Journal of Neurology and Psychology
Download PDF
Research Article
*Address for Correspondence: Svetlana Masgutova, Ph.D, Svetlana Masgutova Educational Institute, LLC, 6275 Hazeltine Dr, Orlando, Florida, 32822, USA, Tel: +1 (720) 544-1166; E-mail: masgutovas@msn.com
Citation: Masgutova S, Akhmatova N, Sadowska L, Shackleford P, Akhmatov E. Progress with Neurosensorimotor Reflex Integration for Children with Autism Spectrum Disorder. J Neurol Psychol. 2016; 4(2): 14.
Copyright © 2016 Masgutova S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology and Psychology | ISSN: 2332-3469 | Volume: 4, Issue: 2
Submission: 22 June, 2016 | Accepted: 19 September, 2016 | Published: 26 September, 2016
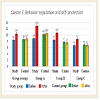
However, the progress in increasing the level of abilities in the Study Group (subgroups A, B, C) depends on the severity of ASD. For example, the changes in Study Group A (mild ASD) overall reached higher points 13.4 and medium in Group B (moderate ASD) - 12.06, and lower in Group C (severe disorder) - 8.55. In Control Group 1 (subgroups A, B, C) there was no dynamic progress. This data shows at the same time that reflex patterns have changed only after directed neurosensorimotor reflex intervention. It also shows the importance of a proper strategy for each individual - taking into consideration their level of ASD severity, therapy tools and procedures, and style/time-frame of work. The more severe the ASD, the more corrective work and longer time-frame will be needed. The results reached within 9 days were very promising; however, our clinical observations show that 2-2.5 years of intense home and training work by professionals with a child with severe ASD is needed to optimize the regulation mechanisms of their brain to get support for more independence, behavior regulation, presence of mind, focus, language development, and improved critical thinking.
Progress with Neurosensorimotor Reflex Integration for Children with Autism Spectrum Disorder
Svetlana Masgutova1*, Nelli Akhmatova2, Ludwika Sadowska3, Patty Shackleford4 and Elvin Akhmatov2
- 1Svetlana Masgutova Educational Institute, LLC, Florida, 32822, USA.
- 2Mechnikov Scientific Research Institute for Vaccines and Serums, 5A Maly Kazenny pereulok, Russia.
- 3Department of Developmental Rehabilitation and Physiotherapy, Wroclaw Medical University of Pastow Slaskich, Poland.
- 4PK Concepts, Melrose, Florida 32666, USA.
*Address for Correspondence: Svetlana Masgutova, Ph.D, Svetlana Masgutova Educational Institute, LLC, 6275 Hazeltine Dr, Orlando, Florida, 32822, USA, Tel: +1 (720) 544-1166; E-mail: masgutovas@msn.com
Citation: Masgutova S, Akhmatova N, Sadowska L, Shackleford P, Akhmatov E. Progress with Neurosensorimotor Reflex Integration for Children with Autism Spectrum Disorder. J Neurol Psychol. 2016; 4(2): 14.
Copyright © 2016 Masgutova S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology and Psychology | ISSN: 2332-3469 | Volume: 4, Issue: 2
Submission: 22 June, 2016 | Accepted: 19 September, 2016 | Published: 26 September, 2016
Abstract
The MNRI® therapy was chosen for facilitation of neurodevelopment in children with ASD. The MNRI® program is aimed at supporting the neuro-sensory-motor system as a marker of the maturity ofextrapyramidal and subcortical brain functions. Children with ASD show obvious asynchronicity and delays in these functions along with poor skills related to early motor milestones. In Reflex Assessments given to children with ASD prior to the MNRI® therapy it was foundthat 83.33% reflex patterns (25 out of 30) were dysfunctional compared to their neurotypical peers. After completion of MNRI® intervention, the number of dysfunctional reflex patterns of these children improved in 63.33% of reflex patterns. The study also shows a correlation between significant improvement in levels of reflex patterns and the children´s cognitive abilities, particularly in such areas as sensory-motor integration, behavioral and emotional regulation, self-awareness, sociability and interaction, stress resilience, physical health, speechand language, cognitive processing, learning, and motivation.Keywords
Masgutova neurosensorimotor reflex integration; MNRI; Reflex integration disorder; Autism reflexes; ASDAbbreviations
MNRI: Masgutova Neurosensorimotor Reflex Integration; ASD: Autism Spectrum DisorderIntroduction
Neurosensorimotor reflex integration, the basis forextrapyramidal nervous system [1-3] and subcortical brain maturation, was the target for study of children with autism that show obvious asynchronicity between cognitive, emotional, and physical development [4-9] and delays in these areas causing poorabilities and skills related to early motor-cognitive milestones. The goal was to analyze the effect of the reflex pattern restorative program - the Masgutova Neurosensorimotor Reflex Integration (MNRI) - on functioning of individuals with autism (total n=484) with different severity, specifically, in areas of sensorimotor integration, behavior, emotional regulation, communication, cognition and other.Results of the Reflex Assessment [10] given to children with autism prior to and after Reflex Integration Therapy were correlated with results obtained by the Questionnaire of Skills Progress [11] within ten domains: behavior, emotional regulation, communication, and others. Statistical analysis based on the multivariable function z=f(x) by A. Krefft and nonparametric comparison by the Wilcoxon and Mann-Whitney tests, using Statistical (version 6.0) have shown significant values at p<0.001 and 0.05 evidencing the effectiveness of reflex integration program results [12,13]. Statistical analysis ound that 83.33% of reflex patterns in children with autism were immature and dysfunctional, showing two-fold evidence: presence of the Reflex Integration Disorder (RID) [10,14,15] and also poor skills development [16-18].
The abnormalities in reflex functions [19] can cause certain deviations in neurodevelopment in children with autism. This study shows clearly the links between the level of autism severity and lower development of reflex patterns and abilities in different areasof their life and learning. The MNRI therapy results show significant progress (p>0.05) in these children in: reflex level development, postural-motor coordination, tactile sensitivity, behavioral control, self-awareness, and other areas. The use of reflex integration therapy can improve the practice of many helping professionals - OT, PT, SP, psychologists and others working with children with autism.
