Journal of Nutrition & Health
Download PDF
Research Article
Analysis of Pregnancy Testing Index Results in Miyun District, Beijing from 2017 to 2021
Lu Yu1, Gaiyan L2, Jinxin G1, Hongmei X1,3 and Ting L4*
1Hebei University, Hebei, China
2Xingtai Third Hospital, Hebei, China
3The First Hospital of Hebei Medical University, Hebei, China
4Beijing Maternity, & Child Healthcare Hospital, Beijing, China
*Address for Correspondence:
Ting L, Beijing Maternity & Child Healthcare Hospital, Beijing, China; Tel:
13552960339; Email: 13552960339@163.com
Submission: 30 May, 2022
Accepted: 29 June, 2022
Published: 01 July, 2022
Copyright: © 2022 Yu L, et al. This is an open access article distributed
under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided
the original work is properly cited.
Abstract
To understand the physical health of women during pregnancy
in Beijing, the data of pregnant women who attended the obstetrics
outpatient clinic of Miyun District Maternal and Child Health Hospital
of Beijing from 2017 to 2020 were selected. The blood lipid indexes
(the triglyceride (TG), total cholesterol (TC), high-density lipoprotein
cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C)),
75g oral glucose tolerance test (fasting plasma glucose, 1hplasma
glucose, 2h plasma glucose) and thyroid hormones (thyroid stimulating
hormone (TSH), free thyroxine (FT4), free triiodothyronine (FT3), total
thyroxine (TT4), and total triiodothyronine (TT3)) of 11 parameters
were analyzed. The levels of lipid and thyroid hormones in pregnant
women, during 2017-2021, showed a general trend of decreasing
and then reversing increase, and the difference was statistically
significant (P< 0.0001). Fasting blood glucose, 1h postprandial and 2h
postprandial blood glucose showed a trend of chronological increase
(P< 0.0001). Except LDL-C, Lipid index levels and fasting glucose, 1h
postprandial and 2h postprandial glucose levels increased with age in
pregnant women (P< 0.0001). The opposite trend was observed for the
indicators of thyroid function measurement. There were chronological
differences in the abnormal rates of lipid index, OGTT, and thyroid
hormones during pregnancy, but the trend was not significant. The
abnormal rates of HDL-C, LDL-C were high. Lipid, blood glucose and
thyroid hormone index in Miyun District of Beijing can better reflect the
physical condition of pregnant women, and strengthening the indexes
is of great value for eugenics and expected female health.
Keywords
Early pregnancy; Pregnant women; Lipids; Blood
glucose; Thyroid hormone levels
Introduction
As the economic level in China continues to rise, the dietary
habits of pregnant women have changed dramatically, leading to
an increasing number of complications during pregnancy. In order
to adapt to the needs of fetal growth and development during
pregnancy, the hormones in pregnant women’s bodies change
accordingly, and all indicators of the body are prone to change. The
level of progesterone and human placental prolactin increases with
the prolongation of pregnancy, which leads to excessive lipolysis
and reduced synthesis, resulting in physiological elevation of blood
lipid level in pregnant women and a certain degree of elevated blood
lipid level, but pathological elevation of blood lipid tends to induce
a series of metabolic diseases [1]. After pregnancy, the thyroid gland
is relatively active due to the dual regulation of hypothalamuspituitary-
thyroid axis and placenta-thyroid axis and its metabolism
is enhanced accordingly, which may lead to hyperthyroidism and
hypothyroidism [2]. At 24-28 weeks, the need for insulin of pregnant
women reaches its peak. While the secreted insulin is not enough to
maintain the normal level of glucose, it will cause metabolic disorders
such as gestational hypertension, infection and ketoacidosis [3].
In order to understand the physical condition of pregnant women
during pregnancy in Miyun District, this study collected data from
pregnant women in obstetric clinics from 2017-2021, and the study
is as follows.
Material & Methods
Study Population
All pregnant women who attended the obstetrics department of
Miyun District Maternal and Child Health Hospital in Beijing from
January 2017 to December 2021 were selected. Exclusion criteria:
pregnant women with diabetes mellitus or other severe metabolic
diseases before pregnancy.
