Journal of Neurology and Psychology
Download PDF
Special Issue: Clinical Neuropsychology
Research Article
*Address for Correspondence: Leonard A. Jason, Center for Community Research, DePaul University, 990 W. Fullerton Ave., Chicago, IL 60614, USA, Tel: 773-325-2018; Fax: 773.325.4923; E-mail: ljason@depaul.edu
Citation: Jason L A, McManimen S, Sunnquist M, Brown A, Newton JL, et al. Examining the Institute of Medicine’s Recommendations Regarding Chronic Fatigue Syndrome: Clinical Versus Research Criteria. J Neurol Psychol. 2015; S(2):8.
Copyright © 2015 Jason LA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology and Psychology | ISSN: 2332-3469 | Special Issue: 2
Submission: 16 September 2015 | Accepted: 20 November 2015 | Published: 25 November 2015
Editors: Dr. David AS Kaufman, Assistant Professor of Psychology Saint Louis University, USA
Research Article
Examining the Institute of Medicine’s Recommendations Regarding Chronic Fatigue Syndrome: Clinical Versus Research Criteria
Leonard A. Jason1*, Stephanie McManimen1, Madison Sunnquist1, Abigail Brown1, Julia L.Newton2, and Elin Bolle Strand3
- 1Center for Community Research, DePaul University, 990 W.Fullerton Ave., Chicago, IL 60614, USA
- 2Newcastle University, Newcastle upon Tyne, Tyne and Wear NE17RU, UK
- 33Oslo University Hospital, Sognsvannsveien 20, 0372 Oslo, Norway
*Address for Correspondence: Leonard A. Jason, Center for Community Research, DePaul University, 990 W. Fullerton Ave., Chicago, IL 60614, USA, Tel: 773-325-2018; Fax: 773.325.4923; E-mail: ljason@depaul.edu
Citation: Jason L A, McManimen S, Sunnquist M, Brown A, Newton JL, et al. Examining the Institute of Medicine’s Recommendations Regarding Chronic Fatigue Syndrome: Clinical Versus Research Criteria. J Neurol Psychol. 2015; S(2):8.
Copyright © 2015 Jason LA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology and Psychology | ISSN: 2332-3469 | Special Issue: 2
Submission: 16 September 2015 | Accepted: 20 November 2015 | Published: 25 November 2015
Editors: Dr. David AS Kaufman, Assistant Professor of Psychology Saint Louis University, USA
Abstract
The Institute of Medicine (2015) has proposed a new clinical case definition for what had been known as chronic fatigue syndrome (CFS). This new criteria involved the following domains: substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities; postexertional malaise; unrefreshing sleep; and at least one of the two following symptoms: cognitive impairment or orthostatic intolerance. In addition, in August of 2015, the CFS Advisory Committee, which makes recommendations to the Secretary of US Department of Health and Human Services, proposed that the Canadian 2003 criteria should serve as the research case definition for CFS. Up to now, there have not been any published investigations comparing these clinical and research criteria. Using patient samples collected in the United States, Great Britain, and Norway, the current study compared and contrasted patients who met the clinical and research criteria. Overall findings indicated that those meeting the research criteria in comparison to those meeting the clinical criteria were significantly more impaired on a wide variety of symptoms and functional areas. The implications of these findings are discussed.Keywords:
Myalgic encephalomyelitis; Chronic fatigue syndromeCase definition
For the past 20 years, investigators around the world have used what is known as the Fukuda et al. criteria to define chronic fatigue syndrome (CFS) [1]. The Fukuda CFS criteria required a person to experience 6 or more months of chronic fatigue of a new or definite onset that is not substantially alleviated by rest and not the result of ongoing exertion. The fatigue must also result in substantial reductions in occupational, social, and personal activities. The Fukuda et al. CFS case definition used polythetic criteria: a set of symptoms in which all do not need to be present to make a diagnosis. Because these criteria require only four symptoms out of a possible eight, critical CFS symptoms, such as post-exertional malaise or memory and concentration problems, were not required for a patient to receive a diagnosis of CFS. This could have increased the heterogeneity of the population and complicated identification of comparable samples.
