Journal of Geriatrics and Palliative Care
Download PDF
Research Article
*Address for Correspondence: Everlien de Graaf, Academic Hospice Demeter, Weltevreden 3, 3731 AL De Bilt, the Netherlands, Tel: 31654394889; Fax: 31302202596; E-mail: e.degraaf@hospicedemeter.nl
Citation: de Graaf E, Zweers D, de Graeff A, Daggelders G, Teunissen S. Does Age Influence Symptom Prevalence and Intensity in Hospice Patients, or Not? A Retrospective Cohort Study. J Geriatrics Palliative Care 2014;S(1): 7.
Copyright © 2014 Graaf et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Geriatrics and Palliative Care | ISSN: 2373-1133 | Special Issue
Submission: 18 August 2014| Accepted: 25 September 2014 | Published: 29 September 2014
Reviewed & Approved by: Dr. Huai Yong Cheng, Associate Professor of General Medicine, Geriatrics and Palliative Care at University of Virginia, USA.
Does Age Influence Symptom Prevalence and Intensity in Hospice Patients, or Not? A Retrospective Cohort Study
E de Graaf1,2, D Zweers RN 2,3, A de Graeff 1,3, G Daggelders 1,4 and S Teunissen RN1,2
- 1Academic Hospice Demeter, the Netherlands
- 2Division of Internal Medicine and Dermatology, University Medical Center Utrecht, the Netherlands
- 3Department of Medical Oncology, University Medical Center Utrecht, the Netherlands
- 4Community Health Center De Bilt, the Netherlands
*Address for Correspondence: Everlien de Graaf, Academic Hospice Demeter, Weltevreden 3, 3731 AL De Bilt, the Netherlands, Tel: 31654394889; Fax: 31302202596; E-mail: e.degraaf@hospicedemeter.nl
Citation: de Graaf E, Zweers D, de Graeff A, Daggelders G, Teunissen S. Does Age Influence Symptom Prevalence and Intensity in Hospice Patients, or Not? A Retrospective Cohort Study. J Geriatrics Palliative Care 2014;S(1): 7.
Copyright © 2014 Graaf et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Geriatrics and Palliative Care | ISSN: 2373-1133 | Special Issue
Submission: 18 August 2014| Accepted: 25 September 2014 | Published: 29 September 2014
Reviewed & Approved by: Dr. Huai Yong Cheng, Associate Professor of General Medicine, Geriatrics and Palliative Care at University of Virginia, USA.
Abstract
Introduction: Elderly are a growing population in hospice care. Palliative- and hospice care is less accessible to elderly due to difficulty in marking the palliative phase and identifying palliative care needs.Aim: The aim of this study was to gain insight into symptoms of hospice patients of different ages, to improve hospice care for elderly.Method: A retrospective cohort study of patients admitted to a high care hospice facility from June 2007 to 2013 was conducted using prospectively collected data, from the first week after admission. Four age groups were selected: <65, 65-75, 75-85 and >85. The Utrecht Symptom Diary, a Dutch adapted translation of the Edmonton Symptom Assessment System, self-assessing the 12 most prevalent symptoms and (un)well-being on a 0 -10 numerical scale was used to collect data on symptom prevalence and intensity. Primary outcomes: symptom prevalence (score >0), and symptom intensity. Secondary outcomes: clinically relevant symptoms (score >3) and quality of life.Results: A total of 227 patients were included. Patients suffered from 6.3 symptoms concurrently. Of those 4.7 were clinically relevant. Fatigue was the most prevalent and intense symptom in all age groups, followed by dry mouth and anorexia. Pain was more prevalent and intense in patients <65 and anorexia was more prevalent in the oldest old. Quality of life was decreased for all ages, mean (un)well-being score 4.3 and most impaired for <65, (un)well-being score 4.72. Conclusion: Over 70% of all hospice patients were able to self-assess their symptoms. Little differences were identified, supporting the evidence that individualized hospice care is needed for all ages. Future research should focus on determination of appropriateness of the current set of symptoms for the oldest patients as well as exploration of the meaning of symptoms and underlying mechanisms in different age groups.Keywords
Elderly; Ageing; Hospice; Palliative care; Symptom; Intensity; Prevalence; AssessmentIntroduction
Worldwide, elderly become an increasingly important population for palliative care services, due to the aging demographics and increased treatment options. Elderly are less and later transferred to palliative- and hospice care, due to difficulties in palliative phase marking and identifying palliative care needs within the older population [1]. The World Health Organization defined palliative care as: “An approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual [2].” Older hospice patients differ from their younger counterparts in various aspects. Elderly have less cancer diagnosis and more comorbidity, therefore, symptoms and problems experienced by older hospice patients are hypothesized to be different [3]. To improve access of elderly patients and to enable healthcare professionals to provide optimal prevention and relief of symptoms, insight into specific symptoms of the aged population is needed [4]. Self-assessment is the gold standard to assess symptom intensity [5]. The Edmonton Symptom Assessment System (ESAS) is a worldwide recognized and validated tool to self-assess symptom