Journal of Geriatrics and Palliative Care
Download PDF
Research Article
Management Patterns of the Older Population with Cancer during The Early State Of Alarm In the Valencian Autonomous Community: The GIDO GERICOV-2020 PROJECT
Gironés R1*, Paredero I2, Arnal M2, Puchades C1, Rodríguez P3, García J4, Torregrosa M5, Melián M6, Aparisi F7, Climent MA6, Maestu I5, de Julián M6, Salvador C8, Sandiego S6, Gómez N1, Soriano D1, Ávila C8, Domingo B1, Ferrero A1, Blanch S6, Perea J1, Sánchez A2 and Juan O1
1Medical Oncology Service. Hospital Universitari i Poltècnic La F.: Valencia
2Medical Oncology Service. Hospital Provincial de Castellón. Castellón
3Medical Oncology Unit. Hospital Virgen de los Liros Alcoi. Alicante
4Medical Oncology Service. Hospital Arnau de Valencia. Valencia
5Medical Oncology Service. Hospital Universitri Doctor Peset . Valencia
6Medical Oncology Service. Fundación Instituto Valenciano de Oncología. Valencia
7Medical Oncology Unit. Hospital de Requena. Valencia
8Medical Oncology Unit. Hospital de Xàtiva. Valencia
*Address for Correspondence:
Gironés R, Medical Oncology Service Hospital, Universitari, i Poltècnic, La F.: Valencia, Spain Email: reginagiro@hotmail.com
Submission: 28 October, 2021
Accepted: 22 March, 2022
Published: 28 March, 2022
Copyright: © 2022 Sarrió RG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
In the current care scenario of the COVID-19 pandemic, older oncology patients are especially vulnerable and find themselves facing a double threat. On the one hand, the risk of contracting an infection that we still know little about facilitated by immunosuppression and potentially aggravated by the antineoplastic treatment toxicity, co-morbidities, and the cancer severity [1]. On the other, the neoplastic disease itself, along with the risk of losing an opportunity because of the reduction of medical cancer care, due to the limitation or re-allocation of resources [2]. Therefore, one priority aspect is establishing the individual risk associated with the neoplasm and the treatment, in the context of each type of oncological patient [3]. Although cancer is assumed to be an adverse prognostic factor in patients with COVID-19 and in older persons, there is still uncertainty and a lack of robust evidence. Recommendations have surged concerning therapeutic decisions in oncology patients, and the records of cancer patients with COVID. Nevertheless, the real impact of therapeutic decisions in clinical practice remains unknown, especially in the older patient group as well as the evolution of this population group.
To increase the available evidence in the current pandemic, we aimed to retrospectively record the management of patients 70 years and older with cancer who received care in the Medical Oncology services of the hospitals belonging to the GIDO group during the early pandemic.
Keywords
Cancer; Neoplastic disease; Covid-19; Immunocompromised
Objective
To increase knowledge regarding this population, we planned to retrospectively analyse patients with cancer aged 70 year or older that had been assessed in the Medical Oncology service of the Hospitals belonging to the GIDO group: Group for Investigation and Divulgation in Oncology.
Introduction
On 14th March 2020, a state of alarm was declared in Spain [4]. A COVID-19 infection is a threat for oncology patients, immunocompromised by definition, owing to their neoplasia and the treatments administered to treat it [5-8]. The risk/benefit balance that is always considered during the treatment of an oncology patient has become exceptionally complex during the COVID-19 pandemic. Both older patients and patients with cancer have a greater risk of infection and mortality due to the COVID-19 infection [9]. During this situation, multitudes of recommendations have arisen, not only how to avoid the infection and for its management, but also in making decisions regarding active treatment in the oncology population. In general, the recommendations agree in maintaining adjuvant indications despite the threat of COVID-19 infection during treatment [2,8]. The decisions concerning the population with metastases are more contradictory, because while there is a risk of infection, delays in palliative treatment may allow the basal status of the patient to deteriorate and cause a loss of the therapeutic window [2]. Delays should also include the evaluation of the increased risk of admission for the management of palliative symptoms during a situation when available resources are scarce [2,8]. With the arrival of the pandemic, new methods of communication with patients have been implemented, promoting the use of telephone contact and reaching an agreement with patients regarding delays, cancellations, or administration of treatment. In summary, we find ourselves in a challenging situation regarding therapeutic decisions for the oncology patient, proposing how and when to provide cancer treatment during this time [3].
