Journal of Geriatrics and Palliative Care
Download PDF
Research Article
*Address for Correspondence: XinQi Dong, Professor of Medicine, Nursing and Behavioral Sciences Director, Chinese Health, Aging and Policy Program Associate Director, Rush Institute for Healthy Aging, Rush University Medical Center, Chicago, Illinois, USA, Tel: 312 942 3350; Fax: 312 942 2861; E-mail: xinqi_dong@rush.edu
Citation: Dong X, Su D. Epidemiology of Physical Function Impairment in Global Chinese Aging Population: A Systematic Review. J Geriatrics Palliative Care 2016;4(1): 23.
Copyright © 2016 Dong X, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Geriatrics and Palliative Care | ISSN: 2373-1133 | Volume: 4, Issue: 1
Submission: 22 February 2016 | Accepted: 26 April, 2016 | Published: 3 May 2016
Background: Physical function is a cornerstone of geriatric medicine. Impairment in physical function may threaten one’s ability to live independently and is associated with multiple negative health outcomes. Although Chinese people is one of the fastest growing populations in the world, there is a limited understanding of the epidemiology of physical function impairment in the global Chinese aging population.
Methods: Researchers used the PRISMA statement and performed a comprehensive online search to highlight the global epidemiology of physical function impairment of Chinese older adults in terms of prevalence, incidence, risk and protective factors, and health consequences. Search items include Chinese, older adult, Asian elderly, aging, physical function, physical function impairment, disability, function impairment, functional dependence, functional limitation, mobility, ADL, IADL, Nagi, and Rosow-Breslau.
Results: Eighty-two papers met inclusion criteria. Prevalence of ADL impairment ranges from 3.0% to 11.6%, while prevalence of IADL impairment ranges from 7.9% to 50.2%. Common risk factors include older age, female gender, lower education, lower income, rural residences, unmarried status, chronic diseases, depression/depressive symptoms, cognitive impairment, and falls. Health outcomes include suicidal ideation/attempted suicide, depression/depressive symptoms, cognitive impairment, falls, and mortality.
Conclusion: The prevalence of physical function impairment among Chinese aging population varies across regions and the number of physical function impairments increases over time. Physical function is influenced by multiple aspects, including socio-demographic characteristics, health conditions, and health behaviors, and can lead to adverse health outcomes. Future longitudinal research is necessary to explore the regional differences, effectiveness of existing intervention programs, as well as the cultural contexts of physical function impairment. Concerted support from caregivers, healthcare and social service providers, and policy makers is necessary to improve physical function and promote healthy aging among Chinese older adults.
Understanding physical function in Chinese older adults is important. According to the 6th Chinese National Population Census in 2010, the proportion of Chinese older adults aged 60 and above within the general population has increased from 8.0% to 13.3% within 20 years [22] and is projected to reach 19.3% by 2025 [23]. By 2050, it is estimated that 25% of the world’s aging population will beChinese [24]. As one of the fastest growing aging populations in the world [23], the Chinese older adult population may experience a great risk of physical function impairment, which is a serious social and public health concern. However, while many studies have been done in western countries to examine physical function among older adults, little is known in the Chinese aging population, especially among overseas Chinese population. Integrating existing information about physical function impairment among different Chinese communities can help to provide population estimates for the older adults in China and globally, as well as to direct future study and policy making.
The possible differences and similarities of physical function impairment between Chinese aging population and other racial groups warrant attention. Cultural differences may shape the understanding of disease prevention, health maintaining, and treatment [25]. In addition, genetic factors, life style, health care disparities may also partially contribute to the varied health status across different racial groups [26,27]. There is growing evidence reported that U.S. immigrants have poorer physical function compared to their US born counterparts [28]. Research has indicated worse physical health among Asian Americans compared to non-Hispanic white, and Chinese subgroup has the highest rate of prevalence of limitedphysical function compared to other Asian subgroups [29]. Chinese immigrant aging population may face a higher risk of poor health status due to cultural and linguistic barriers, social isolation, healthcare disparities, and acculturation [27]. Evidence has also suggested that relocation and loss of native support network might lead to health disparities among Chinese population [30-34]; the distress of being old combined with immigration-related barriers may make Chinese immigrant aging population even more vulnerable [35]. Furthermore, Chinese aging population may be impacted by barriers of access to health care including language, help-seeking behaviors, and traditional Chinese thinking [25,36], which may lead to delayed care and treatment, and increase the likelihood of having hysical function impairment.
Although risk/protective factors and health consequences of physical function impairment in general aging population has been identified in prior studies [9,13,19,37-48], the situation may differamong Chinese older adults due to a variety of socioeconomics, culture beliefs, health literacy, available social services, and access to healthcare resources [49]. Additionally, given the unique cultural characteristics of Chinese population, older adults may expect more care and support from family members, known as “filial piety” [50], especially for those have difficulty in daily task performance. Prior research suggested that a higher level of filial piety is associated with better self-rated health for older adults [51]. However, providingcaregiving is likely challenging for immigrant adult children due to cultural and linguistic barriers. Furthermore, Chinese older adults who suffer physical function impairment may face potential elderabuse and discrimination from others [20,52]; additionally, poor health or disability can be especially stigmatized in Chinese culture [21]. These cultural components play important roles which may mediate the relationships between physical function impairment, its risk/protective factors, and health outcomes. Moreover, looking at physical and functional impairment among Chinese aging population across countries and geographic areas can help us understand differences and similarities between populations and provide more comprehensive and better focused recommendations for health promotion. Last, understanding the epidemiology of physical function among Chinese older adults may effectively direct the allocations and uses of limited health care and social-care resources, as well as the development of future strategy at both macro and micro levels.
Despite the increasing awareness on physical function impairment among older adults, there has not been a systematic review of physical function impairment in global Chinese aging population. The purpose of this review is to improve our understanding of the epidemiology of physical function impairment among the global Chinese population including its prevalence, incidence, risk and protective factors, and health consequences, and also aims to collect evidence and extract information for directions for future research and health policy.
Prevalence
Prevalence of older adults’ physical function impairment varies across different Chinese communities depending on the setting, research methods, and measurements. Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) limitations are most commonly measurements used to assess one’s physical function. The majority of studies used “difficulty in completing at least one item of daily tasks” as the cut-off point of ADL or IADL impairment [53-55]. The rates of ADL impairment ranged from 3.0% to 11.6% among global Chinese communities [23,29,56-64], while the rates of IADL impairment ranged from 7.9% to 50.2% (Table 1) [23,29,56,57,61]. Further, the prevalence of physical function impairment was relatively higher among Chinese population compared to other ethnic or racial groups. For example, the National Health Interview Survey of 738 Asian American older adults suggested that the Chinese subgroup experienced the highest ADL or IADL disabilities (11.6% ADL vs. 17.3% IADL impairment) compared to other subgroups of Asian Americans (Filipino: 8.3% ADL vs. 15.3% IADL impairment; Asian Indian: 4.6% ADL vs. 9.1% IADL impairment) [29]. Additionally, studies also report that Chinese older adults living in Chicago had a higher prevalence of IADL impairment in comparison with other Chinese older adults in Mainland China [23,56,61]. In addition to ADL and IADL measurements, researchers have used other assessment tools to evaluate Chinese older adults’ physical function, such as Nagi index of basic physical activities and Rosow and Breslau index of mobility [56,65]. A recent paper documented that the rate of self-reported mobility disability was 8.9% in males and 8.5% in females among 616 community-dwelling older adults aged 60 or above in Chengdu and Suining [58], while another paper reported that the rate of low skeletal muscle mass was 9.55% in males compared to 6.63% in females based on a survey of 432 older adults aged 65 or above in Yanqing [66].
Incidence
Most papers reported that an increasing proportion of older adults experience physical function impairment over time (Table 2) [61,67-70]. For instance, the Chinese Longitudinal Healthy Longevity Survey, a four-year follow-up study of 11,112 older adults acrossChina, reported that the rate of ADL disability onset was 9.67% [67]. Additionally, these trends may differ by gender. A communitydwelling study conducted in Beijing reported that the ADL disability increased by 0.96% per year for males over a 15 years follow-up, while declining by 1.15% per year for females [70].