The MNRI therapy modality, based on historical research of reflexes [2,20-22] and clinical observations of individuals´ reflex pathologies, was chosen for facilitation of the neurodevelopment in children with ASD. The MNRI program´s specific reflex circuit restorative strategies and techniques are aimed at supportingthe maturation of the neuro-sensory-motor system. Reflexes are considered to be markers of the extrapyramidal and subcortical brain functions [23-26] that can be seen as reflex integration disorder if they are displayed as poor abilities and skills related to early motor milestones [27,28]. An MNRI Reflex Assessment was given to all children (n=556) prior to and after the study period. Statistical analysis found that a large number of reflex patterns (86.7%/26 out of 30 patterns) in children with ASD show dysfunctional or very low level of development and do not reach the norm compared to children with neurotypical development [28-31].
An unconditioned reflex is automatic, unconscious, and involuntary. This automaticity must mature, moving from the reactivity of infancy to a state in which a reflex activates automatically in response to real danger, and yet does not react inappropriately to stimuli that are not dangerous. Conditioned reflexes incorporate the effects of experience and learning, connecting the basic reflex (lower level of the nerve system) with higher brain structures. This is how internal control develops. Children with mature reflexes can maintain their posture, move, and use reflex motor patterns and theirvariants without having to think about it, so they are free to learn, interact, and grow naturally and easily. A child with immature and hyperactive reflexes must consciously try hard to initiate and control many functions that should activate and be controlled automatically. So when reflexes are delayed, hypo/hyperactive, or non-integrated, they interfere with cortical processing and impede development. Consequences of abnormal reflex development include hyper- or hypotonic muscles, metabolic diseases, neurotransmitter function deficits, vestibular dysfunction, poor brain plasticity, aberrant motor development, difficulties with auditory and visual processing, poor sensory-motor integration, delayed language, and poor social, emotional, and cognitive development.
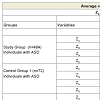
This study concerns three groups of children: one group with ASD who received the MNRI program (Study Group; n=484) and two groups that did not have the MNRI program: one group of children with ASD - Control Group 1 (n=72) and the other with neurotypical development - Control Group 2 (n=483). Children in the Study Group with mild or high functioning ASD (n=134), moderate ASD (n=188), or severe ASD (n=162) are the main targets for current research.
Reflex Assessments done prior to and after the MNRI therapy training (duration of 6 hours daily, 48 hours total) demonstrated a statistically significant improvement in the level of development of reflex patterns of the children with ASD in the Study Group. The number of dysfunctional reflex patterns decreased from 86.7% (26 patterns out of 30) at initial Reflex Assessment to 23.3% (7 patterns out of 30) after completion of the MNRI intervention resulting in improvement of 63.33% of the reflex patterns. This tendency was characteristic for all sub-groups of children with differing levels of severity - mild, moderate, and severe ASD.
The results indicated an evident correlation between the presence of the Reflex Integration Disorder (RID) and the severity level of ASD in the Study Group. The abnormalities in reflex functions can cause a deviation in neurosensorimotor integration and neurodevelopment, and can contribute significantly to problems in development of children with ASD, specifically in areas of: behavior, inner control, emotional regulation, communication and language development, and cognitive processing. This study shows clear links between the levels of reflex patterns and the abilities of children in different areas of their life and learning.
Comparative analysis of progress made by Study Group in their reflex patterns and of their abilities/functioning in areas of behavior/emotional regulation, communication and cognitive functioning after participation in the MNRI therapy training shows significant progress (p>0.05). The changes were particularly noted in: improved postural control, motor coordination, balance, tactile sensitivity, behavioral control, self-awareness, as well as other areas.
ASD, an early childhood disorder, is increasing in the whole world, particularly in technologically developed countries [32,33]. The U.S. Center for Disease Control research indicates that, in some states, one out of every 68 children (one out of 42 boys) is diagnosed with ASD, a 30% increase from 2012 [34]. This pervasive developmental disorder is also on the rise in other countries. The 2012 SDAC showed an estimated 115,400 Australians (0.5%) had autism - a 79% increase from the 64,400 people estimated to have the condition in 2009 [35]; in South Korea the prevalence is 2.64% or 1 in 38 children; in Mexico autism´s prevalence is 1 in 115; in China the autism rate is 16.9 cases per 10,000; in France the autism rate is 5 cases per 10,000; in Denmark the autism rate is 68 cases per 10,000 people [34].
Some typical characteristics in the development of ASD children are well documented [36,37]:
- Tactile hypo or hypersensitivity and/or auditory hypersensitivity.
- Poor eye contact.
- Alimentary behavior disorders such as a preference for a limited number of foods.
- Poorly developed self-defense reactions.
- Inability to connect with the world around them.
- Tendency to focus on negative stimuli and events.
- Poor muscle tone.
- Chronic diseases - seizures, asthma, eczema or skin and food allergies, gastro-intestinal problems (inflammation of the colon).
- Gaps in the development of kinesthetic memory and selfconsciousness.
- Inability to imitate and follow instructions.
When approaching treatment options from the educational perspective, many models and services based on one theory or another of behavioral therapy are noted. These include: Applied Behavioral Analysis (ABA), comprehensive behavioral early intervention - The Early Start Denver Model (ESDM), Relationship Development Intervention (RDI), Floortime therapy, Pivotal Response Therapy (PRT), Verbal Behavioral Therapy, and Social Communication/Emotional Regulation/Transactional Support (SCERTS) [38,39]. Another aspect of the educational treatment for the ASD population includes addressing cognitive issues such as social interaction, difficulties with communication skills and language, and repetitive actions and behaviors. Recent epidemiology studies estimate that approximately 60% of children with autism have IQ´s above 70 by age 8 (70 is the cut-off point for developmental delay) [34]. Such cognitive oriented therapy modalities are being proposed: Structured Teaching (TEACCH), Cognitive Behavior Therapy (CBT), and the Discrete Trial Teaching (DTT) [40]. Traditional and complementary services are directed toward different aspects of their abilities and skills development, such as: Speech-Language Therapy (SLT), Occupational Therapy (OT), Sensory Integration (SI), Physical Therapy (PT), Social Skills, Picture Exchange Communication System (PECS), Auditory Integration Therapy and other aspects [14]. Currently these traditional therapy methods are used with no reliable predictability for the best outcomes for children with ASD, as autism is a lifelong disorder [34].
Even with all the attention given to these medical and educational interventions there are limited studies concerning the aspect of the development of early sensory-motor in these children. The MNRI system calls this - Reflex Integration. Reflex integration is one of the most important neurodevelopmental aspects affecting every function in the course of a child development and the chronology of their brain development [1,22,27,41-46].
MNRI therapy modality offers a key concept and system as a practical tool for treatment of ASD. MNRI offers a corrective intervention for alleviation of Reflex Integration Disorder (RID) as it offers a therapy modality to restore dysfunctional and pathological reflexes [28,46].
