local ethics committee. Patients’ demographics, surgical procedure duration and outcomes including short and long term complications were gathered through our computerized data base. Using clinic interviews patients’ current status (weight, height etc.) as well as evaluation of their quality of life through our pre-formed questionnaire was evaluated.
Survey content
The study included the two groups of patients which filled out a self-administered questionnaire, including the BAROS questionnaire which is considered the standard questionnaire for bariatric operations [12]. The questionnaire concerned personal data (age, gender, family status etc.), eating and drinking habits, quality of life aspects (ability for physical activity), daily activities (like dressing, shop for clothing), self-esteem, (satisfaction of sexual activity etc.) and finally weight and height before the surgery and in the present.
Data gathering and storage
Data was gathered, coded and stored using SPSS software (SPSS 18.0, Chicago, IL, USA).
Statistical analysis
We analyzed the data using descriptive and analytical statistics: independent samples t test, one way ANOVA and χ2. We also used a-parametric analysis when applicable. Statistical significance was considered when p< 0.05.
Results
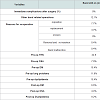
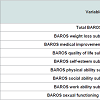
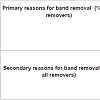
Our records show that in the period our study was conducted 509 patients underwent band removal. The reasons for band removal were variable including removal due to erosion (46 patients 9.1%), slippage (51 patients 10.1%), and band intolerance (75 or 14.9%). The most common reason was band replacement (262 or 51.9%). Thus, true removal of the band was only performed in 247 of our patients. If we consider removal of the band due to medically indicated reason, we find that 351 cases were medically indicated (73.6%), and only 126 cases (26.4%) were lacking a sound medical indication. After grouping we found that 15% of the removal cases were due to a known intolerance (75 cases). Of those 64 were recruited to our study, which means that 85% of the patients who suffered from intolerance were recruited to our study. If we consider the fact that in that decade the number of patients who underwent LGB surgery with our surgical teams is close to 8000 cases, the intolerance rate is less than 1%.From the patients who had their band removed we created the study group, and from patients who did not elect to remove the band we randomly sampled patients using a simple random sampling procedure. Thus, our study population included 360 patients, of them 272 were still with the band upon the time in which the study was conducted (76%). 24 of the patients had partial information or followup and thus were omitted from data analysis. The compliance to be in the study was 73% in patients who removed the band (study group) and 100% with the patients who were still with the band (control group). 93 Of the study patients were males (25.8%). Demographical and weight data are summarized in Table 1. Our results have shown that the patients who elected to remove the band were older, and on the average were for longer periods with the band. Looking at the weight and the BMI at the day of the interview one can see a significant difference between the groups, in which those who elected to remove the band were higher in both aspects. But, if we look at the excess weight the two groups lost, or the lowest weight attained while still on the band (both a factor of measuring the success of the operation), we have found no significant difference between the groups.Table 2 shows the pre and post-op morbidity of our subjects, as well as complications - one can see from this table that long term complications in those who removed the band were higher, except band malfunction which was more frequent in the control group. From this table also stems a significant difference between the background illnesses of the subjects, and that the band removers were more frequently suffering from them.When considering issues of quality of life, as measured by the BAROS scale (see Table 3), we have seen that even though the total BAROS score did not differ between the groups, sub-scales like selfesteem, social interaction and work ability were significantly elevated in band removers.This led us to our questions about the specific reasons which led band removers to remove their bands, as depicted in Table 4.We asked our patients open ended questions about their main reason to remove the band, as well as any secondary reasons that led them to this decision. Our subjected have named band intolerance as the primary cause for removing the band (49% of our patients have stated this to be the main and primary cause of band removal).
The second most frequent reason for band removal was band complications (mainly slippage), which was the primary cause in 41% of the patients.
We also asked our patients about secondary reasons for band removal, and amongst patients who depicted other reason except intolerance as their primary reason for band removal, 47% of the patients depicted band intolerance to be the cause.