In terms of demographic factors, older age, female gender, lower socioeconomic status, and lower education levels are common risk factors of physical function impairment among Chinese older adults (Table 3) [23,29,54,56,60,61,64,65,71-84]. Previous research among Chinese older adults documented that older age was significantly associated with higher risk of physical function impairment [23,29,56,60,65,71,77,78,80-83]. Interestingly, a study of 7,845 Chinese older adults found that young-old older adults (60-69 years old) experienced higher severity of ADL impairment compared to an older subgroup (70 years old and above) [54]. Additionally, gender is another widely discussed predictor of physical function impairment; multiple studies indicated females are more likely to suffer physical disability or other ADL/IADL difficulties than males [29,54,56,65,71-75,82,84]. Further, two studies reported that older adults with lower socio-economic status or lower income have a higher proportion ofworsening functional status [61,80], while another study concluded that absolute income is not an important predictor of functionaldependency [85]. Moreover, higher self-rated financial adequacy wasreported to indicate better physical health [84]. With respect to the level of education, Chinese older adults with lower education levels were correlated with higher possibility of ADL and IADL impairment, or mobility decline [56,60,61,65,81,83]. One study further indicated that an individual with a lower education level was more likely to have early-onset functional limitation [82].
With respect to location and immigration status, risk factors include living in a rural area, larger Chinese community, and living in the U.S. for more years [23,54,56,71,78,84]. Three studies from Mainland China indicated the difference of functional disabilities between rural and urban residents [23,54,78]. Compared with respondents living in urban areas, older adults living in rural areas had higher disability rates for all age groups [23,54]. One study found that rural residence was associated with ADL limitation among female participants [78]. In contrast, a study indicated that living in a rural area could lead to a less rapid increase in ADL difficulties [71]. Additionally, one study among 2,272 Chinese Canadian population reported that residing in communities with a smaller Chinese population was associated with better physical health [84]. In terms of immigration status, results based on a community-dwelling population of U.S. Chinese older adults indicated that having been in the United States and living in the community longer were associated with ADL or IADL impairment [56].
Health conditions
In terms of health conditions, disease, especially chronic conditions, is a major risk factor associated with physical function impairment. Relatedly, polypharmacy is another risk factor associated with physical function impairment [86]. Most commonly reported diseases include obesity [55,58,87], sarcopenia [77,88,89], stroke [14,55,62,63,69], diabetes [14,62,63,69,90], arthritis [60], asthma [69], heart disease [14], hypertension [14], tracheitis [60], and emphysema (Table 3) [62,63]. Regarding obesity as an example, several studies have reported that older adults with obesity not only had generally worse physical function but also had a greater risk of ADL or IADL disability [55,58,87]. High values of BMI or waist circumference are also used to predict poor physical function performance [57,91]. Dynapenia or dynapenic-obesity were also positively associated with an increased risk of slow gait speed, mobility disability, or ADL or IADL limitations [58,87]. Moreover, worsened health over the lastyear was correlated with older Chinese Americans’ ADL or IADL impairment [56]. However, only one cross-city study conducted in Shanghai and Singapore reported that the number of chronic diseases was associated with ADL measured functional disability [64].
Changes in the psychological and psychiatric status also play a pivotal role in describing the occurrence of physical function impairment. Common risk factors include helplessness or depressive symptoms [85,92], a history of neurological disease [74], psychiatric or mood disease [74], Parkinson’s disease [62,63,69], dementia [62,63,69], and cognitive impairment [14,64,93,94]. For example, individuals who experience helplessness or depressive disorders were reported to have ADL limitations, IADL limitations, or other physical disability [85,92]. On the other hand, psychological resilience was regarded as an important protective factor that can fight against ADL disability [67].
Additionally, other risk factors related to health conditions include frailty [95], high waist circumference [57], pain [96], and poor sleep quality [97]. Last, results generated from a sample with 875 older adults born at the Peking Union Medical College Hospital of China form 1921 to 1941 showed that older maternal age at birth (35 or above) could make children at a higher risk of ADL limitation in older age [59].
Health behaviors
Existing studies conducted among Chinese communities showed a better physical function if engaged in more physical activities such as Tai Chi [98,99], habitual walking [75], or being non-smokers or quitting smoking (Table 3) [71]. For example, a study contains 39 older adults in Beijing reported that those who practiced Tai Chi has higher knee extensor strength compared to those who do not (p<0.013). Another study in Singapore indicated that older adults with self-reported higher levels of habitual walking are more likely to have better performance in peak oxygen consumption (VO2 max), one measure to examine one’s physical performance and fitness (p=0.007) [75].
Other factors
In addition to those common risk and protective factors list above, there are other factors associated with physical function impairment, such as falls [81,100,101], home environmental hazards [101], ethnicity [73], Chinese health beliefs [102], healthcare unit size [74], quality of life [56], and agricultural occupation (Table 3) [78].
According to our review, falls and home environmental hazards are common risk factors of physical function impairment among the aging population [81,100,101]. A study conducted among 1,419 community-dwelling Chinese older adults in Hong Kong revealed that an incident fall could lead to lower scores of the Barthel Index, the Total Mobility Score in Tinetti Balance and Gait Evaluation, IADL, and slower gait speed (p<0.001) [100]. Home environmental hazards can also put older adults at a high risk of falls or other physical injuries and therefore have a negative impact on their physical function. For lder adults, two common home hazards were lack of grab bars and no protections against slipping in the bathroom [101].
Auyeung et al. have reported community-dwelling Chinese older adults in Hong Kong have lower mean appendicular skeletal mass scores compared to black and white counterparts, suggesting ethnicity may be an important indicator and contributor to physical function differences [73]. Out of all the papers included in this review, there is only one study conducted in 2,272 Canadian Chinese population which quantified and analyzed Chinese culture, finding Chinese health beliefs are associated with physical health and IADL limitations [102].
Consequences
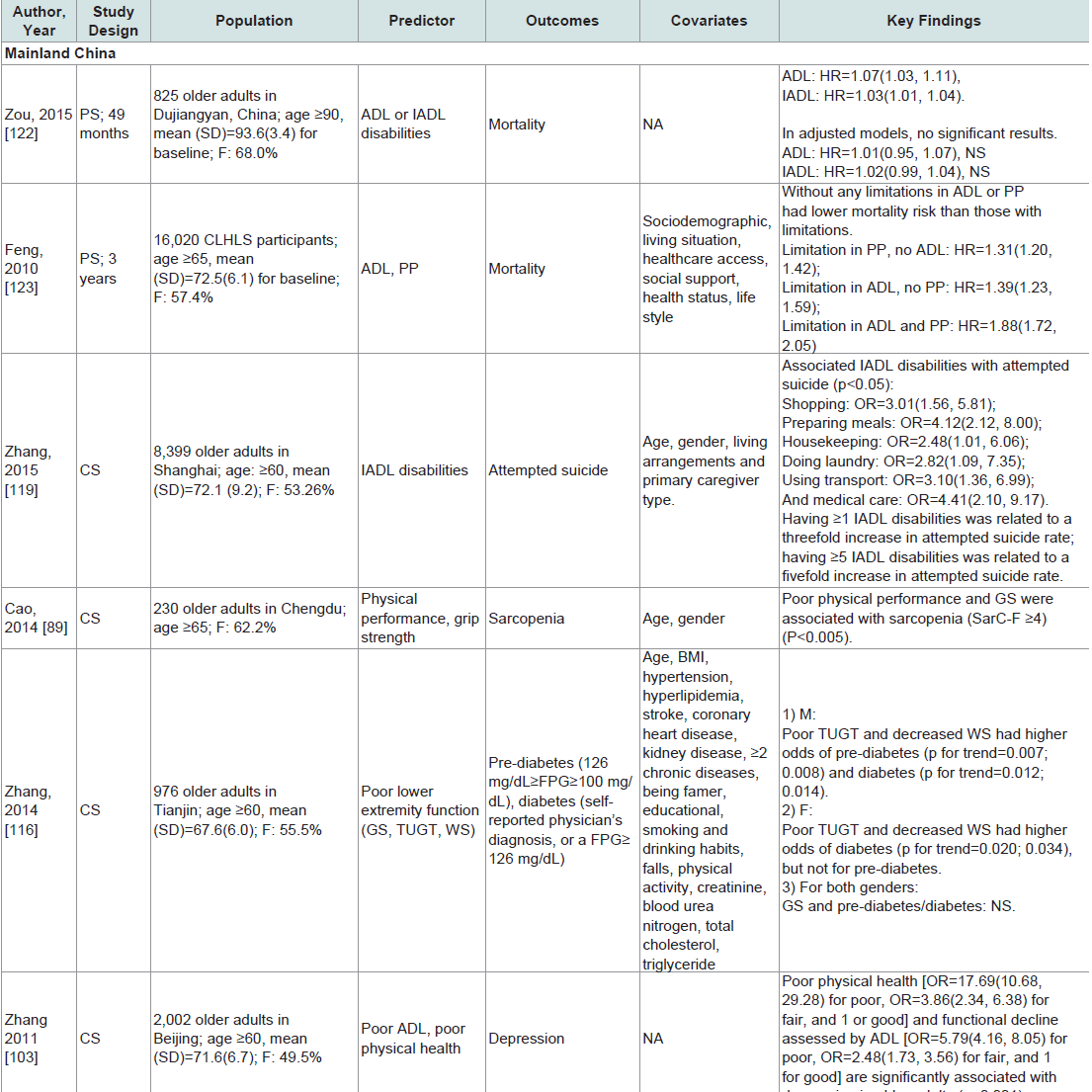
Physical function impairment has multiple serious consequences among Chinese older adults, such as depression or depressive symptoms [11,103-109], cognitive impairment [110-112], fear of falling [113], falls [114,115], sarcopenia [89], pre-diabetes and diabetes [116], low anthropometric indices [117], a risking risk of dependency [118], and institutionalization [118], attempted suicide or suicidal ideation [119-121], and mortality (Table 4) [14,118,122-124]. In Mainland China, studies showed that physical function impairment was associated with depression or higher depressive symptoms, while better physical function was positively associated with psychological well-being [11,103-109]. In addition, a history of falls is one of the most recognizable risk factors of physical function impairment, and physical function impairment in turn can result in falls [114,115]. Poor ADL performance can also make older adults fear falling, which has been shown among Chinese older adults [113]. Furthermore, reduced walking speed and stride length ay be a predictor of older adults’ rising risk of dependency and institutionalization [118]. Suicide or suicidal ideation is another consequence associated with physical function impairment [119-121]. For example, a study conducted among 8,399 Chinese older adults aged 60 or above in Shanghai reported that IADL disabilities were associated with attempted suicide. The researchers also demonstrated that more IADL disabilities is related to an increase in suicide attempts [119]. Moreover, impairment in physical function can lead to severe consequences among Chinese aging population such as a higher risk of mortality [14,118,122-124].