This study describes the efficacy of the MNRI program in improving the overall and specific neurodevelopment of children with ASD through targeting individually specific reflex patterns that develop and improve physical and cognitive skills as well as improve behavioral and emotional regulation. Through collection of data and clinical observations, the implementation of the MNRI program has found that dysfunctional reflex pattern expression is evident in two separate groups of children diagnosed with autism: 1) those whose reflexes were immature and deeply dysfunctional from birth, and 2) a group who appeared to develop normally but regressed suddenly into autism at age 2 or 3. In this second ASD group, their reflexes may have been immature at the time of birth but not noticed by parents or specialists until the stress of new learning patterns and more interaction with others occurred during their toddler years. Possibly their nerve systems were not resilient enough to handle these extra stressors and their reflexes were not able to naturally move into a more matured state due to the asynchronicity in their cortical and brain stem functions. This unrecognized weakened state only becomes more evident as the child grows older and expectations become higher. Other life stressors can also interrupt the natural course of neurodevelopment such as physical and emotional traumas, food intolerance, or reaction to toxins.
Children with ASD demonstrate a lack of sensory-motor development and integration skills [47,48] related to early motor milestones that children with typical neurodevelopment go through naturally. Children with ASD either skip all this together or show delayed development of many reflex patterns such as Hands Grasp, Hands Pulling, Hands Supporting, Crawling, Asymmetrical Tonic Neck Reflex, Symmetrical Tonic Neck Reflex, Babkin Palmomental, Ocular-Vestibular, and other reflex patterns. The MNRI program utilizes non-invasive intervention to support maturation in the neuro-sensory-motor system of those reflex patterns through specific strategies and techniques that access resources of reflex circuit components [21,28,46,49] and the protection function of a reflex to normalize over-freezing and fight or flight responses seen, for example, in tactile defensiveness or deprivation [2,3,33,50,51]. This program works with the autonomic nervous system and its sympathetic and parasympathetic processes governing the alarm system of the child as described by H. Selye in 1974 and the working of the hypothalamus, pituitary, and adrenal glands called the HPA stress-axis [51].
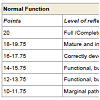
This study presents the reflex profile of children with ASD in which 86.7% of reflex patterns (26 out of 30 patterns) are dysfunctional and 13.3% (4 out of 30 patterns) are functional, but on a very low level of development, compared to those in children with neurotypical development (see Table 1). Previous research [28] has demonstrated that when a threshold of 35% of reflexes is dysfunctional, the result causes reflex integration disorder (RID) [46,52]. The Reflex Profile for ASD revealed that RID is characteristic for children with autism as a majority of their reflex patterns were assessed to be immature and dysfunctional. Knowledge of the state of an individual´s reflex functioning has been the indicator for choosing an effective strategy of reflex integration intervention and filling the gap in addressing neurodevelopmental modalities.
Materials and Methods
This research project specifically focuses on the results of children diagnosed with ASD treated with MNRI therapy program during the years of 2011-2013. The children who participated all showed symptoms in several important areas: 1) social development delays (lack of understanding of family and surrounding social structure, inability for presence in interaction, tendency for hyperactive selfprotection and aggression), 2) speech and communication deficits (non-verbal, poor expressive language, poor conversational language), and 3) behavioral rituals (such as stimming, repetitive movements and actions, hyperactive jumping/running; stuck in certain postures) and abnormal habits (pinching/biting/hitting self and others, hitting the head/jaw/chest, poor toilet control; negative perception of changes in day routine); 4) poor integration of sensory-motor and reflex patterns (disharmonious work of tactile system - hyper and hyposensitivity, tactile defensiveness, seeking for specific overstimulation; delay or dysfunctional reflex patterns); 5) lack of motor and postural programming, planning and control; 6) intellectual processes delay (poor prioritizing and selective perception, delay in focusing and widening the attention span, poor memorizing and cause-reasoning thinking, poor choice making).This study documents the effect of MNRI treatment with 484 children with ASD (4 to 19 years old). There were 172 females (57 girls of 4-6 years, 63 girls of 7-12 years, and 52 girls of 13-19-year-old age) and 312 males (107 boys of 4-6 years, 97 boys of 7-12 years, and 108 boys aged 13-19). All of these children were grouped according to the level of severity of their disorder determined by their official medical documentation based on the main criteria accepted in medical/psychiatry evaluations [46]. Based on this material the 484 children with ASD were described as follows: 27.68%/134 children - mild disorder (also described as high functioning ASD), 38.84%/188 - moderate disorder, and 162/33.47% children - severe disorder.
Each participant was given a pre-assessment (pre-test) followed by the MNRI corrective training sessions and post-test at the end of training Family Conference. Core Specialists who have successfully completed a specific set of courses and clinical hours in MNRI conducted reflex training sessions. The corrective training included 8 days of treatment: 4 days of intense training, one-day rest, followed by another 4 days of training (9 days of duration total). Training session topics included MNRI programs, given to the child on an individual one-to-one basis: Neurostructural Reflex Integration, NeuroTactile Integration, Dynamic and Postural Reflex Re-patterning, Visual and Auditory Reflex Integration, Oral-Facial Reflex Integration, Proprioceptive/Vestibular and Cognitive Skills Development, Lifelong Reflex Integration, and Archetype Movement Integration. Caregivers were also given evening group lectures and training workshops.
In this Study Group of 484 children, each attended at least one MNRI Training Conference held during the 2011 and 2013 calendar years. Family Training Conferences were held in Warsaw, Poland; San Francisco (CA), Minneapolis (MN), West Palm Beach, St. Petersburg, Fort Lauderdale (FL), U.S; and Vancouver (B.C.), Canada. Group sizes at these multiple day conferences were 20-36 participants.
Control Group 1 included 72 individuals with ASD that did not go through the MNRI therapy program. Each participant was given a Reflex Assessment - pre-test and post-test within the same time frame as the Family Training Conferences of 9 days. This group (ASD, n=72) was of the same age range of 4 to 19 years; 28 females and 44 males and had severity levels as follows: 25%/18 children - mild ASD, 30.56%/22 children - moderate ASD, 44.44%/32 children - severe ASD.
Control Group 2 was composed of 483 individuals with neurotypical development that did not go through the MNRI therapy program. Each participant was given a Reflex Assessment pre-test and post-test within the same time frame as the Family Training Conferences of 9 days. Control Group 2 consisted of neurotypical children (aged 4 years to 19 years; 276 females and 207 males without MNRI training).