Materials & Methods
Study Design & Participants:
A retrospective observational study was designed to collect online data from the Medical Oncology service of the hospitals integrated in the GIDO. Patients with outpatient services booked were identified for the period 16th March 2020 to 31st March 2020, including patients that were being followed-up and those that were receiving active treatment. Planned first consults during the data collection time period were also included. Patients 70 years or older at the time of inclusion were included.Data were collected from electronic clinical histories, including
demographic and clinical characteristics.
The project objective was to determine the relationship between
the older outpatient population with cancer and COVID infection,
and, in particular, to describe the management patterns of this
population during the first weeks of the state of alarm.
Here, we present the second part of the project, in which we
analyse the treatment of the sample population both in terms of
follow-up and active treatment.
This study was approved by the Research with Medicines Ethics
committee of the University and Polytechnic Hospital La Fe and
classified by the Spanish Medicines Agency as an Observational Study
No Post-Authorization (NO-EPA, as per the Spanish abbreviation)
Informed consent for voluntary participation was requested from
the patients, allowing consent to be provided via phone call to avoid
hospital contact. The definition of COVID contact or infection was
collected from the clinical history.
Statistical Analysis:
For the descriptive analysis, continuous variables were presented
as means with standard deviation or medians with the corresponding
interquartile range (IQR), depending on which was the most
appropriate for each case. Categorical variables were presented as
numbers and percentages (%). Potential risk factors and associations
with COVID infection were explored using the Cox proportional
model with hazard ratio and the corresponding confidence interval
(HR 95%CI). All statistical analyses were conducted using SPSS
Statistics version 21.0 (IBM: New York, NY). A p-value <0.05 was
considered as statistically significant.Results
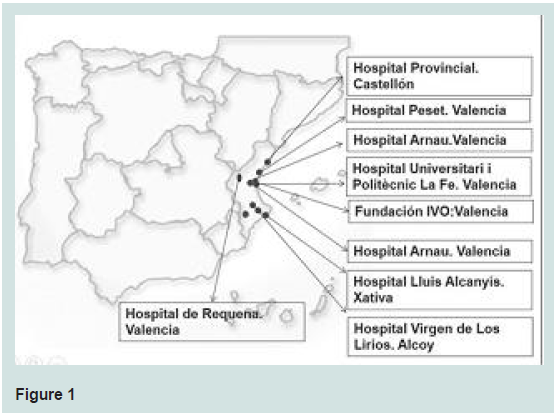
Following the required approvals, 13 Researchers from 9 hospitals
in the Valencian Autonomous Community participated (Figure 1). In