Prevalence/Incidence: The prevalence of physical function impairment varies across different regional and cultural groups; however, there are limited studies comparing the prevalence rates between Chinese and other racial groups. Lack of a standardizedevaluation makes it difficult to compare prevalence rates across multiple study groups. According to our review, only two studies conducted in North America did the comparisons of physical function impairment among different racial groups. One reported that the Chinese subgroup has the highest ADL or IADL disability prevalence compared to other Asian Americans [29], while the other reported the Chinese subgroup has the lowest disability prevalence compared to other Asian Americans [125]. The results are contradictory and further research comparing prevalence across different racial groups is needed.
Another study conducted among U.S. Chinese older adults in the Greater Chicago Area reported a high IADL impairment prevalence of 50.2% [56], which indicates Chinese immigrants may have a higher risk of physical function impairment due to unique factors associated with immigration status, such as acculturation [49,126]. Linguistic and cultural barriers can result in poor access to and use of healthcare services [127,128] and negatively influence Asian immigrants on their physical and mental health [128,129], which may lead to a high prevalence of physical function impairment. Although most studies reported increasing numbers of physical function impairment over time, this trend is not uniformly present in all research. There are three articles which reported a decline of ADL or IADL disability among Chinese aging population [53,70,130]. For example, a 10-year study examining the trends of ADL and IADL disability in a cohort of Shanghai reported that older adults in 2003, 2005, and 2008 were less likely to be IADL disabled compared to those in 1998, but no significant changes were found in ADL [130]. More longitudinal studies are needed to explore the trends of physical function impairment among Chinese older adults over time.
Risk and protective factors: Due to the diversity of studies with respect to setting, population, and research methodologies, a variety of risk factors have been identified to be associated with physical function impairment among Chinese older adults. According to our review, the most common risk factors of physical function impairment in Chinese aging populations include older age, female gender, lower education levels, lower socioeconomic status, unmarried, having fewer household members, rural residents, chronic diseases, depression or depressive symptoms, cognitive impairment, and incident falls, which resonated with prior studies conducted in other geographic areas with non-Chinese individuals [19,86,131-136]. However, one longitudinal study reported an increasing disability trend over time experienced by male rather than female [70]. The association between female gender and physical function impairment deserves further exploration. Research has also established among other racial and ethnic groups that smoking, alcohol abuse, an unhealthy diet associated obesity, and lack of exercise could cause worsening in physical performance [81,133,134,137,138]; similarly, our review revealed that healthy lifestyle behaviors may lead to better physical functioning among Chinese older adults, such as engaged in more physical activities, practicing Tai Chi, habitual walking, and being non-smokers or quitting smoking. Notably, there is still limited knowledge regarding other factors like ethnic or racial differences. For example, although one prior study reported that Asian older adults may experience poorer physical function than other ethnic groups [73], but still, very little is known about the ethnic difference in physical function impairment between Chinese and other aging populations.
Consequences: Depression or depressive symptoms, cognitive impairment, fear of falling, falls, sarcopenia, attempted suicide or suicidal ideation, and mortality are established health consequences associated with physical function impairment for Chinese older adults. These findings were consistent with research conducted among other racial groups [9,13,39-48]. Notably, depression or depressive symptoms, falls, sarcopenia, and cognitive impairment were reported not only as risk factors but also as outcomes of physical function impairment. For example, falls may directly lead to physical function impairment, and also may confine older adults to homes and limit their activity due to fear of falls, which may further accelerate functional loss and put older adults at a higher risk of recurrent falls.
The relationship between these factors and physical impairment warrants further investigation among the Chinese aging population. Additionally, there are limited studies examining other health consequences associated with physical function impairment among Chinese aging population, which has been reported in other cohorts, such as self-neglect [139], and pre-diabetes or diabetes [116].
Previous studies have highlighted the impact of physical function impairment on the occurrence of mental health issues such as depression or depressive symptoms, and suicidal ideation among older adults [12,92,119-121]. Older adults with physical function impairment are experiencing difficulties in performing daily tasks or mobility, which indicates they may become more dependent and treat themselves as a burden to others. In particular, deeply influenced by Confucian culture, Chinese older adults may have high expectation of filial piety of the younger generation and rely on their children or other family members [50]. Thus, emotional support and caregiving from children or family members tend to be important for Chinese older adults, especially for those with physical function impairment. Unfortunately, the actual behaviors of children do not always fit the expectation of parents due to having difficulty of work-life balance, and disparities of culture values between East and West [50]. That could be one explanation why psychological issues are commonly reported among Chinese older adults [140-144], and why physical function impairment among Chinese older adults is linked to depressive symptoms or suicidal ideation.
Overall, there are several limitations in the current research field of physical function concerning Chinese older adults. First, there is a lack of a standardized evaluation to measure one’s physical function. Older adults’ physical function is usually measured by self-reported evaluation or observed performance-based tests. For physical and mobility disability assessments, Activities of Daily Living (ADL), Instrumental Activities of Daily Living Scale (IADL), the Barthel Index, and the Health Assessment Questionnaire (HAQ) Disability Scale are most commonly used. For functional assessment tools, Tinetti Performance Oriented Mobility Assessment Tool, Walking Speed, Functional Independence Measure, and Timed Up and Go (TUG) test are considered [145-147]. A variety of instruments are used in different studies in order to meet different research needs. However, this also decreases the ability to compare across studies. Even for studies that use same measurement, cutoff points that define impairment may differ, leading to vast variations in estimating the prevalence of physical function impairment. Researchers should expand efforts to develop a more-consistent instrument and standardized cutoff points for future assessment of physical function impairment to facilitate comparisons across studies. Another limitation is the discordance between self-reported and performance based tests in previous research [56]. For self-report tests, Chinese older adults may be reluctant to report true situation about their physical function status due to the traditional Chinese value of “saving face”. As a result, the accuracy and credibility of results could be reduced. Additionally, the sample sizes of most existing studies among Chinese older adults are relatively small. A large and representative sample size is encouraged to provide more convincing evidence for future strategy planning and policy making in health promotion. In terms of the limitations of this review, we did not include peer-reviewed manuscripts in non-English languages Nevertheless, this systematic review characterizes the state-of-science in physical function, reveals physical function impairment is an important issue among global Chinese aging population, as well as illustrates the future research direction and practical strategies.
Similarly, there are several consequences of physical function impairment that has been widely reported in other race groups, but are not yet fully examined among Chinese older adults, especially in overseas Chinese aging population, such as increased risk of mortality [13,48], attempted suicide or suicidal ideation [150,151], and depression or depressive symptoms [152,153]. As one of the most severe outcomes of physical function change, more attention should be paid to the relationship between mortality and physical function impairment. Additionally, attempted suicide or suicidal ideation may further result in higher risk of mortality, suggesting the importance of offering psychological counseling service to prevent suicide or suicidal ideation for those vulnerable groups. More studies are still needed to evaluate the associations between depression and depressive symptoms or other mental disorders and older adults’ physical function impairment, as well as examine how mental health care can prevent Chinese older adults with physical function impairment from developing severe psychological illnesses.