The New England IRB (85 Wells Avenue, Suite 107, Newton, MA 02459) (IRB ll-173) granted Institutional Review Board (IRB) approval. The New England Institutional Review Board is a central institutional review board for sponsors, CROs and individual researchers across North America (http://www.neirb.com). The IRB ensures the safety of human subjects in clinical trials by committinga thorough and ethical IRB review process. The New England IRB is registered with both the FDA and the Office for Human Research Protections (OHRP) under IORG Number IORG0000444, and has Full Accreditation status from the Association for Accreditation of Human Research Protection Programs (AAHRPP). Adverse effects (new or worsening medical conditions of any kind) were promptly investigated and reported to the IRB.
Ethical approval for this research also was granted by the Health Sciences, Department of Developmental Rehabilitation of Medical Academy by Piastow Slaskich (Wroclaw, Poland) and the Mechnikov Scientific Research Institute for Vaccines and Serums (Moscow, Russia). All participants were assigned codes to protect anonymity. Receipt of informed consent was received from all participants´ parent or legal guardian. MNRI Assessments and therapy sessions were conducted by designated MNRI Core Specialists who had successfully completed the Continuing Professional Education requirements and clinical hours.
The primary outcomes of interest were changes in the reflex patterns of children with autism. Reflex Pattern Assessments were conducted prior to conferences (pre-test) and after conferences (posttest) and the results went through comparative analysis. Evaluations of motor and cognitive patterns considered the child´s age, neurologic abnormalities, and normal status of inborn reflex patterns. Briefly, this entailed grading 30 reflexes (diagnostic qualities/realms coded X1-X30) using five parameters: reflex pattern (or sensory-motor circuit), direction of a motor/postural response, strength of reaction (or muscle tone regulation), time of reaction (latency, length, finishing, dynamic), and symmetry (of all parameters above) with four features for each. Scores were assigned on a continuous scale of 0-4, with 4 indicating full display of a parameter, and 0 indicating the absence of the parameter display resulting (for five parameters) in a maximum score of 20 for each reflex (Table 1). A summary of the varying scores is in Table 1. Reflex patterns were further categorized according to body movement planes, with ten reflex patterns each corresponding to sagittal, horizontal, and dorsal planes [10,46,52].
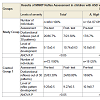
The evaluation of changes in children´s sensory-motor integration, behavior, communication, personality and cognitive areas done by parents and specialists before and after the MNRI therapy training was based on analysis of results of the Questionnaire of Dynamic Changes of Children´s Abilities (see Appendix 1) and its scoring system in points from 0 to 20, with 0 and 1 denoting the lowest developed features and 20 - indicating normal and very well developed (Table 2). This Questionnaire contains 10 clusters of statements reflecting different areas of functioning and everyday activities of children including features from the criteria for autism spectrum (1). The areas that were proposed for evaluation include: 1) Sensory-motor coordination and integration; 2) Behavior regulation and self-protection, 3) Emotional regulation, 4) Self-awareness, 5) Sociability/ interaction, 6) Stress vulnerability/resilience, 7) Physical health, 8) Speech and language, 9) Cognitive processes and learning, and 10) Motivation for achievement and learning. Parents and specialists working with a child gave daily reports during eight days of MNRI training program and one additional summarizing after all of the therapy work is finished. The results of the first and last summarizing report of one parent and four professionals per a child are presented (total of 5 reports on each child). Every statement is evaluated with 5 criteria: ‘neurotypical/normal response’, ‘close to norm/average’, ‘some difficulties’, ‘major difficulties’, ‘pathological response’ (see results of the analysis of Questionnaire in Table 3 as Appendix 2).
Results of Reflex Assessments in children with ASD were analyzed based on the multivariable function z=f(x) of directly non-observable phenomena by A. Krefft [12]. Briefly, this function estimates the level of the reflex pattern integration Z as a function of the grading reflex patterns X1, X2, ..., X30. Consequently, variable ZS (reflex patterns mainly serving the sagittal body plane) summarizes information from the first ten reflex patterns X1, X2, ...,X10, variable ZH (horizontal body plane) summarizing the information from the second ten reflex patterns X11, X12, .., X20, and variable ZD (dorsal) summarizes the last ten reflex patterns X21, X22, .., X30. The level of the reflex pattern integration (ZC) is estimated by all measured reflex patterns (X1, X1,..., X30). In this case, instead of taking 30 values with each of the scores (0 to 20) for each patient, we determined three values of reflex pattern integration by body plane symmetry and/or one value of the reflex pattern integration level Z for values between 0 and 1. Mean values of ZC, ZS, ZH, and ZD were compared before and after participating in the MNRI program using an ANOVA test developed for this type of analysis (IBM SPSS Statistics Grad Pack 22.0). Results were considered statistically significant where p<0.001 and not significant at p>0.05. The results of a level of synthesized function Z=f(x) [13,22] were validated statistically also using nonparametric comparison of two variables by Wilcoxon Matched Pairs test (p>0.001; Statistical Program).
Part of the statistical evaluations was performed also with the Mann-Whitney U-test, using Statistica (version 6.0; Stat Soft Inc, Tulsa, OK, USA). P values (M±SD) less than 0.001 and in the same way were considered significant and not significant at p>0.05.
Also statistical analysis of the data of the Questionnaire of Dynamic Changes of Children´s Abilities [11] was using an ANOVA test (IBM SPSS Statistics Grad Pack 22.0) in which results were in the same way considered statistically significant where p<0.05 and not significant at p>0.05 (Table 4). Also the Mann-Whitney U-test, using Statistica (version 6.0; Stat Soft Inc., Tulsa, OK, USA) was applied, which was interpreting the values (M±SD) less than 0.05 as significant and not significant at p>0.05.
Table 3: Results of comparative analysis of average values and standard deviations with three synthesizing variables: ZS (sagittal body plane), ZH (horizontal), and ZD (dorsal) and ZC (cumulative) in pre- and post-tests levels of reflex patterns development in the Study Group and Control Groups 1 and 2.
The MNRI Reflex Assessment of Individuals with ASD (n=556) was conducted in two groups, Study Group (n=484) and Control Group 1 (n=72), and of Control Group 2 (n=483) of children with neurotypical development as presented in Table 2, showed that dysfunctional reflexes in children with ASD were characteristic for both groups. The Study Group showed 86.7%/26 of reflex patterns as dysfunctional and Control Group 1 showed 83.3%/25 of reflex patterns as dysfunctional with no statistical significance in the number or development level of the deviated reflex patterns in these two groups as p>0.05. Results in Control Group 2 of children with neurotypical development show that all their reflex patterns (100%) are functional (a statistical significance of p<0.05).