Because of these problems with the Fukuda et al. CFS criteria, the Institute of Medicine (IOM) proposed new clinical criteria for what had been known as CFS. The IOM criteria (which was called Systemic Exertion Intolerance Disease, SEID) included the following criteria: substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities; post-exertional malaise; unrefreshing sleep; and at least one of the two following symptoms: cognitive impairment or orthostatic intolerance [2]. There is considerable amount of empirical support for these four domains [3]. However, when Jason, Sunnquist, and Brown et al. analyzed archival samples from the USA, Great Britain, and Norway [4], findings indicated that the SEID IOM criteria identified 88% of participants in the samples analyzed, which was comparable to the 92% that met the Fukuda criteria. It is important to note that the samples selected in the Jason, Kot et al. [1] article had already been screened for exclusionary illnesses. Because the IOM criteria have few exclusionary conditions, when other data sets were examined that had other illness groups, a study by Jason, Sunnquist et al. found that the SEID IOM prevalence rate would be 2.8 times higher than when using the Fukuda et al. criteria [5]. This is of importance as the new SEID criteria could considerably broaden the prior CFS Fukuda et al. criteria, and this could make this classification system more heterogeneous.
In addition, the CFS Advisory Committee, which makes recommendations about CFS to the Secretary of the US Department of Health and Human Services, recommended that the Canadian Criteria become the research criteria [6,7]. In contrast to the prior Fukuda et al. criteria, this case definition specified core symptoms, including post-exertional malaise, impairment of memory and concentration, unrefreshing sleep, arthralgia and/or myalgia, and several autonomic, neuroendocrine, and immune manifestations. In addition, rather than 4 primary symptoms that had been recommended by the IOM’s SEID criteria, the Canadian criteria required at least 7 core symptoms, and considerable research had been conducted over the past decade with the Canadian criteria. For example, one study examined the Canadian criteria [6] in contrast to the Fukuda et al. criteria [1]. In that study, Jason, Torres-Harding, Jurgens, and Helgerson found that the Canadian criteria [8], in contrast to the Fukuda et al., criteria selected cases with less psychiatric comorbidity, more physical functioning impairment, more fatigue or weakness, and more neuropsychiatric and neurological symptoms. Comparable findings emerged elsewhere [9]. In another study, Jason, Brown, Evans, Sunnquist, and Newton also found that about 87 to 96% of patient samples recruited through different methods met the Fukuda et al. case definition criteria, whereas only 73 to 77% met the Canadian ME/CFS criteria [10].
There has been some recent research that has compared the IOM [2] criteria to the Canadian criteria [7]. This is of importance because if there are to be two groups of patients to be identified by clinicians and scientists, we do need to know how these two groups of patients differ. One recent study examined the percent of individuals meeting different criteria from studies with varying case ascertainment methods [11]. Based on data from that study, 88% of patients met the IOM [2] criteria, whereas 76% met the Canadian criteria [7]. That study suggests that within more tertiary care settings, or when patients have self-identified as having ME or CFS, it appears that more individuals meet the IOM criteria. However, that study did not examine sociodemographic, symptom and functional differences between these clinical and research criteria. The present study is the first to compare the clinical criteria as defined by the SEIDIOM to IOM [2] and contrasted this with the research criteria as specified by the Canadian criteria on a wide variety of demographic, symptom, and functional measures. We hypothesized that the research criteria would identify a more impaired group. Many believe this illness to be neurologically-based, so identifying the proper assessment with such a comparison would be of importance to the field of clinical neuropsychology. Determining the criteria for a more homogenous, impaired group of patients may allow scientists to find appropriate treatment interventions. At the present time, we do not know how clinical and research criteria differentiate patients who are identified in clinical practice as well as research settings.
Methods
Research participantsDePaul sample: An international convenience sample of adults self-identifying as having CFS, ME/CFS, or ME was recruited. To be eligible, an individual needed to be at least 18, capable of reading and writing English, and have a self-reported, current diagnosis of ME, CFS, or ME/CFS. Following approval from DePaul University’s Institutional Review Board, participants were recruited from a variety of sources: postings on internet forums, support group visits, recontacting individuals who had participated in the DePaul research team’s studies in the past, and contacting individuals who hademailed the team in the past with interest in future studies.