Discussion
Our results have shown us that both the study and the control groups are quite similar in most aspects, even though the band removers were a bit older (4 years in average, p=0.014). This difference can be explained in part by the fact that band removers were a longer time with the band (p< 0.001, on the average they had the band for 2.7 years longer).Looking at background illnesses one can see a similar trend - band removers were more likely to suffer from HTN (p=0.03, 23% in the control group vs. 36% in the band removers), OSA (p< 0.001, 7% in the control vs. 24% in the band removers), and lung problems like COPD or Asthma (p< 0.001, 12% vs. 45% in the band removers). These findings are of interest to us, because even though these patients were generally sicker than the control group, and thus more likely to benefit from the operation [11], they still elected to remove their band.
On the other hand, we did not find any difference between the groups after surgery in their health status, which means they actually did benefit from the operation as their counterparts, which means that the explanation of a lesser degree of benefit - either before or after operation, is not a feasible explanation for why they decided toremove the band.
The same applies for weight and BMI - the groups were similar pre-op in these aspects and their BMI and weight loss were not different significantly, which means that more obese patients are not more prone to remove their band, or that weight loss difference is the cause for deciding to remove the band.
On the other hand, upon the day of the interview the weight and the BMI did differ significantly (p< 0.001), while for those with band the current average weight was 86±19 kg and an average BMI of 31 (±6), in the band removers average weight rose to a 100 (±23) kg with an average BMI of 36 (±7). If considering the weight loss until the day of the interview, one can see that band removers lost from their initial weight 21 (±2.8) kg with an average BMI reduction of 7.3 (±7.7), whereas the control group has lost on average 34 (±2) kg, with an average BMI reduction of 12.2 (±6.5) (p< 0.001). Our data has shown that the control and the research group had similar weight loss as long as both had the band on, and thus we can conclude that the changes above stem from weight gain after the band has been removed.
This means that the common belief seen in band removers that they have learned to control their eating habits (an issue we surveyed in a previous article in JOAB) is wrong, and as long as they had the band they were able to maintain a significant weight loss, which disappears when the band is removed, as seen also in other studies[13].
Our data has shown a significant difference in the post-op complications between the 2 groups.
We have seen that patients who had a higher complications rate were more prone to elect to remove their band, and it seems logical to assume that frequent hospitalization and re-operations have an impact upon our patients’ decisions to remove the band.
But, the patients themselves do not think so, and they did not explain their decision to remove the band due to surgical complications, as the primary cause.
One reservation that must be announced is that our patients who decided not to remove their bands were bothyounger and with a shorter time with the band, and thus our explanation above is flawed, and all we see is age related.
As seen in Table 4, we did not find any differences in the quality of life, or other measures depicted by the BAROS, between the two groups, which means that those who elected to remove the band “enjoyed” the same benefits as those in the control group. This seems odd if we recall that patients stated that the main reason for their decision to remove the band was band intolerance, and thus we surveyed each sub scale of the BAROS, and found that patients who elected to remove their band were on the average with lower self-esteem, but with better social and work connections. This might imply a less mature personality that tends to idealize and have unrealistic expectations from the band, which leads to a faster tendency to remove the band, a phenomena seen also in other studies [13].
If asking the patients themselves to explain why they decided to remove the band, the leading causes were - frequent vomiting, feeling less comfortable while eating and surgical complications. Much has been written upon surgical complications like erosion [12], or band slippage [14], but a lot less was written about band intolerance, even though researchers believe this is an important aspect to why people decide to remove their band [13].
The current study has found that the main reasons for band removal could be attributed to band intolerance and not to band complications, as was commonly believed. It seems that success in maintaining weight loss after bariatric surgery requires the ability to implement longterm changes in eating habits and lifestyle, and those who are unable to do so seem to be more prone to decide upon removal of the band. Although general guidelines exist, individual monitoring and tailoring are frequently required. This has been shown vividly in our study in which a large variance was found in many issues, but we do believe that a main theme does exist and should be implemented in guidelines that should be common knowledge to all bariatric surgeons alike.