In the Study Group, the results before and after the MNRI program (in 9 days) showed highly dynamic changes in the level of reflex patterns in a rather short period of time. The number of dysfunctional reflex patterns (86.7%) at the post-test decreased to 23.3%, which means that 66.7% of patterns moved one level higher to a level designated as “marginal between dysfunctional and functional” and 10% rose to an even higher level of “functional but very low level of development”.
The control groups (Control Group 1 and Control Group 2) that did not go through the MNRI therapy training did not show the positive dynamic in change in the level of reflex pattern development. The comparison of the results in the Study Group and Control Group 1 offers evidence of the positive gains made by MNRI intervention therapy in Study Group (Table 2).
Table 2 expresses the Diagnostic Quality Features (X1-X30) within body movement planes (S=sagittal; H=horizontal; D=dorsal), levels of reflex development, and Assessments results before and after participation in MNRI integration therapy in the Study Group. Note: *statistical significance equal p<0.001. It also presents the pre- and post-Assessment results in control groups that did not go through MNRI intervention (post-test after 9 days). Note: *statistical significance equal p>0.05.
Additional analysis of the average values and standard deviations was carried out for three synthetic variables: ZS (sagittal body plane), ZH (horizontal), and ZD (dorsal) and ZC (cumulative) in pre- and posttests levels of reflex pattern development in the Study Group and Control Groups 1 and 2. The reflex patterns development results in each body plane are statistically significant only in the Study Group that participated in MNRI intervention (Table 4).
The results in Table 4 were validated statistically using data on a level of synthesized function Z=f(x) by NewKrefft algorithm [12] as well as the nonparametric comparison of two variables by Wilcoxon Matched Pairs test (p>0.001; Statistical Program). The statistical evaluation of the data demonstrates significant change in all synthetic variables (with 10 reflex patterns in each) and a high degree of effectiveness for the MNRI program.
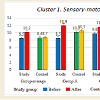
The data of the sensory-motor integration, behavior, communication, personality and cognitive characteristics derived from the Questionnaire of Dynamic Changes in Children´s Abilities [11] collected before and after the MNRI therapy training for children in the Study Group also shows corresponding positive changes in all 10 clusters/areas (Table 4).
Average score for different areas of activity of children before and after the MNRI intervention grew from 13.2 points corresponding to average 9.47±0.46 before and 11.54±0.5 after with statistical significance p<0.05.
Table 5 shows substantial improvement in abilities of children with ASD in Study Group after the MNRI intervention independently of the level of its severity (p<0.05). There were no significant changes in children´s abilities in Control Group 1 in any of sub-groups (A, B, C), where they did not have MNRI intervention (p>0.05 in all subgroups).
Table 5: The results of comparison of progress in children’s sensory-motor integration and abilities in areas of: behavior, communication, personality and cognitive processes evaluated by parents and specialists before and after the MNRI® therapy intervention in Study Group with different level of ASD severity.
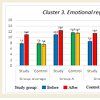
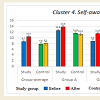
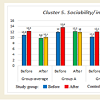
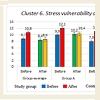
More detailed analysis of the data on the abilities of children with different levels of ASD show that some areas improved more than the others in all three groups (Figures 1-10). Graphs below show the following data: Sensory-motor integration (Cluster 1) shows 8.5 points initially and 10.2 after the MNRI training (p<0.05); Emotional regulation (Cluster 3) shows 7.8 points initially and 10.9 after (p<0.05); Self-awareness (Cluster 4) shows 8.7 and 10.4 after (p<0.05); Stress vulnerability and trauma resilience (Cluster 6) shows 8.7 and 10.8 after (p<0.05); Physical health (Cluster 7) shows 10.4 and 12.8 after (p<0.05); Cognition and learning (Cluster 9) shows 10.7 and 13.2 after (p<0.05); Achievement and learning motivation (Cluster 10) shows 9.6 and 12.8 after (p<0.05). (See data in Graphs 1-10 with means.) The data on such clusters as: Behavior regulation and self-protection (Cluster 2), Sociability/ interaction (Cluster 5), and Speech and language (Cluster 8) before and after the MNRI training also improved statistically (p<0.05) but to a less extent than the other clusters, which based on our experience can mean that results will be demonstrated in new few months. The areas of different abilities of children in Control Group 1 did not show progress (p>0.05, see graphs 1-10 and their medians).
Results
Initial reflex scores of children in the Study Group ranged from a “dysfunctional” level (7.1±0.7 points) and increased after the MNRI intervention to a “low level of development” (13.99±0.4 points) which equals the statistical average of 9.13±0.4 points before and reaching 10.74±0.63* points after intervention though not to the level of development comparable with that of children with neurotypical development (Table 2). Correspondingly, a significant change in the number of their dysfunctional reflexes occurred resulting in improvement of 63.3%/19 of reflex patterns within 8 days of intensive training. Some reflex patterns, such as: the Automatic Gait, Hands Supporting, Flying and Landing, and Pavlov Orientation did not show statistical significance, although positive changes were observed particularly in the following patterns: the Automatic Gait, which became more balanced and reciprocal in a manner and speed of walking, and Hands Supporting which showed better orientation in motor response in space and increased muscle strength.The means of all reflexes summarized in three groups according to the body planes (ZS, H, D values) showed increased progress after completion of the MNRI program, as noted in the cumulative ZC value (Table 4).
Comparative analysis of the improvement of the reflex functions in children with ASD with different levels of severity (A-mild disability, B-moderate, C-severe) demonstrate that the changes in reflex patterns in each of these sub-groups were statistically significant (Table 3 and Table 6).
Table 3 shows that in the group of children with mild ASD (Group A) the number of dysfunctional reflex patterns before intervention was 56.7% patterns (17 out of 30), and after MNRI intervention decreased to 20.0% (6 out of 30) with corresponding average level of reflex patterns development of 10.8±0.41 points before and increasing to 11.85±0.46* points after intervention with statistical significance of p<0.05 resulting in substantial improvement of 36.67%/11 reflex pattern within 8-days of training.
In the group with moderate ASD (Group B), the number of dysfunctional reflex patterns was 86.7% patterns (26 out of 30), and after the MNRI intervention decreased to 36.7.0% (11 out of 30) with corresponding average level of reflex patterns development of 9.67±0.6 points before and increasing to 10.8±0.47* points after MNRI intervention with statistical significance of p<0.05 resulting in significant improvement of 50%/15 reflex pattern.