Participants were given three options for completing study measures: an electronic survey, a hard-copy survey, or a verbal survey over the telephone. All participants were given the opportunity to complete these surveys at home or in person at DePaul University. Participants were not given a timeline for survey completion, as this illness can be unpredictable and result in a rapid decline of functioning on any given day. The first one hundred individuals who completed the survey received a $5.00 gift card to Amazon.com for their participation. Of the 217 individuals who participated, 216 were included in the present study; one participant was excluded due to incomplete data.
Demographically, the sample was 84.2% female and 15.8% male. This sample was predominantly (97.7%) Caucasian, while 0.5% identified as Asian, and the remaining 1.9% selected ‘Other’ as their race. Only 13.5% of the sample was working full- or part-time, and 56.7% of the sample was on disability. With regard to educational level, 40.5% of the sample held a graduate or professional degree; 34.4% held a standard college degree; 18.1% had attended college for at least one year; and 7.0% completed high school or had a GED. The mean age of the sample was 52.0 (SD = 11.3).
SolveCFS BioBank sample: A separate sample of individuals was collected by the Solve ME/CFS Initiative. This patient data originated from the SolveCFS BioBank, a resource with clinical information and blood samples on a population of individuals diagnosed by a licensed physician specializing in CFS, ME/CFS, and ME. The sample used in the present study included only those over 18. Participants were recruited by the Solve ME/CFS Initiative through physician referral. All participants who met eligibility criteria completed a written informed consent process. Participants completed the study measures electronically or by hard copy. The data were de-identified and shared with the DePaul research team following submission and peer review of a research protocol to the Solve ME/CFS Initiative.
Of the 239 patients who participated, 99.2% were Caucasian, and 0.8% were Asian or Pacific Islander. With regards to gender, 73.1% of the sample was female. Only 10.5% of the sample was working fullor part-time, with 65.3% on disability. Regarding education level, 24.7% of the sample held a graduate or professional degree; 42.3% had completed college; 20.5% had completed some college; and 11.3% had a high school degree or GED. The average age of the sample was 49.7 (SD = 12.9).
Newcastle sample: Participants in the Newcastle sample had been referred for a medical assessment at the Newcastle-upon-Tyne Royal Victoria Infirmary clinic due to a suspected diagnosis of CFS. An experienced physician performed a comprehensive medical history and examination, and individuals who met eligibility criteria completed a written informed consent process. A total of one hundred participants completed study measures by hard copy, but three were excluded due to incomplete data.
The Newcastle sample was 99.0% Caucasian and 1.0% multiracial,and 82.5% of participants were female. Of this sample, 37.5% of participants were working either part- or full-time, and 30.2% were on disability. With regard to education level, 20.9% had a graduate or professional degree; 29.7% had a college degree; 24.2% had completed at least one year of college; 14.3% had a high school degree; and 11.0% had not completed high school. The average age of the sample was 45.6 (SD = 14.0).
Norway sample 1: Individuals with CFS were invited to participate in a randomized controlled trial of a CFS self-management program. Participants were recruited from four mid-sized towns in southern Norway, two suburbs of Oslo, and some surrounding communities. Recruitment sources included: healthcare professionals, the waiting list for a patient education program, and CFS patient organizations. Information about the study was disseminated through brochures and personal communication. In addition, study announcements for participants were placed on the Oslo University Hospital website.
Participants were required to be older than 18 years of age and diagnosed with CFS by a physician or medical specialist. In addition, participants could not be pregnant and needed to be physically able to attend the self-management program. Those who were interested in participation were given additional information by telephone. Participants completed a consent form that provided permission to request confirmation of their CFS diagnosis from their physician or medical specialist. The study gained approval from the Regional Committee for Medical Research Ethics (Health Region North) and the Privacy Ombudsman for Research at Oslo University Hospital. Of the 176 participants, 175 were included in this study; one participant was excluded due to missing data.
This sample was 86.8% female and 13.2% male. Almost all participants were Caucasian (99.4%); one participant selected ‘Other’ when asked about race. Only 9.7% of participants were working, while 84.0% were on disability. Regarding education, 9.9% of participants had a graduate or professional degree, 40.1% a standard college degree, 41.9% a high school degree, and the remainder had not completed high school. The mean age of the sample was 43.4 years (SD = 11.7).