intensity [6, 7]. A cutoff over three on the numerical scales indicates clinically relevant symptoms in need of interventions [8]. The last item of the ESAS is a single item (un)well-being measurement, showing good congruence with quality of life measurement tools [9].Early detection of symptom prevalence and monitoring of symptom intensity enables caregivers to anticipate on problems and treat symptoms in an early stage to prevent crises. Suitable application of assessment tools supports the communication between the patient, their families and professionals [10]. Research studies on symptoms in palliative care are mostly conducted within a relatively young advanced cancer population. A former study within an advanced cancer inpatient population found fewer differences than expected in symptom prevalence between different age groups [11]. In hospice care the patient population is more heterogenic due to different diagnoses and comorbidity causing different illness trajectories [12]. In the last three months of life hospitalization caused by symptom burden is more likely and increases towards death [13,14]. Towards the end of life the symptom-profile seems to be less stable [15]. Differences in symptom experience between age groups could therefore be clearer within the hospice population. Differences between age groups are hypothesized to be more prevalent and obvious in the hospice care population. Symptoms are more prevalent and more fluctuant during this last phase of life. Insight into the differences on symptom prevalence and intensity within age groups supports the ability of symptom recognition and anticipation in care and treatment by healthcare professionals providing more optimal symptom treatment and relief. The aim of this hospice study is to gain insight into symptoms of hospice patients of different ages, to improve hospice care for elderly.Methods
A quantitative retrospective cohort study with a cross sectional design, using prospectively collected data from a 11 point numerical scale collected during admission to a hospice facility. The data were collected from a database in June 2014.Setting and population This single center study was conducted in high care hospice facility in the center of the Netherlands, providing inpatient and outpatient care. The study population consisted of all adult inpatients, admitted to the hospice, from June 2007 to December 2013. Patients were categorized in four age groups: < 65, 65-75, 75-85 and > 85 years of age. Patients unable or unwilling to self-assess their symptoms were excluded from this research study. All patients were informed about research within our hospice facility and the ability to decline. None of our patients declined. Some patients were not able to use the self-assessment instrument and some were not willing to. Data were collected anonymous, using an electronic database, SYMPAL, where personal data are separated from other characteristics. Only the principal investigator could link data to individuals using a decryption key, separately stored within the database. The use of SYMPAL data for research queries was approved by the local ethics comity of the Utrecht University Medical Center.Data sources and measurement A Dutch adapted translation of the ESAS, the Utrecht Symptom Diary (USD), was used to asses symptom prevalence and symptom intensity. The instrument assesses the twelve most prevalent symptoms: pain, sleeping problems, dry mouth, dysphagia, anorexia, constipation, nausea, shortness of breath, fatigue, anxiety, depressed mood and confusion. The USD measures symptom intensity on a 0-10 point numerical scale. Patients can add four more symptoms if necessary. Finally, quality of life is assessed using a 1-item (un)well-being measure. The USD was filled out twice a week (standard care) and more often if clinically indicated. All USD were prospectively collected during hospice stay and entered in the SYMPAL database with patient- and illness characteristics. The SYMPAL database was specifically developed (2009) to collect data from palliative care patients in a diversity of palliative care settings. From the database the data of all hospice patients meeting the eligibility criteria were collected. Patient and illness characteristics were retrieved from the database and finally the USD data from all patients were imported from the database to a separate research file. Data from the first symptom assessment after admission were included. Symptom assessments, collected over 7 days after admission were excluded from this research study, symptom prevalence and intensity is hypothesized to be influenced by hospice care and treatment. Outcomes The primary outcomes of this hospice study were symptom prevalence and symptom intensity. A symptom was prevalent at admission when a patient scored one or higher at the USD. Symptom intensity was determined by the numerical USD score the patient gave per symptom. Secondary outcomes were: clinically relevant symptoms, number of concurrent symptoms and concurrent clinical relevant symptoms per patient, quality of life and patient characteristics. Clinical relevant symptoms were all USD symptoms scored over the cutoff of three. The number of prevalent symptoms and the number of