Data collection
This study is a hospital-based multi-stage cross-sectional study.
It collected the results of glucose tolerance test, lipid and thyroid
function indexes from the investigated subjects through the hospital
electronic information system. The study was reviewed and approved
by the Ethics Committee of Miyun District Maternal and Child
Health Hospital, Beijing, China.
Research Methods
Based on the 9th edition of Obstetrics and Gynecology, the reference
values of laboratory tests are used as the basis for judgment [4].
The reference ranges of OGTT: 24-28 weeks of pregnancy oral
glucose tolerance test diagnostic criteria fasting blood glucose, 1h
blood glucose, 2h blood glucose of 5.1, 10.0, 8.5 mmol/L, respectively.
The reference ranges of lipid indicators: TC, TG,HDL-C, LDL-C
is 3.49-5.55mmol/L, 0.25-1.71mmol/L, 1.29-1.55mmol/L, and
2.07-3.10mmol/L, respectively.
The reference ranges of thyroid function indicators: TT3, TT4,
FT3 measured by ECLIA method is 1.3-3.1nmol/L, 66-181nmol/L,
3.1-6.8pmol/L; TSH measured by Roche reagent is 0.05-5.17mIU/L,
FT4 measured by Roche reagent is 12.91-22.35pmol/L from 2017 to
2019; afterwards it measured by Beckman reagent is 7.64-16.03pmol/L.
Statistical Analysis
Continuous variables were expressed as mean ± standard
deviation, and categorical variables were expressed as rate ratio. The Kruskal-Wallis test was used for comparison between years and
age groups for each parameter, and the chi-square test was used to
compare the differences in abnormal rates of maternal indicators
between years. Statistical significance was defined as < 0.05. All
statistical were performed using IBM SPSS Statistics for Windows
version 26.0.
Results
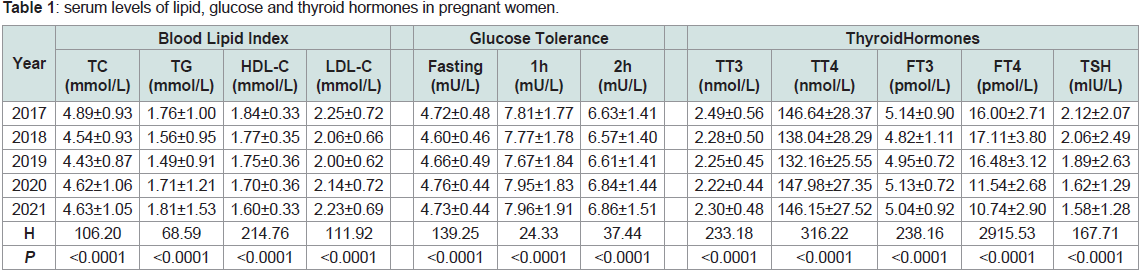
Comparison of differences in parameters between year groups
Analysis of lipid indicators during pregnancy from 2017-2021
revealed that TC, TG, and LDL-C levels decreased year by year and
began to reverse in 2019, while HDL-C levels showed an overall
decreasing trend over time. Fasting blood glucose, 1h postprandial
and 2h postprandial blood glucose was found to have the lowest
levels in 2018, and then showed an increasing trend by years. FT4
and TSH levels showed an overall decreasing trend from 2017-2021,
while TT3 and FT3 levels had chronological differences and had the
highest in 2017, although the change trend was not obvious. The
differences between year groups for all the above indicator values
were statistically significant (P< 0.0001), as shown in Table 1.