Norway sample 2: Participants were recruited from an inpatient medical ward for severely ill patients as well as from the outpatient clinic at a multidisciplinary CFS/ME Center. To be eligible for inclusion, participants needed to be between 18 and 65 years old and capable of reading and writing Norwegian. Individuals with a suspected diagnosis of CFS were referred for evaluation and completed the study measures. All participants took part in a comprehensive medical history interview and a detailed medical examination conducted by experienced consultant physicians and a psychologist. The examinations were conducted to rule out exclusionary medical and psychiatric conditions. Participants completed a written informed consent, and the study measures were completed by hard copy. The project gained approval from the Privacy Ombudsman for research at Oslo University Hospital. Of the 64 total participants, 63 were included in this study; one was excluded due to missing data.
This sample was 82.5% female and 17.5% male. The majority of the sample identified as Caucasian, but 1.6% identified as Asian, and 3.3% as ‘Other.’ Most participants (76.2%) were on disability, while 19.0% were working. With regard to education, 11.1% held a graduate or professional degree; 25.4% held a standard college degree; 46.0% had a high school degree; and 17.5% had not completed high school. The mean age of the sample was 34.9 years (SD = 11.6).
Measures
The DePaul Symptom QuestionnaireAll participants completed the DePaul Symptom Questionnaire (DSQ), a self-report measure of ME and CFS symptomatology, demographics, and medical, occupational and social history [12]. This measure was developed to classify individuals by a variety of ME and CFS case definitions, but the list of 54 symptoms was based upon a revised approach to the Clinical Canadian criteria [7]. Participants rate each symptom’s frequency over the past six months on a 5-point Likert scale: 0=none of the time, 1=a little of the time, 2=about half the time, 3=most of the time, and 4=all of the time. Likewise, participants rate each symptom’s severity over the past six months on a 5-point Likert scale: 0=symptom not present, 1=mild, 2=moderate, 3=severe, 4=very severe. Frequency and severity scores were multiplied by 25 to create 100-point scales. The 100-point frequency and severity scores for each symptom were averaged to create one composite score per symptom. The DSQ has evidenced good test-retest reliability among both patient and control groups [13]. A factor analysis of these symptoms resulted in a three-factor solution, and these factors evidenced good internal consistency [14]. The DSQ is available in the shared library of Research Electronic Data Capture (REDCap) [15], hosted at DePaul University: https://redcap. is.depaul.edu/surveys/?s=tRxytSPVVw.
Medical outcomes study 36-Item Short-Form Health Survey (SF-36 or RAND Questionnaire)
The SF-36 measures the impact of participants’ health on physical and mental functioning [16]. The measure results in eight subscales: Physical Functioning, Role Physical, Bodily Pain, General Health, Social Functioning, Mental Health, Role Emotional, and Vitality. Higher subscale scores indicate less impairment. The SF-36 evidences strong psychometric properties, including good internal consistency and discriminant validity [17].
Case definitions
IOM criteria: The IOM [2] clinical criteria were operationalized the following ways: substantial reductions in functioning as measured by meeting at least two of the three following criteria on the SF-36: Role Physical score ≤ 50, Social Functioning score ≤ 62.5, and Vitality score ≤ 35. Patients needed to have at least one post-exertional malaise item, which included: soreness after mild activity, drained/sick after mild activity, minimum exercise makes tired, muscle weakness, dead/ heavy feeling after exercise, and mentally tired after slightest effort. Neurocognitive items included: difficulty paying attention, difficulty expressing thoughts, problems remembering, absent-mindedness, can only focus on one thing at a time, slowness of thought, difficulty understanding, and difficulty paying attention. Orthostatic Intolerance was defined as either dizziness/fainting, shortness of breath, unsteady on feet, irregular heartbeats, or chest pain. To meet IOM criteria, patients had to have at least one neurocognitive or Orthostatic Intolerance item. Finally, patients needed to have at least one sleep dysfunction symptom, which included: unrefreshing sleep, problems staying asleep, problems falling asleep, waking up early, and need to nap daily. Frequency and severity criteria, as specified in the IOM, were employed.