clinical relevant symptoms per patient were calculated, adding all prevalent symptoms and all clinical relevant symptoms per patient. Quality of life was assessed using the USD (un)well-being item. Patient characteristics were gathered using demographics: age, gender, marital status and living situation. Illness related factors were determined by the primary diagnosis and phase of illness (treatment directed, symptom directed or dying phase). The patients’ performance status was assessed using the WHO score. Finally, admission time was concluded as the number of days a patient was admitted to the hospice facility and survival as the number of days from admission to death.Analysis The primary and secondary outcomes were analyzed using descriptive statistics. Group differences of symptom intensity, number of symptoms, number of clinically relevant symptoms and (un)well-being were analyzed using Kruskall Wallis, since the data did not meet the assumptions to perform an ANOVA analysis. The categorical data, symptom prevalence, clinically relevant symptoms, were analyzed using the Pearson Chi Square. Demographics were analyzed using ANOVA for continuous data or non-parametric if necessary, and Pearson Chi Square for categorical data. Statistical significance (two-sided) was set on p<0.05. Statistical software IBM SPSS 22 was used to analyze the data.Results
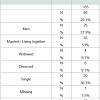
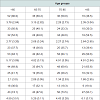
A total of 342 patients were admitted to the hospice facility from June 2007 to December 2013, 246 patients (71.9%) were eligible, having at least one USD measurement. 19 patients were excluded because of the lack of any USD measurements within the first week after admission. Data of 227 patients (66.4%) were included in the study, 87 were men (38%) and the median age was 74 (mean 71.7; 31-96; SD 12.782).Analysis of characteristics excluded patients showed significant differences between the eligible and non-eligible population. Patients unable or unwilling to self-assess symptoms were more likely to be over 85, or had a low WHO performance status, or a life expectancy less than 14 days, or a survival less than 14 days, or a short admission time (p<0.05).Demographics and illness characteristics Patients in diverse age groups did not differ significantly regarding overall patient characteristics and illness characteristics. However the difference in illness characteristics of the oldest old, over 85, shows a lower proportion of oncology as primary diagnosis. Demographics differed significantly in marital status. The living situation differed between groups: the oldest patients were more likely to be widowed and live alone, patients under 85 were more likely to live with a partner. Nevertheless, the availability of family caregivers did not differ over groups. Demographic and illness characteristics are shown in detail in Table 1. Hospice admission The admission duration and survival of patients differed largely in individual cases due to outliers in the quantity of days. The median admission time and survival of patients over 85 were longer than the other three groups, 28 days, however not significant (Table 1).Symptom prevalence On admission patients in hospice care suffered from 6.3 symptoms concurrently. Age groups differences were minimal, respectively 6.64; 6.33; 6.09 and 6.39 over the four age groups. The most prevalent symptom in all age groups was fatigue, with prevalence as high as 100% for the oldest old. The other symptoms relevant to all age groups were anorexia, dry mouth, pain, dysphagia and constipation. Pain is more prevalent in younger patients (0.001), anorexia is more prevalent in patient over 85 years of age (p=0.047). Details on symptom prevalence are presented in Table 2. Symptom intensity The symptom intensity scored on the USD was highest for fatigue. Dry mouth, loss of appetite, pain, constipation and sleeping problems had the highest intensities. Pain intensity scores differed significantly between groups. Pair wise comparisons showed a significant difference (0.007) between the age groups < 65 and 75-85. Symptom intensity for all USD symptoms is presented in Table 2.Clinical relevant symptoms At admission patients suffered from 4.66 symptoms scoring over the cutoff indicating clinical relevance for symptom treatment. The age groups show differences however small, scoring 4.83; 4.78; 4.49 and 4.57 respectively. Clinical relevant symptoms reveal a pattern within the age groups that is similar to the symptom prevalence. Fatigue is highly prevalent in the higher scores, as well as anorexia and dry mouth. Where pain, constipation and sleeping problems show, scores between 50% and 30% clinical relevance in all age groups. Pain is a more often clinical relevant for younger patients under 65. Anorexia is more often clinical relevant in patients over 85. Details on clinical relevant symptoms are presented in Table 2.Quality of life The quality of life at hospice admission is relatively low, showed by a (un)well-being score of 4.3. Over the different age groups the differences are minimal, non-significant, scoring respectively 4.72; 3.81; 4.26; 4.07.Discussion