total, data were analysed for 1127 patients that were included for the
period 16 March 2020 to 31 March 2020.
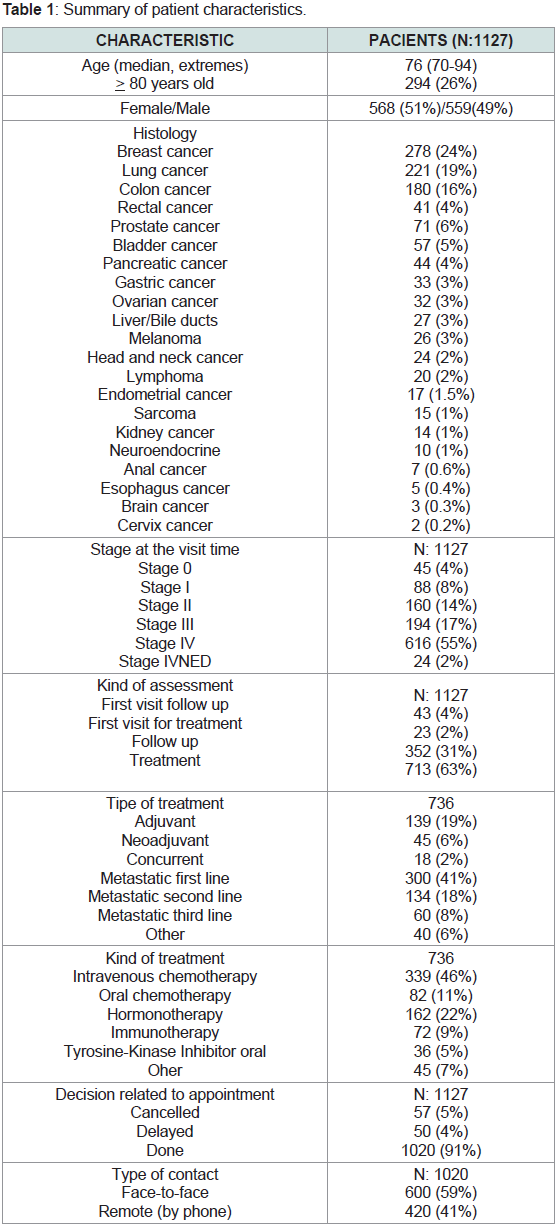
Demographic Characteristics:
The median age was 76 years (70-94). Patients 80 years and older
comprised 26% of the study sample. The gender distribution was
even (51% women). Breast cancer predominated (24%), followed
by lung cancer (19%), and colon cancer (16%). The demographic
characteristics and histological distribution are shown in the Table 1. The majority of the patients (55%, 616) had stage IV at the time
of their appointment. 63% of appointments were for treatment
administration, and 35% of first appointments (66 total) were also
for treatment administration. Appointments were kept for 91% of the
patients (1020), and more than half were face-to-face consults (600,
59%).Demographic Characteristics between Both Types of Populations:
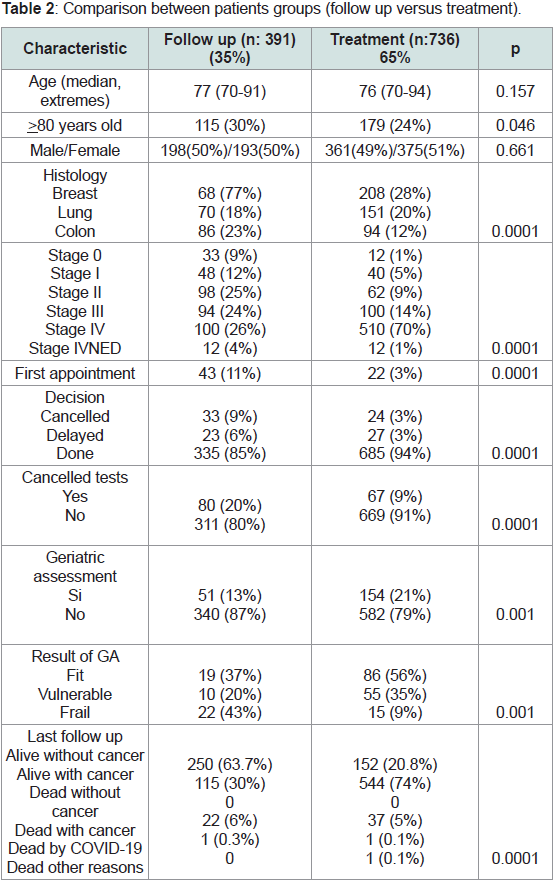
The demographic characteristics of both groups are compared
in Table 2. Over half (736 patients, 65%) of the patients included
were receiving active treatment compared with 35% (391 patients) that were being followed-up. Overall, no significant differences were
detected between groups for median age (77–76, p=0.157). Although
the population 80 years and older were more likely to be found in
the follow-up group (p=0.045). In terms of histological subtype, more
patients with breast cancer and lung cancer were receiving active
treatment compared to a larger number of patients with colon cancer
who were being followed-up (p=0.0001). More patients receiving
active treatment had stage IV (70% versus 26%, p=0.0001). More first assessments for follow-up than for treatment were conducted (11%
vs. 2%, p=0.001). More visits were cancelled in the follow-up group
than in the active treatment group (p=0.0001).Management Patterns in the Active Treatment Group:
Out of 736 patients receiving active treatment, 139 (19%) were
for adjuvant therapy, 18 (2%) concomitant therapy, and 40 (5%)
neoadjuvant therapy. The patients with metastatic disease (539,
74%), 300 received first-line treatment, 134 second, and 60 third-line
metastatic treatment. In terms of treatment type, 22% (162) were being
treated with hormonotherapy, 82 (11%) oral chemotherapy, 71 (10%)
immunotherapy, and 339 (46%) with intravenous chemotherapy.