Canadian case definition [7]: The Canadian Clinical criteria require a substantial reduction from premorbid functioning, six or more months of fatigue, and symptoms from at least six domains. To assess for substantial reduction in functioning, guidelines from previous research are applied; a participant needs to meet two of the following three criteria: an SF-36 Role Physical score less than or equal to 50, an SF-36 Social Functioning score less than or equal to 62.5, or an SF-36 Vitality score less than or equal to 35 [18]. To meet the fatigue requirement, participants need to report that they have experienced problems with fatigue or energy for six months or more. Additionally, participants must report symptoms of at least moderate severity (2 or greater on the DSQ Likert scale) that have occurred at least half of the time (2 or greater on the Likert scale) over the past six months from the following symptom domains: postexertional malaise (at least one symptom), sleep dysfunction (at least one symptom), pain (at least one symptom), and neurocognitive dysfunction (at least two symptoms). Finally participants must report at least one symptom of the same frequency and severity as above from two of the following three domains: autonomic dysfunction, neuroendocrine dysfunction, or immune dysfunction. Individuals with morbid obesity, lifelong fatigue, or medical or psychological conditions that could cause fatigue are precluded from meeting this case definition.
Statistics
We used a MANCOVA to examine whether the two samples were significantly different overall while controlling for age and education level. Tests of between-subject effects were used to determine if the two variables differed. The MANCOVA was conducted on the SF-36 and each symptom domain to reduce the risk of a Type 1 error that could result from conducting a series of one-way ANOVAs on each variable. A Fisher’s exact test was employed with categorical data.
Results
Demographic characteristicsOf the 795 patients in the study, 70.2% met both IOM and Canadian, 18.1% only met the IOM criteria, 11.1% met neither criteria, and 0.6% met the Canadian criteria but not the IOM criteria. The two groups examined in this study were the clinical IOM group, which are the patients that only met the IOM case definition (N=144, 18.1%), and the research Canadian group, which are the patients that either met only the Canadian criteria or met both Canadian and IOM case definitions (N=563, 70.8%). ( Table 1) provides a comparison of the demographic characteristics of the patients meeting each criteria. The clinical IOM was significantly older than the research Canadian groups, F(1, 699) = 4.29, p< .05. In addition, the IOM group had a significantly higher education level than the research Canadian group, [χ2 (1) = 8.87, p< .05]. No other demographic characteristics were significantly different, p> .05.
Mean composites: Table 2 provides a comparison of the mean and standard deviations and MANCOVA results of symptom and domain composites for patients meeting the two sets of criteria after controlling for age and education. The research group had significantly higher scores than the clinical group on all mean composite domain scores (p < .05). In addition, there were significant differences in individual symptoms with the exception of feeling drained/sick after mild activity, needing to nap daily, and difficulty paying attention. For each symptom, the group that met the Canadian criteria had higher scores than the group that only met the IOM criteria, which indicates the Canadian group experiences these symptoms more frequently and severely.
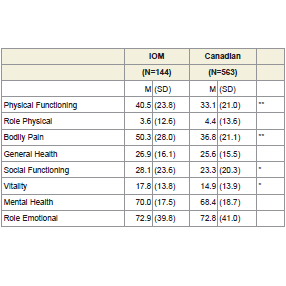
SF-36: Table 3 provides a comparison of the mean and standard deviations for patients meeting each criteria on the SF-36 subscales after controlling for age and level of education in a MANCOVA. The Canadian research group has significantly lower scores on the Physical Functioning, Bodily Pain, Social Functioning, and Vitality subscales indicating they have worse functioning compared to the patients that only met the clinical IOM criteria, p< .05.
Illness characteristics: Table 4 provides a comparison of illness characteristics between patients meeting the research and clinical criteria. The two groups significantly differed on the percentage of patients reporting frequent viral infections with prolonged recovery periods, [χ2 (1) = 5.87, p< .05], indicating that those meeting the Canadian research criteria experienced viral infections significantly more than the patients only meeting the clinical IOM criteria. No other characteristics reached statistical significance, p> .05.