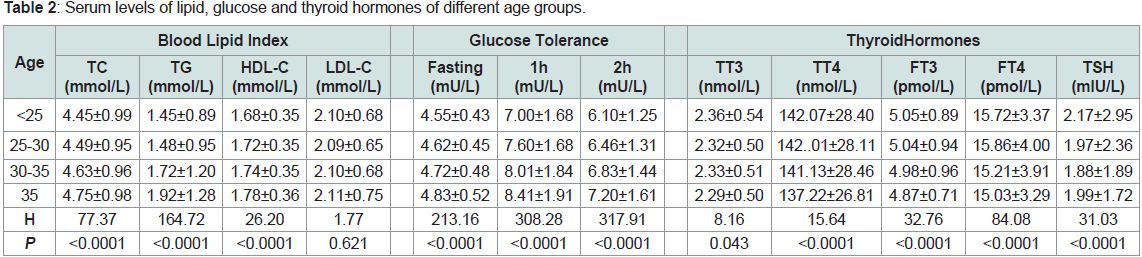
Comparison of differences in parameters between age groups
Table 2 revealed that TC, TG, and HDL-C values increased with
age (P<0.0001). Blood glucose showed a continuous increasing trend
(P<0.0001). Among the thyroid function indicators, TT4, FT3, and
FT4 levels basically maintained a decreasing trend with age and
were statistically different (P< 0.0001). TT3 and TSH did not change
significantly and remained the highest in 2017.
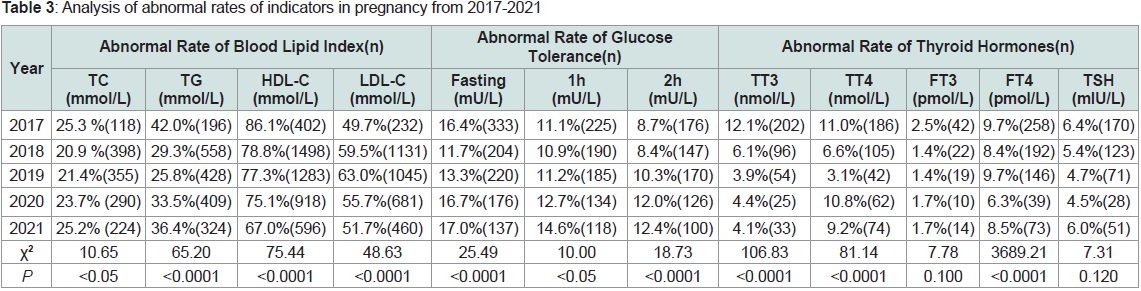
Comparison of parameter abnormality rates between year groups
HDL-C abnormality rate decreased year by year from 2017-2021,
and the difference was statistically significant (P< 0.0001). The trend
of change in TC and TG abnormality rate was roughly the same, TC
abnormality rate started to decrease in 2017, and the abnormality rate reached the lowest value in 2018 then reversed. The TG abnormality
rate climbed after the lowest in 2019. The trend of change in LDL-C
abnormality rate was exactly the opposite of TG. The trend of
fasting glucose, 1h glucose, and 2h glucose abnormality rate changes
is roughly the same: it drops to the lowest in 2018, and then the
abnormality rate climbs and exceeds the abnormality rate in 2017.
TT3 and TT4 abnormality rates both decrease from 2017 to 2019, and
show a small increase and then decrease in 2020, as shown in Table 3.
Discussion
The results of this study showed that the differences in lipid,
glucose and thyroid hormone levels in early pregnancy were
statistically significant (P< 0.0001) in between 2017-2021. Except for
LDL-C, other indicators were also statistically significant at different
ages (P< 0.001). Levels of TC, TG, HDL-C, LDL-C were lower
thanEuropean pregnant women [5]. TC and TG levels were higher
in early pregnancy than Zheng et al [6]. However, TC, TG, HDL-C,
LDL-C were lower than the levels in Southern parts of China [7].
Thyroid hormones such as TSH, FT3 are higher than Chen Dan et al
[8]; FT3, FT4 were higher than those in Xining [9]. TT3, TT4, FT3,
FT4, TSH levels are higher than Guizhou [10]. This indicates that
there are differences between the data from Beijing area and other
areas, which may be related to the differences in economic culture,
dietary habits, geographical location, and iodine nutrition status of
the population.
According to age subgroups, serum lipid levels were found to be
largely elevated in varying degrees. It may be due to the fact that aging
hepatocytes reduce diet-induced apolipoprotein B synthesis with age,
and some elderly women exhibit high cholesterol, triacylglycerol,
high LDL levels, and clinical hyperlipidemia [11].