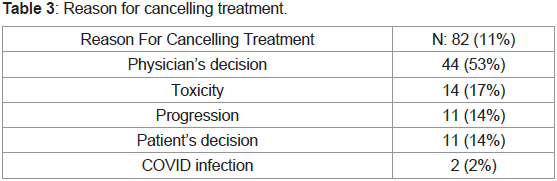
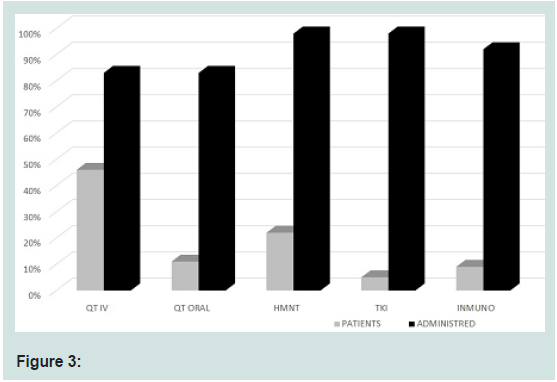
Around 5% (36) were receiving oral tyrosine kinase inhibitors.A. Treatment Modification
Out of the 736 patients in active treatment, the treatment regimen
was modified in 190 (26%) cases. Of these 190 cases, 82 cases had
treatment cancelled (43%), 19 had a reduction in dose (10%), and
89 cases had treatment administration delayed (47%). In total, the
administration of treatment was suspended in 11% of the patients
included in this study, delayed in 12%, and a dose reduction in 3%
(Figure 2). In the cases whose treatment was suspended (82), in 53% this decision was made by the physician; in 17% of cases due to
toxicity, 14% due to progression, and in 14% this decision was the
patients. In 2 cases (2%), treatment was suspended due to COVID-19
infection (Table 3). The probability of suspending treatment did
not correspond with older age, or with being older or younger
than 80 years, nor gender, nor the planned appointment date. No
correlation was found with histological subtype. It was correlated
with stage, with treatment suspended in the patient group with stage
IV (p=0.001). More treatment was cancelled among patients with
metastatic disease who were receiving second or third-line treatment
(p=0.001). In terms of type of treatment administered, treatment
was continued in 98% of patients receiving hormonotherapy, 83% of
intravenous chemotherapy, 92% of immunotherapy, and 83% of oral
chemotherapy (Figure 3).
B. Type of appointment
In the group of patients receiving active treatment, 25
appointments were cancelled (3%), 27 (4%) were delayed, and the
appointment was maintained in 93% of cases (684). 500 in-person
appointments were conducted, and 27% (184) were conducted
via telephone. The probability that an appointment was cancelled
correlated with histology (more appointments were cancelled among
those with breast or colon cancer), with stage (more appointments
were cancelled or delayed among patients with stage IV). No significant
correlation was found with treatment indication (adjuvant, stage IV,
etc.). More visits were cancelled for first-line metastatic treatment
(p=0.0001), (not with age, no with those older than 80 years, nor
gender, nor appointment date, appointments were not cancelled for
hormonotherapy, intravenous chemotherapy, immunotherapy, nor
oral chemotherapy).
The use of telephone contact was related with older age
(p=0.0001). In terms of telephone contact, 47% was in those older
than 80 years vs. 26% in those younger than 80 years (p=0.0001).
Telephone contact also predominated among women (38%) vs. 23%
(p=0.001). A significant correlation was also observed for its use
among patients with breast cancer (46% of contact via telephone
was for patients with breast cancer). No correlation was found with
appointment date. More telephone contact was used in the initial
stages of hormonotherapy treatment, but no telephone contact was
used in the population treated with intravenous or oral chemotherapy,
or immunotherapy.