Discussion
This is the first study to compare clinical criteria as specified by the IOM [2] and research criteria [7] as recently recommended by the CFS Advisory Committee. The findings of this study suggest that patients who meet the Canadian criteria [7] are functionally more impaired than the patients that only meet the IOM [2] criteria. In addition, these patients meeting the Canadian research criteria experience symptoms more frequently and severely than the patients only meeting the IOM clinical criteria. These findings offer some support for the CFSAC’s recommendation regarding differentiating the IOM criteria from a more restrictive research criteria [6]. It is still unclear whether this recommendation will be implemented by the Secretary of the Department of Health and Human Services, and for this reason, evaluating different criteria with large samples is both timely and of importance.At the present time, there will be considerable debate concerning the usefulness of the newly-proposed IOM criteria. But ultimately, the research community needs to explore with data the ways these new criteria compare with past ones, as well as how the clinical criteria might differ from a research criteria. This is a healthy discussion and there might be other ways of classifying patients with these types of complex illnesses. For example, rather than classifying patients into the clinical criteria based on the IOM criteria, we might classify patients into the following categories: patients with exclusionary psychiatric or medical illness; and patients who meet IOM criteria, but who do not have psychiatric or medical exclusions. It is still unclear whether a broad category of those who meet the IOM criteria without exclusionary illnesses is the best clinical case definition.
Although the Canadian criteria have been recommended to be the research criteria, there are some problems that exist with these criteria. In a prior literature review on case definitions, Jason, Sunnquist, Brown, and Reed evaluated the Canadian case definition [7,19], and indicated that seven core symptom domains needs to be present for a patient to meet criteria; however, factor analytic studies do not provide support for this seven symptom framework. There certainly needs to be more comparisons of different research criteria so that investigators have a clearer idea of what criteria to use in research. Settling on this issue will make it easier to compare the work from different research labs on patients who meet the IOM criteria. As one example, the Ramsay criteria for myalgic encephalomyelitis (ME) might identify a more homogenous group [20]. Efforts to operationalize the Ramsay criteria occurred with what are now known as the London criteria (Report from The National Task Force, 1994, pp. 96–98). These criteria recognized four cardinal features: (1) physical or mental fatigue or muscle weakness after minimal exertion that may persist long after exertion ends; (2) circulatory impairment (e.g., feeling hot when it is cold, postural hypotension); (3) one or more symptoms indicating the involvement of the central nervous system, such as impairment of memory or concentration and disturbed sleep patterns; (4) and the marked fluctuation of symptoms [21]. In other words, the Canadian criteria seem to identify patients who are more severe than those who meet the IOM criteria, but there may be other diagnostic criteria, such as the London [21] criteria that may identify a more homogenous group with more illness severity. There certainly needs to be more discussion within the scientific community as to what should constitute the research criteria.
Because the term SEID has not been widely endorsed for the IOM criteria, it is possible that this group could be referred to as Neuroendocrine Dysfunction Syndrome (which had been recommended by the patient inspired Name Change workgroup over a decade ago) to replace CFS, and most patient groups want the term CFS to be eliminated. Those that do not meet the research criteria or the broader IOM criteria could be classified as having chronic fatigue, which is the most general category, and represents those with 6 or more months of fatigue. There is considerable merit to using a broader IOM criteria for clinical purposes, although in practice, the the lack of exclusionary conditions, combined with subjectivity, means this will likely be applied to patients with somatoform illnesses and primary mental disorders like anxiety disorders. However, more restrictive criteria could be used for research purposes. Some scientists might prefer to consider the clinical versus research grouping a matter of severity rather than categorical differences, but a well defined research criteria has the potential to clarify discrepant findings from epidemiologic, etiologic, and treatment studies.
The current study used different methods for ascertaining cases, including merging convenience samples with those evaluated by a medical specialist. In addition, as reported elsewhere, there are a number of demographic differences between our British and US samples [22]. However, this heterogeneity has a number of advantages, and it is possible that we might be able to generalizable our findings to a wide host of settings and countries. What we gain in external validity allows our findings to help in the current diagnostic debates concerning clinical and research criteria for what was once known as CFS.
Due to the variety of case defintions that are currently being employed, it has been a challenge to compare results across research studies. Developing a consensus for a clinical and research criteria, as well as operationalizing such criteria with reliable questionnaires, is a high priority area for this field. Ultimately, decisions need to be made regarding the names and criteria for this illness, the vetting process needs to be open, inclusive and transparent, with scientists, clinicians, government officials, and patient groups involved in these deliberations.