Fatigue, dry mouth, and anorexia are the most prevalent, intense symptoms and clinically relevant for all hospice inpatients on admission. Nevertheless differences of symptoms were shown in pain, being more prevalent and intense in patients under 65 years of age and anorexia being more prevalent in the oldest patients. The mean number of symptoms is approximately constant over all age groups as are the number of clinically relevant symptoms. This study was performed retrospectively, but the strength is that the data from the USD were collected prospectively of all in patients over six years. A limitation is that patients who were unable or unwilling to fill out an USD were excluded. Analysis of patients’ characteristics showed a specific subgroup of hospice patients of whom we have no information on their symptoms. Due to the specific characteristics this group appears to be divided in two subgroups, the very ill patients and very old patients over 85 years of age. Therefore the results of this study are probably an underestimation of the real overall symptom prevalence, intensity and quality of life. Although patients were all inpatients from one high care hospice facility, basic characteristics of hospice patients in the Netherlands show a good resemblance. The number of patients in this study increases the generalizability of these results. Although, differences in cultural and organizational aspects of hospice care over the world should always be taken into account. Overall approximately 70% of all hospice patients were able to self-assess their symptoms. Of the oldest and severely ill patients much less patients were able to do so. Therefore future research should focus on the development and validation of assessment tools individualized to elderly and proxy assessments, as their symptoms are most likely to differ from the other subgroups. Clinical experience has indicated that patients find it hard to express their feelings, the intensity of a symptom, in a figure. Historically other options were tried, using a visual analogue scale initially and faces scales for some specific symptoms like pain or anxiety. The current health and interactive innovations like apps and personalized web based support could be an option to help patients self-assess their symptoms more easily, using numerical scales with visual support of the figures. Further research should focus on exploring which support patients prefer. Pain is a lesser problem in elderly; this is in concordance with other research studies on symptoms in a cancer population [16]. Anorexia is more problematic in the oldest patients, over 85. Older patients suffer from at least as many concurrent symptoms and clinically relevant symptoms as their younger counterparts do. This is supported by the similar indication of reduced quality of life scores and previous research in cancer patients [11, 16]. Hospice and palliative care needs and problems are at least as prevalent and intense in elderly as in their younger counterparts. This means that elderly patients and even the oldest old deserve a similar approach of personalized systematic monitoring of symptoms and problems to reach individualized total care. The challenge of future research is to explore if the current set of symptoms is fully appropriate for the oldest patients and to discover the meaning of symptoms and explore underlying mechanisms in different age groups, to optimize personalized support and symptom treatment, reduce symptom prevalence and intensity and improve quality of life and death for all hospice patients.Conclusion
Over 70% of all hospice patients were able to self-assess their symptoms while admitted to a hospice facility. The oldest patients were significantly less able to assess their symptoms, as were the very ill patients. Hospice patients suffer from 6 to 7 symptoms concurrently. Fatigue, dry mouth and anorexia are most prevalent and intense. Patients under 65, suffer from pain more often and more intense where the oldest patients, over 85, suffer from anorexia more often. Concurrently almost five symptoms score over three, the cutoff for clinically relevant symptoms. The quality of life is limited, scoring between 3.8 and 4.7 for wellbeing on the USD. Although elderly and very ill were underrepresented within the research population, their problems were just as intense as their younger counterparts, indicating the need for personalized hospice care for all patients. There is no further need for future research in the hospice population to focus on differences in symptom burden between different age groups. There is an urge for a creative collaboration between geriatric and palliative care specialists together with general practitioners to develop research models to determine clinical significant themes of hospice care in the ageing population.Acknowledgements
We would like to express our thanks to the patients who took part in this study and the staff at Academic Hospice Demeter who made it possible.Funding
This research study was funded by Academic Hospice Demeter and the Francinus de Wind foundation.References
- Evans N, Pasman HR, Deeg D, Onwuteaka-Philipsen B, on behalf of EURO IMPACT (2014) How do general end-of-life treatment goals and values relate to specific treatment preferences? A population-based study. Palliat Med.