C. Cancellation of complementary tests
In 67 cases, complementary tests were cancelled during the
period analysed (9%). In more than half the cases (39, 58%), the test
cancelled was a CT scan. In 2 cases elective surgery was cancelled, as
well as 16 analytical tests, and 7 mammograms.
The cancellation of tests was not correlated with age or gender.
More exploration tests were cancelled among patients with breast
and lung cancer. Although no statistically significant relationship
was detected, more tests were cancelled during the early days of the
state of alarm declaration. More tests were cancelled among patients
with advanced stages (p=0.005), and patients receiving intravenous
chemotherapy (p=0.023).
D. Geriatric assessment
In the group receiving active treatment, a geriatric assessment had been conducted at some point in 154 patients (21%). 14 cases were frail (9%), 54 pre-frail (35%), and 86 robust (56%).
Situation at the Final Evaluation:
At the final study evaluation, one patient had died due to COVID
(0.1%), 37 had died due to cancer (5%), and 1 had died due to other
causes (0.1%). 544 were still alive with neoplastic disease (74%), and
152 alive without neoplastic disease (20.8%).Characteristics of the Follow-Up Population:
A. Type of appointment:
Of the 391 patients receiving follow-up care, 32 appointments
(8%) were cancelled, 23 (6%) were delayed, and the appointments
remained the same for 86% (336 patients). Telephone consults were
conducted for 238 cases compared to 98 in-person appointments
for those in follow-up care (71% vs. 29%). There were no differences
for in-person appointment or telephone appointment based on age;
however, telephone appointments were more frequent for women
(76% of telephone appointments among females vs. 63% in males,
p=0.04). In terms of histology, telephone check-ups were more
frequent in those with breast cancer (79% vs. 21%), followed by colon
cancer (65%), and lung (60%) (p=0.006). In-person or telephone
appointments varied during the initial days of the state of alarm
(Figure). In-person or telephone contact was not affected by stage at
the time of follow-up.Appointment cancellation was not correlated with age or gender.
Cancellation was also not correlated with histology: colon cancer
(14%, p=0.003) vs. breast (3%) or lung (7%). More appointments
were cancelled in stage II during follow-up care (Figure, p=0.002,
17% vs. 8% in stage IV).
B. Cancellation of complementary tests
In the group receiving follow-up care, tests were cancelled for 80
patients (20%). More tests were cancelled in the group of 80 years or
older (25% vs. 18%, p=0.095). There were no differences by gender
(23% among women vs. 18% among men, p=0.176). No differences
were observed according to histology (23% breast, 23%, colon, 20%
lung). More tests were cancelled for patients with stage II (25%) that
for those with stage IV (18%) (p=0.03).
C. Geriatric assessment
In the group of patients receiving follow-up care, 50 patients
(13%) had undergone geriatric assessment: 14 cases were frail (42%),
10 pre-frail (20%), and 19 robust (38%). In terms of conducting a
geriatric assessment, there were no differences for age; however, more
geriatric assessments were conducted among males (p=0.003)(7% vs.
18%), more among patients with lung cancer (p=0.0001)(27%) and
colon cancer (14%).
D. The situation at the final evaluation
At the time of the final evaluation, in the group receiving followup
care, 1 patient had died due to COVID (0.3%), 22 had died due to
cancer (6%), 115 were still alive with cancer (30%), and 250 were still
alive and cancer-free (63.7%).
Discussion
On the 14th of March 2020, a state of alarm was declared in Spain [4]. Older persons, with co-morbidities, such as cancer, were
considered especially susceptible to suffering from the infection and
its effects, with a higher probability of a fatal outcome than for other
populations, given their immunosuppressed state, both due to the
neoplasm and the treatment [1,2,10]. Given the potential infection
risk that hospitals and medical centres supposed, many scientific
associations released management recommendations for patients
with cancer, in particular, focusing on avoiding frequenting hospitals
[5-7]. Despite this, the majority of societies and cooperative groups
did not initially include recommendations for the management of
the older population group. In fact, French authorities proposed an
age limit of 60 years for postponing cancer treatments, irrespective of
whether the indication was curative or palliative [13-15]. Initially, only
an opinion article published in the Journal of Geriatric Oncology was
available [1], which suggested that older patients with cancer should
not be systematically excluded from active treatment. Subsequently,
the International Society of Geriatric Oncology (SIOG) declared that
chronological age was not an exclusion criterion for treatment in
this population and published their management recommendations
[2]. Therefore, older patients with cancer found themselves in a
situation at risk of being excluded from diagnostic, treatment, and
follow-up processes to protect their health during the pandemic.