Acknowledgements
The authors appreciate the funding provided by NIAID (grant numbers AI 49720 &AI 055735). The authors acknowledge Suzanne D. Vernon’s contribution and that of the Solve ME/CFS Initiative which approved the use of de-identified SolveCFS BioBank registry data in this analysis.References
- Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, et al. (1994) The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med 121: 953-959.
- Clayton EW (2015) Beyond myalgic encephalomyelitis/chronic fatigue syndrome: an IOM report on redefining an illness. JAMA 313: 1101-1102.
- Jason LA, Kot B, Sunnquist M, Brown A, Evans M, et al. (2015) Chronic fatigue syndrome and myalgic encephalomyelitis: towards an empirical case definition. Health Psychol Behav Med 3: 82-93.
- Jason LA, Sunnquist M, Brown A, McManimen S, Furst J (2015) Reflections on the Institute of Medicine’s systemic exertion intolerance disease. Pol Arch Med Wewn 125: 576-581.
- Jason LA, Sunnquist M, Kot B, Brown A (2015) Unintended consequences of not specifying exclusionary illnesses for systemic exertion intolerance disease. Diagnostics 5: 272-286.
- (2015) August meeting of the Chronic Fatigue Syndrome Advisory Committee (CFSAC), Washington, DC.
- Carruthers BM, Jain AK, De Meirleir KL, Peterson DL, Klimas NG, et al. (2003) Myalgic encephalomyelitis/chronic fatigue syndrome: Clinical working case defintion, diagnostic and treatment protocols. J Chronic Fatigue Syndr 11: 7-115.
- Jason LA, Torres-Harding SR, Jurgens A, Helgerson J (2004) Comparing the Fukuda et al. criteria and the Canadian case definition for chronic fatigue syndrome. J Chronic Fatigue Syndr 12: 37-52.
- Jason LA, Brown A, Clyne E, Bartgis L, Evans M, et al. (2012) Contrasting case definitions for chronic fatigue syndrome, myalgic encephalomyelitis/ chronic fatigue syndrome, and myalgic encephaloymelitis. Eval Health Prof 35: 280-304.
- Jason LA, Brown A, Evans M, Sunnquist M, Newton JL (2013) Contrasting chronic fatigue syndrome versus myalgic encephalomyelitis/chronic fatigue syndrome. Fatigue 1: 168-183.
- Jason LA, Sunnquist M, Brown A, Newton JL, Strand EB, et al. (2015) Chronic fatigue syndrome versus systemic exertion intolerance disease. Fatigue 3: 127-141.
- Jason LA, Evans M, Porter N, Brown M, Brown A, et al. (2010) The development of a revised Canadian myalgic encephalomyelitis chronic fatigue syndrome case definition. Am J Biochem Biotechnol 6: 120-135.
- Jason LA, So S, Brown AA, Sunnquist M, Evans M (2015) Test-retest reliability of the DePaul Symptom Questionnaire. Fatigue 3: 16-32.
- Brown AA, Jason LA (2014) Validating a measure of myalgic encephalomyelitis/ chronic fatigue syndrome symptomatology. Fatigue 2: 132-152.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, et al. (2009) Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42: 377-381.
- Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30: 473-483.
- McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD (1994) The MOS 36- item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 32: 40-66.
- Jason LA, Evans M, Brown M, Porter N, Brown A, et al. (2011) Fatigue scales and chronic fatigue syndrome: Issues of sensitivity and specificity. Disabil Stud Q 31.
- Jason LA, Sunnquist M, Brown A, Reed R (2015) Defining essential features of Myalgic Encephalomyelitis and chronic fatigue syndrome. J Human Behav Soc Environ 25: 657-674.
- Ramsay AM (1988) Myalgic encephalomyelitis and postviral fatigue states: The saga of Royal Free disease: Gower Medical for the Myalgic Encephalomyelitis Association.
- Goudsmit E, Shepherd C, Dancey C, Howes S (2009) ME: Chronic fatigue syndrome or a distinct clinical entity? Health Psychol Update 18: 26-33.