In the group of children with severe ASD (Group C) the number of dysfunctional reflex patterns was 96.66% patterns (29 out of 30), and after the MNRI intervention it decreased to 60.0% (18 out of 30) with corresponding average level of reflex patterns development of 6.7±0.46 points before and increasing to 8.2±0.47 after the intervention with statistical significance of p<0.05 resulting in substantial improvement of 36.67%/11 reflex patterns.
The above data demonstrates that improvement in the level of development of reflex patterns was noted in each of the ASD groups independently of the severity of their ASD with statistical significance of p<0.05 (Table 3), which proves the beneficial effect of the MNRI intervention.
Control Group 1: Analysis of reflex patterns in children in the Control Group 1 (with ASD that did not go through MNRI training) reveals that there is no positive dynamic in development of their reflex patterns; there is no statistical significance - p>0.05 (Table 4).
A comparative analysis of reflex patterns in children with ASD with different levels of severity (A - mild disability, B - moderate disability, C - severe disability) in Control Group 1 showed that changes in each sub-group were not statistically significant (Table 3). In the group of children with mild ASD (Group A) the number of dysfunctional reflex patterns was 60.0% patterns (18 out of 30), and after the 9 days it was still 60.0% (18 out of 30) with corresponding average level of reflex patterns development of 10.9±0.7 points before and increasing to 10.7±0.31 after the intervention with no statistical significance as p<0.05.
In the group with moderate ASD severity (Group B) the number of dysfunctional reflex patterns was 90.0% patterns (27 out of 30), and after 9 days it increased to 93.3% (28 out of 30) with corresponding average level of reflex patterns development of 9.1±0.75 points before and 8.9±0.6 points after the intervention with no statistical significance as p<0.05.
In the group of children with severe ASD (Group C), the number of dysfunctional reflex patterns was 93.3% patterns (28 out of 30) and after 9 days it increased to 96.6% (29 out of 30) with corresponding average level of reflex patterns development of 6.8±0.7 points before and increasing to 6.7±0.46 after the intervention with no statistical significance as p<0.05.
Therefore, these results show no positive dynamic in changes of level of development of reflex patterns in pre- and post-assessment in children of Control Group 1, who did not go through the MNRI therapy procedure.
Analysis of reflex patterns of children in Control Group 2 (children with neurotypical development that did not go through MNRI therapy) reveals that all their reflex patterns were functional and that there were not any dynamics in development of their reflex pattern at statistical significance level (p>0.05) (Table 2 and Table 4).
Based on data above, the changes in development of reflex patterns happened only within the Study Group and in every level of severity sub-group of children with different levels of severity (A, B, C) (p<0.01), while in the control groups significant changes did not occur (p>0.05). This means that only children in the Study Group benefited significantly from the MNRI therapy consisting of the specially designed program targeting their neurosensorimotor reflex integration. Reflex patterns of children with severe ASD increased from 6.7±0.46 points in pre-tests to 8.2±0.47* after the MNRI intervention versus Group A with mild ASD with 10.9±0.7 points in pre-test and 10.7±0.31 points in post-test, and in group B with 9.1±0.75 points in pre-test and 8.9±0.6 in post-test. This data shows the importance of creating more specialized individual strategies and programs to work with reflex integration and other modalities for children with ASD at various severities. The most important therapy consideration must be focused on precise knowledge of the child’s reflexes as a phenomenon, their parameters and levels of maturity, the ability levels of these children, and developmental time factors, because children with severe ASD especially need regular and longer term work with specialists and parents trained in the MNRI intervention procedures.
An interesting clinical fact was also observed: progress in correction of the reflex patterns in the Study Group was somewhat dependent on age - it was greater in the group of children aged 4 years to 5 years and the group of children aged 6 to 12 years. Change was significant but less actively dynamic in the group of children aged 13-18 years, which can be interpreted as the MNRI program may guarantee more positive results in children of 0-12 years of age. For this reason, we emphasize the importance of early intervention [53-55]. This information may suggest that older children and adults may benefit from longer-term work with the MNRI tools. This can be studied in a longitudinal study. Long-term clinical analysis of results of the work with children from 2 to 5 years of age with ASD suggests that faster results of changes in reflex patterns occur when MNRI reflex integration intervention is applied at an early age. So, early intervention is a must strategy while working with children with ASD, as the essence of the reflex integration work addresses early sensory-motor patterns.
Children with ASD have a number of developmental disorders [15,56] and there is a need to identify efficacious strategies for improving their functional capabilities. MNRI has been developed as a means of assessing and improving the neurological function of children with developmental disorders [28]. The MNRI therapeutic modality is based on the concept that improving the reflex patterns of children with developmental disorders will improve their sensorimotor integration, behavior regulation and self-control, cognitive planning, and emotional growth. This concept was developed based on clinical observations of improved function among children participating at MNRI Family Conferences [28]. Further support for this concept was evident when improved reflexes resulted in improved gross and fine motor coordination and postural control described by Bernstein [57]. Bobath & Bobath noticed in their earlier works that this concept in educational process improved behavior because children learn to regulate involuntary, unconscious, spontaneous motor activity, and emotional responses [58]. These improvements have also been noticed in children who are involved in MNRI training.
When using the MNRI program to reeducate non-integrated reflexes of a child with ASD or rerouting the circuits of their dysfunctional patterns, the training directed at facilitation of these reflexes should begin as early as possible, when automaticity is the natural ‘focus’ of the neurodevelopment. This Study demonstrates the positive growth found when using the MNRI program to reeducate non-integrated reflexes of a child with ASD or rerouting the circuits of their dysfunctional patterns. Maturation of the automaticity level of the nerve system will serve as a basis for the voluntary sensorymotor performance of a child. Still the use of these early sensory motor patterns - reflexes - can improve dysfunctions and move poor abilities to a higher level in a lesser amount of time. As a child with ASD exhibits a multi-dysfunctional disorder, the therapy program should provide a multi-directional approach based on the individual dysfunctional characteristics of a child. A priority of MNRI therapy for children with ASD is to improve their neurodevelopment, emotional, social, and cognitive functioning through reflex integration and neuroplasticity.