Moreover, for overseas Chinese older adults, there is limited information generated from communities or institutes in Singapore, Canada, and the United States. Since an increasing number of Chinese immigrants are living in different foreign countries, and overseas population might have different experience in physical function impairment than Chinese population in China due to diversity of socioeconomics, acculturation levels, citizenship and immigration status, culture beliefs, language, and access to healthcare services [154-156], a lack of representative studies in other regions may impede to develop a comprehensive understanding on this aging issue. More studies conducted in overseas Chinese communities, as well as more comparative data across different regions and cultural groups are needed.
To advance our understanding of trends in physical function change in Chinese aging population over time, longitudinal studies are needed among the aging population living in the Mainland China as well as overseas Chinese communities. Despite quantitative analysis, qualitative studies can help to generate an in-depth understanding of the concerns, needs, and barriers of older adults with physical function impairment as well as the cultural context behind this aging issue. It is also important to better provide social and healthcare services for older adults and to develop effective intervention programs.
Cultural components among Chinese aging population: First, existing studies did not fully consider the potential influence caused by filial piety or caregiving and how it relates to poor physical performance in Chinese population. Considering the culture components could be critical for better research and intervention design to address potential biases when understanding physical function in a Chinese population. Second, one study conducted in Chicago reported that a decline in physical function was related to higher risk of elder abuse [20], while other studies indicated thatthere was no significant association between physical dependence and a greater risk of elder abuse [157,158]. Given that elder abuse is a serious and common public health concern among Chinese older adults [158], older adults may face burden of grand-parenting [159], and there is a lack of evidence-based research conducted in diversity Chinese communities, it is important to explore the complexity of the relationship between physical function impairment and elder abuse. Third, the ethnic difference of physical function impairment between Chinese older adults and other racial groups has been shown in someprevious studies [29,56,125]. More studies are still needed to explore these across racial groups by considering disparities in life styles, eating habits, geographic settings, socio-economic characteristics, and cultural values. Further, there is diversity within Chinese aging population, which has yet to be explored.
Furthermore, safe living environments for older adults are important for Chinese older adults with physical impairments. As people age, falls are more frequent and serious due to poor balance function, weak muscle strength, and thinning of bones [136]. The home environmental hazards should be removed to prevent incidence falls or injuries. Legislation can be an effective safeguard of rights of older adults with physical function impairment. In 1990, the U.S. Congress enacted the Americans with Disabilities Act (ADA)to prevent disabilities from discrimination, to defend their rights, and to take care of them regarding employment, public entities and transportation, public accommodations and commercial facilities, and telecommunications. China also promulgated the Law of the People’s Republic of China on the Protection of Disabled Persons in 1990 to protect disabilities on aspects ranging from rehabilitation, education, employment, cultural life, welfare, environment, to legal liabilities [162]. While these legislations have promoted health equity for older adults, special attention should be paid to the accessibility of these resources for individuals who have limited English proficiency and may experience other cultural or structural barriers in accessing services. Although this multifaceted approach across individual,familial, and structural level may be difficult, joint efforts and close collaborations of the whole society are necessary to facilitate better health and quality of life among older adults, their families, as well as the general population.
Epidemiology of Physical Function Impairment in Global Chinese Aging Population: A Systematic Review
XinQi Dong* and Dan Su
- Rush Institute for Healthy Aging, Rush University Medical Center, Chicago, Illinois, USA
*Address for Correspondence: XinQi Dong, Professor of Medicine, Nursing and Behavioral Sciences Director, Chinese Health, Aging and Policy Program Associate Director, Rush Institute for Healthy Aging, Rush University Medical Center, Chicago, Illinois, USA, Tel: 312 942 3350; Fax: 312 942 2861; E-mail: xinqi_dong@rush.edu
Citation: Dong X, Su D. Epidemiology of Physical Function Impairment in Global Chinese Aging Population: A Systematic Review. J Geriatrics Palliative Care 2016;4(1): 23.
Copyright © 2016 Dong X, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Geriatrics and Palliative Care | ISSN: 2373-1133 | Volume: 4, Issue: 1
Submission: 22 February 2016 | Accepted: 26 April, 2016 | Published: 3 May 2016
Abstract
Background: Physical function is a cornerstone of geriatric medicine. Impairment in physical function may threaten one’s ability to live independently and is associated with multiple negative health outcomes. Although Chinese people is one of the fastest growing populations in the world, there is a limited understanding of the epidemiology of physical function impairment in the global Chinese aging population.
Methods: Researchers used the PRISMA statement and performed a comprehensive online search to highlight the global epidemiology of physical function impairment of Chinese older adults in terms of prevalence, incidence, risk and protective factors, and health consequences. Search items include Chinese, older adult, Asian elderly, aging, physical function, physical function impairment, disability, function impairment, functional dependence, functional limitation, mobility, ADL, IADL, Nagi, and Rosow-Breslau.
Results: Eighty-two papers met inclusion criteria. Prevalence of ADL impairment ranges from 3.0% to 11.6%, while prevalence of IADL impairment ranges from 7.9% to 50.2%. Common risk factors include older age, female gender, lower education, lower income, rural residences, unmarried status, chronic diseases, depression/depressive symptoms, cognitive impairment, and falls. Health outcomes include suicidal ideation/attempted suicide, depression/depressive symptoms, cognitive impairment, falls, and mortality.
Conclusion: The prevalence of physical function impairment among Chinese aging population varies across regions and the number of physical function impairments increases over time. Physical function is influenced by multiple aspects, including socio-demographic characteristics, health conditions, and health behaviors, and can lead to adverse health outcomes. Future longitudinal research is necessary to explore the regional differences, effectiveness of existing intervention programs, as well as the cultural contexts of physical function impairment. Concerted support from caregivers, healthcare and social service providers, and policy makers is necessary to improve physical function and promote healthy aging among Chinese older adults.
Keywords
Physical function; Older adults; ChineseIntroduction
Physical function is an important indicator of an older adult’s current health status. Subsequent impairment, often referred to as physical disability, mobility disability, or functional limitation [1], may bring growing healthcare, social, and economic burdens to society, especially as physical function may decline as people age [2]. Increased life expectancy further implies higher risk of physical function impairment [3-6]. Additionally, impairment in physical health among older adults has been linked to comorbidities [7,8], incident falls [9], pain [10], and mental disorder [11,12], which could further compromise older adults’ quality of life and even be predictive of mortality [13,14], and may also raise concerns of caregiving burden [15], living environmental hazard [16-18], social engagement [19], and social circumstances [20,21].Understanding physical function in Chinese older adults is important. According to the 6th Chinese National Population Census in 2010, the proportion of Chinese older adults aged 60 and above within the general population has increased from 8.0% to 13.3% within 20 years [22] and is projected to reach 19.3% by 2025 [23]. By 2050, it is estimated that 25% of the world’s aging population will beChinese [24]. As one of the fastest growing aging populations in the world [23], the Chinese older adult population may experience a great risk of physical function impairment, which is a serious social and public health concern. However, while many studies have been done in western countries to examine physical function among older adults, little is known in the Chinese aging population, especially among overseas Chinese population. Integrating existing information about physical function impairment among different Chinese communities can help to provide population estimates for the older adults in China and globally, as well as to direct future study and policy making.
The possible differences and similarities of physical function impairment between Chinese aging population and other racial groups warrant attention. Cultural differences may shape the understanding of disease prevention, health maintaining, and treatment [25]. In addition, genetic factors, life style, health care disparities may also partially contribute to the varied health status across different racial groups [26,27]. There is growing evidence reported that U.S. immigrants have poorer physical function compared to their US born counterparts [28]. Research has indicated worse physical health among Asian Americans compared to non-Hispanic white, and Chinese subgroup has the highest rate of prevalence of limitedphysical function compared to other Asian subgroups [29]. Chinese immigrant aging population may face a higher risk of poor health status due to cultural and linguistic barriers, social isolation, healthcare disparities, and acculturation [27]. Evidence has also suggested that relocation and loss of native support network might lead to health disparities among Chinese population [30-34]; the distress of being old combined with immigration-related barriers may make Chinese immigrant aging population even more vulnerable [35]. Furthermore, Chinese aging population may be impacted by barriers of access to health care including language, help-seeking behaviors, and traditional Chinese thinking [25,36], which may lead to delayed care and treatment, and increase the likelihood of having hysical function impairment.