Nevertheless, early on during the pandemic, no recommendations
existed in our environment, and therefore each centre, service, and
physician had to make decisions based on their own criteria, which
changed depending on the progression of the infection. Neither has
the actual management of older patients with cancer been published
retrospectively, at least in our environment.
We present the first study with data of older patients with
cancer in eight hospitals of the Valencian Autonomous community,
which collates the management patterns of this population. The
management of 1127 patients 70 years or older with cancer, seen
between 16th of March 2020 and 31st March 2020, are presented. This
manuscript deals with an older population, with 26% over 80 years
of age (currently considered “the oldest old”) [11]. The data analysis
demonstrates that oncogeriatrics is a reality, with an elevated number
of older patients evaluated in consults during this period, also bearing
in mind that the week of the 16th of March was a week of bank
holidays in many places. We were unable to compare the percentage
of the older population with adults due to a lack of records. The most
frequent cancer types were breast, lung, and colon, more than half
(55%) had stage IV, and 63% were receiving active treatment. Despite
the adversity of the situation, active treatment was maintained in 74%
of patients, cancelled in 11%, delayed in 12%, and modified in 5%.
The probability of cancelling treatment was related with cancer type
(breast and colon) and with stage IV. Very few appointments were
cancelled, and a third of them were via telephone (older patients with
breast cancer and oral treatment). The cancellation of exploratory
tests in the treatment group was low (<10%). However, on the patient
group receiving follow-up care, the majority of the appointments
were changed to telephone consults (women with breast cancer) and
more exploratory tests were cancelled (20%). None of these actions
appeared to be correlated with an increased or decreased risk of
COVID-19 infection.
The evidence extrapolated from the collected data suggests that
the administration of active treatment was safe during the first weeks of the state of alarm. The number of cancelled treatments was low,
and especially correlated with indications for palliative treatment.
In terms of follow-up care, the majority of consults were remote.
Consults were prioritised, with first visits maintained as well as those
consults in particular with pathologies that were not able to be delayed
or those whose treatment intent was palliative-curative. Telephone
consults were promoted, when appropriate, to avoid patients coming
to the hospital and increasing their risk of infection. In terms of
treatments, different modifications were made to minimize the risk
of infection.
The pandemic and state of alarm has raised the need for rapid
adaptation to oncology care. Despite the many recommendations
aimed at minimising patient’s attendance in the hospital,
antineoplastic treatment should not be delayed [10]. The general
perspective in the various clinics was quite homogenous for the older
patient population with cancer, with few cancellations and treatment
delays. Although our data may be biased owing to the initial low
detection of asymptomatic cases, and because the participating
hospitals were not the most affected by COVID infection in our
environment. The oncology services that included cases did not
cancel or shut down their service, and were therefore able to continue
providing care, and in general, maintained their care provision. In
contrast, our data showed that consults were suspended in palliative
and advanced cases, where the benefit in this population is not clearly
demonstrated. Chronological age is not a good parameter to base a
decision for cancelling or not a consult or oncological treatments
that have been demonstrated as beneficial in this population [2].
The approach via geriatric or frailty assessment may assist in the
assessment of global health status in these patients and help to
personalise therapeutic plans, although in our environment geriatric
assessments are not widely used. Although oncogeriatrics is a reality,
our data show relatively low use of the geriatric assessment in the
management of this population (26%). Given the scarce number of
assessments, no significant relationships were able to be established.
In conclusion, during the first weeks of the pandemic and state of
alarm, in 8 medical oncology services of the Valencian Autonomous
Community, provision of care was able to be maintained for patients
receiving active treatment, and the majority of those receiving followup
care had their appointments changed to remote telephone consults.
Specific types of patients (breast cancer, hormonal treatment, colon
cancer receiving follow-up care) appear to have an ideal profile for
reducing the load of in-person appointments and promoting remote
consults as an alternative.