This study has measured the abilities of children with ASD within 10 clusters: 1) sensory-motor coordination and integration; 2) behavior regulation and self-protection, 3) emotional regulation, 4) self-awareness, 5) sociability -interaction, 6) stress vulnerability - resilience, 7) physical health, 8) speech and language, 9) cognitive processing and learning, 10) motivation for achievement and learning [11]. (Data in Graphs 1-10). It concluded that their development correlated with their level of reflex integration disorder. The improvement of the children with ASD (for all levels of severity) after MNRI therapy modality shows that changes are possible within a shorter time frame and with more stable changes than we usually observe in traditional educational-therapeutic settings. Thus the modality of neurosensorimotor integration must become a focus in the work of developmental specialists.
Clinical observations of professionals (OTs, PTs, SPs, special educators, psychologists) and parents also show that children with ASD, demonstrate substantial improvements after interventions using the MNRI program. These often include balance, postural control, motor programming, planning and control that facilitates coordination of movements, strength, precision, space-time orientation, speed of perception and response, and better presence of mind, focusing, memorizing, and language development (receptive and expressive).
It is crucial that reflex integration therapy be offered as an early intervention when any developmental delay of reflex patterns is observed. It is the authors’ premise that reflex integration should be used as a tool for early intervention for all children demonstrating developmental challenges. All children with ASD, whatever their age, can benefit from the support and correction of motor patterns and underdeveloped or dysfunctional reflexes [14,59,60].
An MNRI Assessment provides unique reflex profiles of children with ASD (Tables 2-4) which can orient professionals in creating individualized therapy programs for each child’s specific developmental challenges. MNRI Assessments of children with ASD show that most of their reflex patterns (86.7%) are at the dysfunctional level which, in MNRI validated Reflex Assessment models indicates the reflex integration disorder (RID). MNRI research provides statistically valid data in creating the hypothesis that RID is one of themost important underlying causes of ASD.
A comparison of changes in reflex parameters before (86.7%/26 dysfunctional of 30 reflex patterns) and after the MNRI therapeutic training (23.3%/7 being dysfunctional) showed specifically that positive change occurred in children´s reflex patterns within 8 daysof 6-hour daily intensive training in all three sub-groups; those with mild, moderate, and severe ASD. The average of 63.3%/19 improved reflex patterns, with progress noted in the level of reflex integration in all subgroups of severity at the p<0.001. This suggests a positive achievement in ‘rerouting’ and bringing the reflex pattern back to its genetically given place and functions in the nervous system, which strongly supports a step toward normal neurodevelopment. The unique function of the MNRI program to ‘teach and re-train’ the brain to improve its own sensory-motor links and functions is done by activation of primary unconditioned reflex schemes to facilitate voluntary sensory-motor abilities and skills.
Thus, the MNRI program for children with ASD opens up the possibility of regaining their neurosensory motor reflex integration, improvement in emotional and behavior regulation, increasing self-awareness, learning, and development of their own unique personalities.
Conclusion and Future Work
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards ofthe institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.This article does not contain any studies with animals performed by any of the authors.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Acknowledgements
The authors wish to acknowledge Prof. Anna Krefft of Medical Academy of Poland for her valuable suggestions for study organization; Sally Averkamp, the publishing specialist of the Svetlana Masgutova Educational Institute® (SMEI), LLC, for her content, language, and technical editing; for Vicky Roy, Ph.D. for her contribution in scientific language editing; and also the SMEI organization for funding the research.References
- Haines DE (2002) Fundamental neuroscience for basic and clinical application. (4th edn.), Elsevier Saunders, Philadelphia, USA, pp. 504.
- Sechenov I (1935/2012) Selected physiological and psychological works. Foreign Languages Publishing House, Moscow, Russia.
- Sherrington C (1947) The integrative action of the nervous system. Cambridge University Press, London, UK, pp. 433.
- Cohn E, Miller LJ, Tickle-Degnen L (2000) Parental hopes for therapy outcomes: children with sensory modulation disorders. Am J Occup Ther 54: 36-43.
- Bundy A, Lane S, Murray E (2002) Sensory integration theory and practice. (2nd edn.), F.A. Davis Company, Philadelphia, USA.
- Brody LE, Mills CJ (1997) Gifted children with learning disabilities: a review of the Issues. J Learn Disabil 30: 3, pp. 282-296.
- Kranowitz SK (1998) The out-of-sync child has fun: Activities for kids with sensory integration dysfunction. New York, NY: G P Putnam's Sons.
- Oberman LM, Hubbard EM, McCleery JP, Altschule EL, Ramachandran VS, et al (2005) EEG evidence for mirror neuron dysfunction in autism spectrum disorders. Brain Res Cogn Brain Res 24: 190-198.
- Durden WG, Mills CJ (1993) Talent derailed: The education establishment's assault on ability grouping. Wisconsin Interest 2: 43-50.
- Masgutova S, Masgutov D (2015) MNRI® assessment for determining the level of reflex development. In book: Reflexes: Portal to Neurodevelopment and Learning. A Collective Work. USA: SMEI, Florida, pp. 201-209.
- Masgutova S (2016) The Questionnaire of Dynamic Changes in Children´s Abilities.
- Krefft A (2007) Diagnosis of functions of invisible phenomena (Statistic Mathematic Analysis). Wroclaw, PL: Ofycyna Wydawnicza Politechniki Wrocławskiej.
- Cheung YK, Klotz JH (1997) The Mann-Whitney Wilcoxon distribution using linked lists. Stat Sin 7: 805-813.
- Lemer PS (2008) Envisioning a bright future. Interventions that work for children and adults with autism spectrum disorders. OEP Foundation, Santa Ana, CA, USA, pp. 414.
- Cashin A, Sci DA (2006) Two terms--one meaning: the conundrum of contemporary nomenclature in autism. J Child Adolesc Psychiatr Nurs 19: 137-144.
- al´Absi M, Hugdahl K, Lovallo WR (2002) Adrenocortical stress responses and altered working memory performance. Psychophysiology 39: 95-99.
- Clark L, Iversen SD, Goodwin GM (2001) The influence of positive and negative mood states on risk taking, verbal fluency, and salivary cortisol. J Affect Disord 63: 179-187.
- Condren RM, O´Neill A, Ryan MC, Barrett P, Thakore JH (2002) HPA axis response to a psychological stressor in generalized social phobia. Psychoenuroendocrinology 27: 693-703.
- Schott JM, Rossor MN (2003) The grasp and other primitive reflexes. J Neurol Neurosurg Psychiatry 74: 558-560.
- Pavlov I (1927/1960) Conditioned reflexes: An investigation of the physiological activity of the cerebral cortex. Dover Publications Inc, New York, USA.
- Luria AR (1978) Functional brain organization. In Book: Biological-scientific basis of psychology, Ed. By Smirnov AA, Luria AR, Niebilistsin VD. Moscow, Russia, pp. 109-139.