Although risk/protective factors and health consequences of physical function impairment in general aging population has been identified in prior studies [9,13,19,37-48], the situation may differamong Chinese older adults due to a variety of socioeconomics, culture beliefs, health literacy, available social services, and access to healthcare resources [49]. Additionally, given the unique cultural characteristics of Chinese population, older adults may expect more care and support from family members, known as “filial piety” [50], especially for those have difficulty in daily task performance. Prior research suggested that a higher level of filial piety is associated with better self-rated health for older adults [51]. However, providingcaregiving is likely challenging for immigrant adult children due to cultural and linguistic barriers. Furthermore, Chinese older adults who suffer physical function impairment may face potential elderabuse and discrimination from others [20,52]; additionally, poor health or disability can be especially stigmatized in Chinese culture [21]. These cultural components play important roles which may mediate the relationships between physical function impairment, its risk/protective factors, and health outcomes. Moreover, looking at physical and functional impairment among Chinese aging population across countries and geographic areas can help us understand differences and similarities between populations and provide more comprehensive and better focused recommendations for health promotion. Last, understanding the epidemiology of physical function among Chinese older adults may effectively direct the allocations and uses of limited health care and social-care resources, as well as the development of future strategy at both macro and micro levels.
Despite the increasing awareness on physical function impairment among older adults, there has not been a systematic review of physical function impairment in global Chinese aging population. The purpose of this review is to improve our understanding of the epidemiology of physical function impairment among the global Chinese population including its prevalence, incidence, risk and protective factors, and health consequences, and also aims to collect evidence and extract information for directions for future research and health policy.
Materials and Methods
By using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, this review includes articles that discuss physical function problems among Chinese older adults globally. Inclusion criteria for this review paper are studies that report prevalence or incidences of physical function impairment, as well as risk factors, and health outcomes. Eligible studies focus on older adults aged 50 years old or above who self-identify as ethnic Chinese. The global literature was searched in the databases PubMed, MEDLINE, PsychInfo, China Knowledge Resource Integrated Database, and Wan Fang Data. Search keywords include: “Chinese”, “older adult”, “Asian elderly”, “aging”, “physical function”, “physical function impairment”, “disability”, “function impairment”, “functional dependence”, “functional limitation”, “mobility”, “ADL”, “IADL”, “Nagi”, and “Rosow-Breslau”. One review also identified and examined for relevant articles [38]. To refine our review, full manuscripts were further screened to eliminate ineligible articles. Exclusion criteria were: abstracts or case reports, qualitative studies, published over 25 years ago, written in non-English language, combined sample of Chinese and other race group, did not clearly define physical function as the primary dependent or independent variable, and examine the aggregate of physical function and other factors (Figure 1).Results
There are a total of 125 articles identified through the online database search, and 82 of them met inclusion criteria. These 82 articles discussed physical function problems among Chinese older adults in Mainland China (n=35), Hong Kong (n=22), Taiwan (n=16), Singapore (n=2), and North America (n=7). Three papers have cross-city samples. Among eligible articles, 23 included the information regarding prevalence of physical function impairment, 5 reported the incidence of physical function decline and trends in physical function, 47 examined the risk and protective factors associated with physical function impairment, and 25 evaluated the health consequence related to physical function impairment. Author, year, study design, population and setting, key independent variables, covariates, outcomes and key findings are presented in Tables 1-4.Prevalence
Prevalence of older adults’ physical function impairment varies across different Chinese communities depending on the setting, research methods, and measurements. Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) limitations are most commonly measurements used to assess one’s physical function. The majority of studies used “difficulty in completing at least one item of daily tasks” as the cut-off point of ADL or IADL impairment [53-55]. The rates of ADL impairment ranged from 3.0% to 11.6% among global Chinese communities [23,29,56-64], while the rates of IADL impairment ranged from 7.9% to 50.2% (Table 1) [23,29,56,57,61]. Further, the prevalence of physical function impairment was relatively higher among Chinese population compared to other ethnic or racial groups. For example, the National Health Interview Survey of 738 Asian American older adults suggested that the Chinese subgroup experienced the highest ADL or IADL disabilities (11.6% ADL vs. 17.3% IADL impairment) compared to other subgroups of Asian Americans (Filipino: 8.3% ADL vs. 15.3% IADL impairment; Asian Indian: 4.6% ADL vs. 9.1% IADL impairment) [29]. Additionally, studies also report that Chinese older adults living in Chicago had a higher prevalence of IADL impairment in comparison with other Chinese older adults in Mainland China [23,56,61]. In addition to ADL and IADL measurements, researchers have used other assessment tools to evaluate Chinese older adults’ physical function, such as Nagi index of basic physical activities and Rosow and Breslau index of mobility [56,65]. A recent paper documented that the rate of self-reported mobility disability was 8.9% in males and 8.5% in females among 616 community-dwelling older adults aged 60 or above in Chengdu and Suining [58], while another paper reported that the rate of low skeletal muscle mass was 9.55% in males compared to 6.63% in females based on a survey of 432 older adults aged 65 or above in Yanqing [66].
Incidence
Most papers reported that an increasing proportion of older adults experience physical function impairment over time (Table 2) [61,67-70]. For instance, the Chinese Longitudinal Healthy Longevity Survey, a four-year follow-up study of 11,112 older adults acrossChina, reported that the rate of ADL disability onset was 9.67% [67]. Additionally, these trends may differ by gender. A communitydwelling study conducted in Beijing reported that the ADL disability increased by 0.96% per year for males over a 15 years follow-up, while declining by 1.15% per year for females [70].
Risk and Protective Factors
Social demographic factorsIn terms of demographic factors, older age, female gender, lower socioeconomic status, and lower education levels are common risk factors of physical function impairment among Chinese older adults (Table 3) [23,29,54,56,60,61,64,65,71-84]. Previous research among Chinese older adults documented that older age was significantly associated with higher risk of physical function impairment [23,29,56,60,65,71,77,78,80-83]. Interestingly, a study of 7,845 Chinese older adults found that young-old older adults (60-69 years old) experienced higher severity of ADL impairment compared to an older subgroup (70 years old and above) [54]. Additionally, gender is another widely discussed predictor of physical function impairment; multiple studies indicated females are more likely to suffer physical disability or other ADL/IADL difficulties than males [29,54,56,65,71-75,82,84]. Further, two studies reported that older adults with lower socio-economic status or lower income have a higher proportion ofworsening functional status [61,80], while another study concluded that absolute income is not an important predictor of functionaldependency [85]. Moreover, higher self-rated financial adequacy wasreported to indicate better physical health [84]. With respect to the level of education, Chinese older adults with lower education levels were correlated with higher possibility of ADL and IADL impairment, or mobility decline [56,60,61,65,81,83]. One study further indicated that an individual with a lower education level was more likely to have early-onset functional limitation [82].
Regarding family arrangement, risk factors of physical function impairment include being unmarried or widowed, having fewer household members, and having more children [23,29,56,83]. While most studies reported that being unmarried or widowed can predict physical function impairment [23,29,56], one study found that married individuals in Beijing showed higher levels of ADL limitations compared to unmarried ones [65]. A research based on the data generated from 3,159 Chinese older adults in the Greater Chicago Area mentioned that having fewer household members and more children has been linked with ADL or IADL impairment [56].
With respect to location and immigration status, risk factors include living in a rural area, larger Chinese community, and living in the U.S. for more years [23,54,56,71,78,84]. Three studies from Mainland China indicated the difference of functional disabilities between rural and urban residents [23,54,78]. Compared with respondents living in urban areas, older adults living in rural areas had higher disability rates for all age groups [23,54]. One study found that rural residence was associated with ADL limitation among female participants [78]. In contrast, a study indicated that living in a rural area could lead to a less rapid increase in ADL difficulties [71]. Additionally, one study among 2,272 Chinese Canadian population reported that residing in communities with a smaller Chinese population was associated with better physical health [84]. In terms of immigration status, results based on a community-dwelling population of U.S. Chinese older adults indicated that having been in the United States and living in the community longer were associated with ADL or IADL impairment [56].
Health conditions
In terms of health conditions, disease, especially chronic conditions, is a major risk factor associated with physical function impairment. Relatedly, polypharmacy is another risk factor associated with physical function impairment [86]. Most commonly reported diseases include obesity [55,58,87], sarcopenia [77,88,89], stroke [14,55,62,63,69], diabetes [14,62,63,69,90], arthritis [60], asthma [69], heart disease [14], hypertension [14], tracheitis [60], and emphysema (Table 3) [62,63]. Regarding obesity as an example, several studies have reported that older adults with obesity not only had generally worse physical function but also had a greater risk of ADL or IADL disability [55,58,87]. High values of BMI or waist circumference are also used to predict poor physical function performance [57,91]. Dynapenia or dynapenic-obesity were also positively associated with an increased risk of slow gait speed, mobility disability, or ADL or IADL limitations [58,87]. Moreover, worsened health over the lastyear was correlated with older Chinese Americans’ ADL or IADL impairment [56]. However, only one cross-city study conducted in Shanghai and Singapore reported that the number of chronic diseases was associated with ADL measured functional disability [64].