- World Health Orgnization (2002) WHO definition of palliative care.
- Addington-Hall J, Altmann D, McCarthy M (1998) Variations by age in symptoms and dependency levels experienced by people in the last year of life, as reported by surviving family, friends and officials. Age Ageing 27: 129-136.
- Teunissen SCCM, Wesker W, Kruitwagen C, De Haes HCJM, Voest EE, et al. (2007) Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manage 34: 94-104.
- Nekolaichuk CL, Maguire TO, Suarez-Almazor M, Rogers WT, Bruera E (1999) Assessing the reliability of patient, nurse, and family caregiver symptom ratings in hospitalized advanced cancer patients. J Clin Oncol 17: 3621-3630.
- Claessens P, Menten J, Schotsmans P, Broeckaert B (2011) Development and validation of a modified version of the Edmonton Symptom Assessment Scale in a Flemish palliative care population. Am J Hosp Palliat Care 28: 475-482.
- Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7: 6-9.
- Oldenmenger WH, de Raaf PJ, de Klerk C, van der Rijt CC (2013) Cut points on 0-10 numeric rating scales for symptoms included in the Edmonton Symptom Assessment Scale in cancer patients: a systematic review. J Pain Symptom Manage 45: 1083-1093.
- Bush SH, Parsons HA, Palmer JL, Li Z, Chacko R, et al. (2010) Single- vs. multiple-item instruments in the assessment of quality of life in patients with advanced cancer. J Pain Symptom Manage 39: 564-571.
- Pereira J, Green E, Molloy S, Dudgeon D, Howell D, et al. (2014) Population-based standardized symptom screening: Cancer Care Ontario's Edmonton Symptom Assessment System and performance status initiatives. J Oncol Pract 10: 212-214.
- Teunissen SC, de Haes HC, Voest EE, de Graeff A (2006) Does age matter in palliative care? Crit Rev Oncol Hematol 60: 152-158.
- Lynn J, Adamson DM (2003) Living well at the end of life. Adapting health care to serious chronic illness in old age 2003.
- Abarshi E, Echteld M, Van den Block L, Donker G, Deliens L, et al. (2010) Transitions between care settings at the end of life in the Netherlands: results from a nationwide study. Palliative Medicine 24: 166-174.
- Costantini M, Higginson IJ, Boni L, Orengo MA, Garrone E, et al. (2003) Effect of a palliative home care team on hospital admissions among patients with advanced cancer. Palliat Med 17: 315-321.
- de la Cruz M, Noguera A, San Miguel-Arregui MT, Williams J, Chisholm G, et al. (2014) Delirium, agitation, and symptom distress within the final seven days of life among cancer patients receiving hospice care. Palliat Support Care 20: 1-6.
- Morita T, Kuriya M, Miyashita M, Sato K, Eguchi K, et al. (2014) Symptom burden and achievement of good death of elderly cancer patients. J Palliat Med 17: 887-893.