Study limitations
Today more and more people opt to remove their band, and the numbers shown in this study might be an underestimation. This stems from the fact that patients might opt to remove the band in other medical facilities in Israel, but our experience with these patients have shown us that even if they decide to remove their band they have a tendency of doing so in our institution due to the long follow-up we have with these patients.
Our study is case-control in its’ design, which is a study design more prone for biases like information and selection bias, and it would be better if this study would have been conducted in a cohort study design, but time and financial issues prevented us from this.
Another limitation is the length and timing of the study - We did not see in the years of the study any trend of more band removers, but in the last 2 years as sleeve has become more and more prevalent in Israel, we did see a rise in the number of band removers, but these number and patients were not included in the study period, and thus no formal conclusion can be met about patients these days. Our records have also shown an annual rate of band removal, which shows a steady rise from 50 cases a year to 100 or so cases yearly in the ending years of our study period.
Conclusions
The current study has shown that the patients who elected to remove their bands did not differ upon background characteristics, or in their post-op surveillance. They did differ in post-op surgical complications which were more frequent in those who removed the band, and more importantly in a subjective feeling of incompetence with the band which lead them to decide to remove the band. This finding highlights the importance of our patients quality of life - a patient that has a problem adjusting to the band is more prone to decide to remove it, even if the band fulfills its’ main purpose which is weight reduction. This leads us to believe that a better surveillance and guidance with a multi-disciplinary team, which will aid our patients to adjust to the band, might lead to lower attrition with the band.References
- Choi BC, Hunter DJ, Tsou W, Sainsbury P (2005) Diseases of comfort: primary cause of death in the 22nd century. J Epidemiol Community Health 59: 1030-1034.
- Percik R, Stumvoll M (2009) Obesity and cancer. Exp Clin Endocrinol Diabetes 117: 563-566.
- Ziyab AH, Karmaus W, Kurukulaaratchy RJ, Zhang H, Arshad SH (2014) Developmental trajectories of Body Mass Index from infancy to 18 years of age: prenatal determinants and health consequences. J Epidemiol Community Health 68: 934-941.
- Borgeraas H, Hertel JK, Svingen GF, Seifert R, Pedersen EK, et al. (2014) Association of body mass index with risk of acute myocardial infarction and mortality in Norwegian male and female patients with suspected stable angina pectoris: a prospective cohort study. BMC Cardiovasc Disord 14: 68.
- Lavie CJ, Milani RV, Ventura HO (2009) Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 53: 1925-1932.
- Sundbom M, Gustavsson S (2004) Bariatric surgery. Clin Dermatol 22: 325-331.
- De Palma GD, Forestieri P (2014) Role of endoscopy in the bariatric surgery of patients. World J Gastroenterol 20: 7777-7784.
- Breznikar B, Dinevski D (2009) Bariatric surgery for morbid obesity: pre-operative assessment, surgical techniques and post-operative monitoring. J Int Med Res 37: 1632-1645.
- Sultan S, Parikh M, Youn H, Kurian M, Fielding G, et al. (2009) Early U.S. outcomes after laparoscopic adjustable gastric banding in patients with a body mass index less than 35 kg/m2. Surg Endosc 23: 1569-1573.
- Navarra G, Musolino C, Centorrino T, De Marco ML, Sarra G, et al. (2009) Perforation of an adjustable gastric banding connecting tube into distal transverse colon with intra-luminal migration. Obes Surg 19: 125-127.
- Yin J, Hou X (2014) Complications of laparoscopic versus open bariatric surgical interventions in obesity management. Cell Biochem Biophys 70: 721-728.
- Oria HE, Moorehead MK (2009) Updated Bariatric Analysis and Reporting Outcome System (BAROS). Surg Obes Relat Dis 5: 60-66.
- Fischer L, Nickel F, Sander J, Ernst A, Bruckner T, et al. (2014) Patient expectations of bariatric surgery are gender specific--a prospective, multicenter cohort study. Surg Obes Relat Dis 10: 516-523.
- Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G (2013) Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol 62: 569-576.