Changes in the psychological and psychiatric status also play a pivotal role in describing the occurrence of physical function impairment. Common risk factors include helplessness or depressive symptoms [85,92], a history of neurological disease [74], psychiatric or mood disease [74], Parkinson’s disease [62,63,69], dementia [62,63,69], and cognitive impairment [14,64,93,94]. For example, individuals who experience helplessness or depressive disorders were reported to have ADL limitations, IADL limitations, or other physical disability [85,92]. On the other hand, psychological resilience was regarded as an important protective factor that can fight against ADL disability [67].
Additionally, other risk factors related to health conditions include frailty [95], high waist circumference [57], pain [96], and poor sleep quality [97]. Last, results generated from a sample with 875 older adults born at the Peking Union Medical College Hospital of China form 1921 to 1941 showed that older maternal age at birth (35 or above) could make children at a higher risk of ADL limitation in older age [59].
Health behaviors
Existing studies conducted among Chinese communities showed a better physical function if engaged in more physical activities such as Tai Chi [98,99], habitual walking [75], or being non-smokers or quitting smoking (Table 3) [71]. For example, a study contains 39 older adults in Beijing reported that those who practiced Tai Chi has higher knee extensor strength compared to those who do not (p<0.013). Another study in Singapore indicated that older adults with self-reported higher levels of habitual walking are more likely to have better performance in peak oxygen consumption (VO2 max), one measure to examine one’s physical performance and fitness (p=0.007) [75].
Other factors
In addition to those common risk and protective factors list above, there are other factors associated with physical function impairment, such as falls [81,100,101], home environmental hazards [101], ethnicity [73], Chinese health beliefs [102], healthcare unit size [74], quality of life [56], and agricultural occupation (Table 3) [78].
According to our review, falls and home environmental hazards are common risk factors of physical function impairment among the aging population [81,100,101]. A study conducted among 1,419 community-dwelling Chinese older adults in Hong Kong revealed that an incident fall could lead to lower scores of the Barthel Index, the Total Mobility Score in Tinetti Balance and Gait Evaluation, IADL, and slower gait speed (p<0.001) [100]. Home environmental hazards can also put older adults at a high risk of falls or other physical injuries and therefore have a negative impact on their physical function. For lder adults, two common home hazards were lack of grab bars and no protections against slipping in the bathroom [101].
Auyeung et al. have reported community-dwelling Chinese older adults in Hong Kong have lower mean appendicular skeletal mass scores compared to black and white counterparts, suggesting ethnicity may be an important indicator and contributor to physical function differences [73]. Out of all the papers included in this review, there is only one study conducted in 2,272 Canadian Chinese population which quantified and analyzed Chinese culture, finding Chinese health beliefs are associated with physical health and IADL limitations [102].
Consequences
Physical function impairment has multiple serious consequences among Chinese older adults, such as depression or depressive symptoms [11,103-109], cognitive impairment [110-112], fear of falling [113], falls [114,115], sarcopenia [89], pre-diabetes and diabetes [116], low anthropometric indices [117], a risking risk of dependency [118], and institutionalization [118], attempted suicide or suicidal ideation [119-121], and mortality (Table 4) [14,118,122-124]. In Mainland China, studies showed that physical function impairment was associated with depression or higher depressive symptoms, while better physical function was positively associated with psychological well-being [11,103-109]. In addition, a history of falls is one of the most recognizable risk factors of physical function impairment, and physical function impairment in turn can result in falls [114,115]. Poor ADL performance can also make older adults fear falling, which has been shown among Chinese older adults [113]. Furthermore, reduced walking speed and stride length ay be a predictor of older adults’ rising risk of dependency and institutionalization [118]. Suicide or suicidal ideation is another consequence associated with physical function impairment [119-121]. For example, a study conducted among 8,399 Chinese older adults aged 60 or above in Shanghai reported that IADL disabilities were associated with attempted suicide. The researchers also demonstrated that more IADL disabilities is related to an increase in suicide attempts [119]. Moreover, impairment in physical function can lead to severe consequences among Chinese aging population such as a higher risk of mortality [14,118,122-124].
Discussion
Physical function impairment is prevalent among the global Chinese population. Additionally, most studies reported an increasing number of physical function impairment over time among Chinese older adults. Common risk and protective factors of physical function impairment can be described into three main dimensions including socio-demographic characteristics, health conditions, and health behaviors. Impairments in physical function can lead to adverse health consequences, both physical and psychological. These findings indicate potential healthcare and caregiving issues for Chinese older adults with physical function impairment and have important implications for future research and policy.Prevalence/Incidence: The prevalence of physical function impairment varies across different regional and cultural groups; however, there are limited studies comparing the prevalence rates between Chinese and other racial groups. Lack of a standardizedevaluation makes it difficult to compare prevalence rates across multiple study groups. According to our review, only two studies conducted in North America did the comparisons of physical function impairment among different racial groups. One reported that the Chinese subgroup has the highest ADL or IADL disability prevalence compared to other Asian Americans [29], while the other reported the Chinese subgroup has the lowest disability prevalence compared to other Asian Americans [125]. The results are contradictory and further research comparing prevalence across different racial groups is needed.
Another study conducted among U.S. Chinese older adults in the Greater Chicago Area reported a high IADL impairment prevalence of 50.2% [56], which indicates Chinese immigrants may have a higher risk of physical function impairment due to unique factors associated with immigration status, such as acculturation [49,126]. Linguistic and cultural barriers can result in poor access to and use of healthcare services [127,128] and negatively influence Asian immigrants on their physical and mental health [128,129], which may lead to a high prevalence of physical function impairment. Although most studies reported increasing numbers of physical function impairment over time, this trend is not uniformly present in all research. There are three articles which reported a decline of ADL or IADL disability among Chinese aging population [53,70,130]. For example, a 10-year study examining the trends of ADL and IADL disability in a cohort of Shanghai reported that older adults in 2003, 2005, and 2008 were less likely to be IADL disabled compared to those in 1998, but no significant changes were found in ADL [130]. More longitudinal studies are needed to explore the trends of physical function impairment among Chinese older adults over time.
Risk and protective factors: Due to the diversity of studies with respect to setting, population, and research methodologies, a variety of risk factors have been identified to be associated with physical function impairment among Chinese older adults. According to our review, the most common risk factors of physical function impairment in Chinese aging populations include older age, female gender, lower education levels, lower socioeconomic status, unmarried, having fewer household members, rural residents, chronic diseases, depression or depressive symptoms, cognitive impairment, and incident falls, which resonated with prior studies conducted in other geographic areas with non-Chinese individuals [19,86,131-136]. However, one longitudinal study reported an increasing disability trend over time experienced by male rather than female [70]. The association between female gender and physical function impairment deserves further exploration. Research has also established among other racial and ethnic groups that smoking, alcohol abuse, an unhealthy diet associated obesity, and lack of exercise could cause worsening in physical performance [81,133,134,137,138]; similarly, our review revealed that healthy lifestyle behaviors may lead to better physical functioning among Chinese older adults, such as engaged in more physical activities, practicing Tai Chi, habitual walking, and being non-smokers or quitting smoking. Notably, there is still limited knowledge regarding other factors like ethnic or racial differences. For example, although one prior study reported that Asian older adults may experience poorer physical function than other ethnic groups [73], but still, very little is known about the ethnic difference in physical function impairment between Chinese and other aging populations.
Consequences: Depression or depressive symptoms, cognitive impairment, fear of falling, falls, sarcopenia, attempted suicide or suicidal ideation, and mortality are established health consequences associated with physical function impairment for Chinese older adults. These findings were consistent with research conducted among other racial groups [9,13,39-48]. Notably, depression or depressive symptoms, falls, sarcopenia, and cognitive impairment were reported not only as risk factors but also as outcomes of physical function impairment. For example, falls may directly lead to physical function impairment, and also may confine older adults to homes and limit their activity due to fear of falls, which may further accelerate functional loss and put older adults at a higher risk of recurrent falls.
The relationship between these factors and physical impairment warrants further investigation among the Chinese aging population. Additionally, there are limited studies examining other health consequences associated with physical function impairment among Chinese aging population, which has been reported in other cohorts, such as self-neglect [139], and pre-diabetes or diabetes [116].