- Sherrington C (1947) The integrative action of the nervous system. Cambridge University Press, London, UK.
- Thabit MN, Nakatsuka M, Koganemaru S, Fawi G, Fukuyama H, et al. (2011) Momentary reward induce changes in excitability of primary motor cortex. Clin Neurophysiol 122: 1764-1770.
- Rumsey JM (1992) Neuropsychological studies of high-level autism. In Schopler E, Mesibov GB (Eds.), High-functioning individuals with autism. New York: the Plenum Press. pp. 41-64.
- Baron-Cohen S, Ring H, Moriarty J, Schmitz B, Costa D, et al. (1994) Recognition of mental state terms. Clinical findings in children with autism and a functional neuroimaging study of normal adults. Br J Psychiatry 165: 640-649.
- Manjiviona J, Prior M (1995) Comparison of Asperger syndrome and high-functioning autistic children on a test of motor impairment. J Autism Dev Disord 25: 23-39.
- Piña-Garza J (2013) Fenichel’s clinical pediatric neurology: A signs and symptoms approach. Elsevier, Atlanta, GA, USA.
- Pilecki W, Masgutova S, Kowalewska J, Masgutov D, Akhmatova N, et al. (2012) The impact of rehabilitation carried out using the Masgutova Neurosensorimotor Reflex Integration method in children with cerebral palsy on the results of brain stem auditory potential examinations. Adv Clin Exp Med 21: 363-371.
- Burhans LB, Smith-Bell, CA, Schreurs BG (2010) Effects of extinction on classical conditioning and conditioning-specific reflex modification of rabbit heart rate. Behav Brain Res 206: 127-134.
- Lennartz RC, Weinberger NM (1992) Analysis of response systems in Pavlovian conditioning reveals rapidly versus slowly acquired conditioned responses: support for two factors, implications for behavior and neurobiology. Psychobiology 20: 93-119.
- Chang RC, Stout S, Miller RR (2004) Comparing excitatory backward and forward conditioning. Q J Exp Psychol B 57: 1-23.
- Hall L (2012) Autism spectrum disorders: From theory to practice (2nd edn.), Pearson, Boston, MA, USA.
- Rutter M, Silberg J (2002) Gene-environment interplay in relation to emotional and behavioral disturbance. Annu Rev Psychol 53: 463- 490.
- Autism Society, Facts and Statistics.
- Australian Bureau of Statistics.
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th edn).
- O’Reilly R, Morlet T, Cushing S (2013) Manual of Pediatric Balance Disorders. Plural Publishing Inc, San Diego, CA, USA.
- Odom S, Collet-Klingenberg L, Rogers SJ, Hatton D (2010) Evidence-based practices in interventions for children and youth with autism spectrum disorders. Prev Sch Fail 54: 275-282.
- Gresham FM, Frankenberger B, MacMillan E, Donald LA (1999) Selective review of treatments or children with autism: description and methodological considerations. School Psych Rev 28: 559-567.
- Wikipedia search of TEACCH, Cognitive Behavior Therapy (CBT), and Discrete Trial Teaching (DTT).
- Vygotsky L (1934/1986) Thinking and Speech. (Edited and translated in part by Eugenia Hanfmann and Gertrude Vakar, and in part by Norris Minnick). The M.I.T. Press (1962).
- Vygotsky L (1934/1986) The child psychology. The problems of child development. M. G. Jaroshevsky. In 6 Books. Moscow, Russia.
- Lanciego J, Luquin N, Obeso JA (2012) Functional Neuroanatomy of the Basal Ganglia. Cold Spring Harb Perspect Med 2: a009621.
- Gross R (1987) Psychology. The science of mind and behavior. Hodder and Stoughton, London, UK.
- Sechenov I (1863/1995) Physiology of behavior. Scientific works/ Ed. Jaroshevsky MG. Moscow, Russia.
- Masgutova S, Masgutov D, Akhmatova N, Akhmatov E (2015) Neurophysiological foundation of the MNRI® reflex integration program. In book: Reflexes: Portal to Neurodevelopment and Learning pp. 31-40.
- Bauman ML, Kemper TL (2005) Neuroanatomic observations of the brain in autism: a review and future directions. Int J Dev Neurosci 23: 183-187.
- Dawson G, Watling R (2000) Intervention to facilitate auditory, visual, and motor integration in autism: a review of the evidence. J Autism Dev Disord 30: 415-421.
- Campbell S (2004) Watch me grow: A Unique, 3-Dimensional Week-by-Week Look at Your Baby's Behavior and Development in the Womb. Carroll & Brown Publishers Ltd, London, UK.
- Barashniev J (2001) Prenatal Neurology. Triada-X, Moscow, Russia.
- Selye H (1974) Stress without distress. J. B. Lippincott Co, Philadelphia, USA.
- Pilecki W, Kipiński L, Szawrowicz-Pełka T, Kałka D, Masgutova S (2013) Spectral Brain Mapping in Children with Cerebral Palsy Treated by the Masgutova Neurosensorimotor Reflex Integration Method. J Neurol Sci 333: e550.
- Boyd B, Odom S, Humphreys B, Sam A (2010) Infants and toddlers with autism spectrum disorder: early identification and early intervention. J Early Interv 32: 75-98.
- Hume K, Bellini S, Pratt C (2005) The usage and perceived outcomes of early intervention and early childhood programs for young children with autism spectrum disorder. Topics in Early Childhood Special Education 25: 195-207.
- Reed P, Osborne L, Corness M (2007) The real-world effectiveness of early teaching interventions for children with autism spectrum disorder. Exceptional Children, 73: 417-433.
- Gutstein S (2009) The RDI book. Forging new pathways for autism, Asperger’s and PDD with relationship development intervention program. Connections Center Publishing, Houston, TX, USA.
- Bernstein N (1997) Bio-mechanics and physiology of the movement. Moscow-Voroniez, Moscow, Russia.
- Bobath K, Bobath B (1984) The neurodevelopmental treatment. Scrutton D, editor. Management of the Motor Disorders of Children with Cerebral Palsy. Oxford: Blackwell Scientific Publications Ltd. 6-18.
- O´Dell N, Cook P (1997) Stopping hyperactivity. A new solution. A unique and proven program of crawling exercises for overcoming hyperactivity. Doubleday, Garden City Park, NY, USA.
- Sadowska L (2001) Neurokinesiological diagnosis and therapy of children with mental and motor deficits. AWF, Wroclaw, Pl.