In this study, we found that blood glucose levels in Miyun District
showed a trend of increasing with year and age. This trend may be
due to over-nutrition in women during pregnancy due to excessive
material intake and unreasonable diet structure.
TG, TC, HDL-C, and LDL-C are commonly used clinically as
indicators of lipid metabolism levels. Some studies have shown
that the incidence of large babies with abnormal lipid levels during
pregnancy is about 30% [12]. Subsequent studies have confirmed that
dyslipidemia during pregnancy is an important predisposing factor
for the occurrence of adverse pregnancy outcomes [13]. One study
found that three or more meals a day and a preference for lighter
tasting foods were independent risk factors for maternal dyslipidemia
in the third trimester [1]. A light diet may reduce satiety, leading to
more frequent meals and excessive carbohydrate intake, which can
eventually lead to the development of maternal dyslipidemia.
In early pregnancy, human chorionic gonadotropin is at a high
level, which binds to thyroid stimulating hormone receptors and
increases thyroid hormone secretion, while pregnancy is a stressful
stimulus to the thyroid gland, which increases the size of the thyroid
gland and increases the demand for thyroxine [14]. Some studies have
reported that the type of salt consumed, blood pressure, blood lipids,
and blood glucose are factors influencing abnormal thyroid levelsin
pregnant women in early pregnancy [15]. These factors can lead to
hyperthyroidism and hypothyroidism in early pregnancy. The body
can compensate to maintain the consumption of thyroid hormones in
mid and late pregnancy, but iodine deficiency is common in women
in early pregnancy. Iodine demand increases in early pregnancy,
and consumption of iodized salt is beneficial to the balance of iodine
supply and demand, which can further strengthen the publicity and
education of iodine supplementation for women in early pregnancy
[16].
Coronavirus disease 2019 (COVID-19) epidemic, which has
been ongoing since 2019, has widely affected social production and
people’s lives, bringing negative psychological reactions such as
anxiety and depression to varying degrees. Pregnant women, who
are in the special physiological process of pregnancy, They are more
prone to anxiety and depression in the face of the risk of infection,
medical problems, fetal health and other problems brought about
by the epidemic [17]. Under the influence of negative emotions,
pregnant women are also more likely to exhibit high blood lipid levels
and impaired blood sugar control [18]. And due to the epidemic,
obstetric outpatient clinics are restricted and lack individualized
interventions for pregnant women, making it difficult to meet their
medical needs. And pregnant women have decreased exercise due to
reduced supervision by medical staff and the inability to go outside,
resulting in significant weight gain [19].
It is thus clear that screening, monitoring and management of pregnant women should be strengthened during special periods, and
guidance on balanced diet during pregnancy and the deployment
of nutrients, as well as supervision of exercise for women during
pregnancy, early detection and elimination of adverse outcomes, are
important measures to ensure the safety of mother and child.
In summary, this study identified the process of dynamic
changes in blood lipid, glucose, and thyroid hormone levels in
women during pregnancy, providing a basis for subsequent studies
of factors affecting women during pregnancy. While this study
collected obstetric outpatient results horizontally for 5 years, due to
the large amount of data, there may be cases that were included in
that exclusion due to the lack of perfect and comprehensive clinical
information of the patients when excluding data according to the
exclusion criteria, resulting in statistical bias. The present study only
examined the indicators in their current state, and no association
could be established between the data.
Conclusion
The rates of abnormalities in blood lipid, glucose, and thyroid
indicators roughly have a trend of rising, which may be closely related
to adverse pregnancy outcomes. The monitoring of lipid and glucose
thyroid indicators during pregnancy should be strengthened, and
maternal care should be emphasized to improve pregnancy outcomes.
Acknowledgement
This research was funded by the research grant from the Natural
Science Foundation of Hebei Province (No. H2021201054), Science
and Technology Research Project of Higher Education in Hebei
Province (No. QN2019130) and Xingtai city key research and
development plan (No. 2020ZC309).