Previous studies have highlighted the impact of physical function impairment on the occurrence of mental health issues such as depression or depressive symptoms, and suicidal ideation among older adults [12,92,119-121]. Older adults with physical function impairment are experiencing difficulties in performing daily tasks or mobility, which indicates they may become more dependent and treat themselves as a burden to others. In particular, deeply influenced by Confucian culture, Chinese older adults may have high expectation of filial piety of the younger generation and rely on their children or other family members [50]. Thus, emotional support and caregiving from children or family members tend to be important for Chinese older adults, especially for those with physical function impairment. Unfortunately, the actual behaviors of children do not always fit the expectation of parents due to having difficulty of work-life balance, and disparities of culture values between East and West [50]. That could be one explanation why psychological issues are commonly reported among Chinese older adults [140-144], and why physical function impairment among Chinese older adults is linked to depressive symptoms or suicidal ideation.
Overall, there are several limitations in the current research field of physical function concerning Chinese older adults. First, there is a lack of a standardized evaluation to measure one’s physical function. Older adults’ physical function is usually measured by self-reported evaluation or observed performance-based tests. For physical and mobility disability assessments, Activities of Daily Living (ADL), Instrumental Activities of Daily Living Scale (IADL), the Barthel Index, and the Health Assessment Questionnaire (HAQ) Disability Scale are most commonly used. For functional assessment tools, Tinetti Performance Oriented Mobility Assessment Tool, Walking Speed, Functional Independence Measure, and Timed Up and Go (TUG) test are considered [145-147]. A variety of instruments are used in different studies in order to meet different research needs. However, this also decreases the ability to compare across studies. Even for studies that use same measurement, cutoff points that define impairment may differ, leading to vast variations in estimating the prevalence of physical function impairment. Researchers should expand efforts to develop a more-consistent instrument and standardized cutoff points for future assessment of physical function impairment to facilitate comparisons across studies. Another limitation is the discordance between self-reported and performance based tests in previous research [56]. For self-report tests, Chinese older adults may be reluctant to report true situation about their physical function status due to the traditional Chinese value of “saving face”. As a result, the accuracy and credibility of results could be reduced. Additionally, the sample sizes of most existing studies among Chinese older adults are relatively small. A large and representative sample size is encouraged to provide more convincing evidence for future strategy planning and policy making in health promotion. In terms of the limitations of this review, we did not include peer-reviewed manuscripts in non-English languages Nevertheless, this systematic review characterizes the state-of-science in physical function, reveals physical function impairment is an important issue among global Chinese aging population, as well as illustrates the future research direction and practical strategies.
Future Research Directions
Knowledge gap: While it has been shown that many medical conditions are associated with increased risk of physical function impairment among Chinese older adults [148], there are a few particular areas which have yet to be adequately explored. First, there is a lack of research that addresses the association between comorbidity and physical function impairment among Chinese aging group, which has been shown in a Canadian community and an American community [7,8]. Additionally, visual impairments but not hearing impairments were reported to be a risk factor of future ADL disability [149], but little is known about these associations among Chinese aging population. Larger healthcare facilities may have more health and human recourses that can provide older adults satisfactory care and support, decreasing the risk of experiencing physical limitations, but there are many unknown confounding factors between healthcare unit size and older adults’ physical status, and more studies are still needed to further demonstrate this association. Furthermore, research has focused on the risk factors of physical function impairment, while inadequately addressing its protective factors.Similarly, there are several consequences of physical function impairment that has been widely reported in other race groups, but are not yet fully examined among Chinese older adults, especially in overseas Chinese aging population, such as increased risk of mortality [13,48], attempted suicide or suicidal ideation [150,151], and depression or depressive symptoms [152,153]. As one of the most severe outcomes of physical function change, more attention should be paid to the relationship between mortality and physical function impairment. Additionally, attempted suicide or suicidal ideation may further result in higher risk of mortality, suggesting the importance of offering psychological counseling service to prevent suicide or suicidal ideation for those vulnerable groups. More studies are still needed to evaluate the associations between depression and depressive symptoms or other mental disorders and older adults’ physical function impairment, as well as examine how mental health care can prevent Chinese older adults with physical function impairment from developing severe psychological illnesses.
Moreover, for overseas Chinese older adults, there is limited information generated from communities or institutes in Singapore, Canada, and the United States. Since an increasing number of Chinese immigrants are living in different foreign countries, and overseas population might have different experience in physical function impairment than Chinese population in China due to diversity of socioeconomics, acculturation levels, citizenship and immigration status, culture beliefs, language, and access to healthcare services [154-156], a lack of representative studies in other regions may impede to develop a comprehensive understanding on this aging issue. More studies conducted in overseas Chinese communities, as well as more comparative data across different regions and cultural groups are needed.
To advance our understanding of trends in physical function change in Chinese aging population over time, longitudinal studies are needed among the aging population living in the Mainland China as well as overseas Chinese communities. Despite quantitative analysis, qualitative studies can help to generate an in-depth understanding of the concerns, needs, and barriers of older adults with physical function impairment as well as the cultural context behind this aging issue. It is also important to better provide social and healthcare services for older adults and to develop effective intervention programs.
Cultural components among Chinese aging population: First, existing studies did not fully consider the potential influence caused by filial piety or caregiving and how it relates to poor physical performance in Chinese population. Considering the culture components could be critical for better research and intervention design to address potential biases when understanding physical function in a Chinese population. Second, one study conducted in Chicago reported that a decline in physical function was related to higher risk of elder abuse [20], while other studies indicated thatthere was no significant association between physical dependence and a greater risk of elder abuse [157,158]. Given that elder abuse is a serious and common public health concern among Chinese older adults [158], older adults may face burden of grand-parenting [159], and there is a lack of evidence-based research conducted in diversity Chinese communities, it is important to explore the complexity of the relationship between physical function impairment and elder abuse. Third, the ethnic difference of physical function impairment between Chinese older adults and other racial groups has been shown in someprevious studies [29,56,125]. More studies are still needed to explore these across racial groups by considering disparities in life styles, eating habits, geographic settings, socio-economic characteristics, and cultural values. Further, there is diversity within Chinese aging population, which has yet to be explored.
Implications for Practical Strategies
There are implications for practical strategies from individual, familial, and policy levels. First, “self-improvement” is important to promote healthy aging and prevent physical function impairment among Chinese older adults [160]. Given the evidence regarding possible intervention strategies, moderate physical activities and partnerships with trained medical professionals may be helpful to maintain physical health for Chinese older adults. Our review findings also suggest that mental health were related to older adults’ physical function status. Intervention strategies which emphasize physical, psychological and social wellbeing, either through clinical trials or social services, should consider linguistically and culturally appropriate measures to better serve diverse aging population. Given the diversity of physical function in older adults’ socio-demographic characteristics, risk and protective factors, and health status, the intervention programs design and health policy making should especially focus on these high-risk groups. Cost effectiveness and applicability of new developed intervention programs should also be considered. Additionally, policy makers should invest in more resources for all individuals, families, and systems involved in caring for Chinese older adults based on the concerning prevalence rates of physical impairment globally. Caring for impaired older adults may be a traditional Chinese value; however, especially for overseas Chinese communities, Chinese adult children may experience a disproportionate burden due to lack of linguistically and culturally appropriate support. Future efforts should expand to promote the collaboration between research institutions and community organizations to better address these concerns and needs [161].Furthermore, safe living environments for older adults are important for Chinese older adults with physical impairments. As people age, falls are more frequent and serious due to poor balance function, weak muscle strength, and thinning of bones [136]. The home environmental hazards should be removed to prevent incidence falls or injuries. Legislation can be an effective safeguard of rights of older adults with physical function impairment. In 1990, the U.S. Congress enacted the Americans with Disabilities Act (ADA)to prevent disabilities from discrimination, to defend their rights, and to take care of them regarding employment, public entities and transportation, public accommodations and commercial facilities, and telecommunications. China also promulgated the Law of the People’s Republic of China on the Protection of Disabled Persons in 1990 to protect disabilities on aspects ranging from rehabilitation, education, employment, cultural life, welfare, environment, to legal liabilities [162]. While these legislations have promoted health equity for older adults, special attention should be paid to the accessibility of these resources for individuals who have limited English proficiency and may experience other cultural or structural barriers in accessing services. Although this multifaceted approach across individual,familial, and structural level may be difficult, joint efforts and close collaborations of the whole society are necessary to facilitate better health and quality of life among older adults, their families, as well as the general population.
Conclusion
Developing of physical function impairment is a natural process as people age. This review highlights physical function impairment; its risk and protective factors, and associated health consequences to advance the understanding of this complicated aging issue among the global Chinese population. Global longitudinal studies are critical to examine the regional and ethnic differences, effectiveness of existing intervention programs, and how physical function impairment relates to culture components such as filial piety and elder abuse. In addition, the relatively high prevalence and a growing number of physical function impairment over time in Chinese aging population reveal the importance of enhancing older adults’ physical fitness and call for more physical function screenings, long-term healthcare and service services, health policy support, and multifactor intervention programs for Chinese older adults. Also, the effectiveness, feasibility, and sustainability of existing interventions should be evaluated.References
- Guralnik JM, Fried LP, Salive ME (1996) Disability as a public health outcome in the aging population. Annu Rev Public Health 17: 25-46.
- Diehr PH, Thielke SM, Newman AB, Hirsch C, Tracy R (2013) Decline in health for older adults: five-year change in 13 key measures of standardized health. J Gerontol A Biol Sci Med Sci 68: 1059-1067.
- Grunenberg EM (1977) The failure of success. Milbank Mem Fund Q Health Soc 55: 3-24.
- Fries JF (1980) Aging, natural death, and the compression of morbidity. N Engl J Med 303: 130-135.
- Manton KG (1982) Changing concepts of morbidity and mortality in the elderly population. Milbank Mem Fund Q Health Soc 60: 183-244.
- Robine JM, Michel JP (2004) Looking forward to a general theory on population aging. J Gerontol A Biol Sci Med Sci 59: M590-M597.
- Schmitz N, Wang J, Malla A, Lesage A (2007) Joint effect of depression and chronic conditions on disability: results from a population-based study. Psychosom Med 69: 332-338.
- Whitson HE, Cousins SW, Burchett BM, Hybels CF, Pieper CF, et al. (2007) The combined effect of visual impairment and cognitive impairment on disability in older people. J Am Geriatr Soc 55: 885-891.
- (2001) Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc 49: 664-672.
- Weiner DK, Haggerty CL, Kritchevsky SB, Harris T, Simonsick EM, et al. (2003) How does low back pain impact physical function in independent, well‐functioning older adults? Evidence from the Health ABC Cohort and implications for the future. Pain Med 4: 311-320.
- Yunming L, Changsheng C, Haibo T, Wenjun C, Shanhong F, et al. (2012) Prevalence and risk factors for depression in older people in Xi′an China: a community‐based study. Int J Geriatr Psychiatry 27: 31-39.
- Lee SH, Tsai YF, Chen CY, Huang LB (2014) Triggers of suicide ideation and protective factors of actually executing suicide among first onset cases in older psychiatric outpatients: a qualitative study. BMC Psychiatry 14: 269.
- Wallman T, Wedel H, Johansson S, Rosengren A, Eriksson H, et al. (2006) The prognosis for individuals on disability retirement an 18-year mortality follow-up study of 6887 men and women sampled from the general population. BMC Public Health 6: 103.
- Lee JS, Auyeung TW, Leung J, Kwok T, Leung PC, et al. (2011) Physical frailty in older adults is associated with metabolic and atherosclerotic risk factors and cognitive impairment independent of muscle mass. J Nutr Health Aging 15: 857-862.
- Brown LJ, Potter JF, Foster BG (1990) Caregiver burden should be evaluated during geriatric assessment. J Am Geriatr Soc 38: 455-460.
- Verbrugge LM, Jette AM (1994) The disablement process. Soc Sci Med 38: 1-14.
- Gill TM, Robison JT, Williams CS, Tinetti ME (1999) Mismatches between the home environment and physical capabilities among community‐living older persons. J Am Geriatr Soc 47: 88-92.
- Gill TM, Williams CS, Robison JT, Tinetti ME (1999) A population-based study of environmental hazards in the homes of older persons. Am J Public Health 89: 553-556.
- Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, et al. (1999) Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med 48: 445-469.
- Dong X, Simon M, Evans D (2012) Decline in physical function and risk of elder abuse reported to social services in a community‐dwelling population of older adults. J Am Geriatr Soc 60: 1922-1928.
- Dong X, Chen R, Simon MA (2014) Experience of discrimination among US Chinese older adults. J Gerontol A Biol Sci Med Sci 69 Suppl 2: S76-S81.
- National Bureau of Statistics of the People's Republic of China (2010) National Census Bulletin.
- Tang Z, Wang HX, Meng C, Wu XG, Ericsson K, et al. (1999) The prevalence of functional disability in activities of daily living and instrumental activities of daily living among elderly Beijing Chinese. Arch Gerontol Geriatr 29: 115-125.
- Banister J (1992) Implications of the aging of China’s population. In: The population of modern China. Springer, pp. 463-490.
- Gervais MC, Jovchelovitch S (1998) The health beliefs of the Chinese community in England: a qualitative research study. Health Education Authority, London, England.
- Williams DR, Lavizzo-Mourey R, Warren RC (1994) The concept of race and health status in America. Public Health Rep 109: 26-41.
- Dong X, Chang ES, Wong E, Wong B, Skarupski KA, et al. (2010) Assessing the health needs of Chinese older adults: Findings from a community-based participatory research study in Chicago's Chinatown. J Aging Res 2010: 1-12.
- Zhang Z, Hayward MD, Lu C (2012) Is there a Hispanic epidemiologic paradox in later life? A closer look at chronic morbidity. Res Aging 34: 548-571.
- Coustasse A, Bae S, Arvidson CJ, Singh KP (2008) Disparities in self-reported activities of daily living and instrumental activities of daily living disability among Asian American subgroups in the United States: results from the National Health Interview Survey 2001-2003. Disabil Health J 1: 150-156.
- Hwang, WC, Wood JJ (2009) Acculturative family distancing: links with self-reported symptomatology among Asian Americans and Latinos. Child Psychiatry Human Dev 40: 123-138.
- Yu ES, Kim KK, Chen EH, Brintnall RA, Liu WT, et al. (2001) Colorectal cancer screening among Chinese Americans: a community-based study of knowledge and practice. J Psychosoc Oncol 19: 97-112.
- Yu ES, Kim KK, Chen EH, Brintnall RA (2001) Breast and cervical cancer screening among Chinese American women. Cancer Prac 9: 81-91.
- Parikh NS, Fahs MC, Shelley D, Yerneni R (2009) Health behaviors of older Chinese adults living in New York City. J Community Health 34: 6-15.
- McCracken M, Olsen M, Chen MS Jr, Jemal A, Thun M, et al. (2007) Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin 57: 190-205.
- Zhan HJ, King SV, Kim JH, Zhang G, Whittington FJ (2004) Double-bind: the experience of aging and being an ethnic minority in the US among Chinese and Korean American elders. Hallym Int J Aging 6: 119-139.
- Collins KS, Tenney K, Hughes DL (2002) Quality of health care for African Americans: findings from the Commonwealth Fund 2001 health care quality survey. Commonwealth Fund.
- Ayis S, Gooberman-Hill R, Bowling A, Ebrahim S (2006) Predicting catastrophic decline in mobility among older people. Age Ageing 35: 382-387.
- Hairi NN, Hiong TG, Bulgiba A, Mudla I (2012) Physical function in older people. INTECH Open Access Publisher.
- Penninx BW, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJ, et al. (1998) Depressive symptoms and physical decline in community-dwelling older persons. JAMA 279: 1720-1726.
- Cole MG, Dendukuri N (2003) Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry 160: 1147-1156.
- Callahan CM, Hendrie HC, Nienaber NA, Tierney WM (1996) Suicidal ideation among older primary care patients. J Am Geriatr Soc 44: 1205-1209.
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, et al. (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49: M85-M94.
- Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, et al. (1998) Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA 279: 585-592.
- Giampaoli S, Ferrucci L, Cecchi F, Lo Noce C, Poce A, et al. (1999) Hand-grip strength predicts incident disability in non-disabled older men. Age Ageing 28: 283-288.
- Rantanen T, Guralnik JM, Ferrucci L, Penninx BW, Leveille S, et al. (2001) Coimpairments as predictors of severe walking disability in older women. J Am Geriatr Soc 49: 21-27.
- 46. Camicioli R, Howieson D, Oken B, Sexton G, Kaye J (1998) Motor slowing precedes cognitive impairment in the oldest old. Neurology 50: 1496-1498.
- Cumming RG, Salkeld G, Thomas M, Szonyi G (2000) Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci 55: M299-M305.
- Olsen J, Jeune B (1979) The mortality experience of early old-age and disability pensioners from unskilled-and semiskilled labour groups in Fredericia. Scand J Soc Med Suppl 16: 50-52.
- Dong X, Bergren SM, Chang ES (2015) Levels of acculturation of Chinese older adults in the Greater Chicago Area - The population study of Chinese elderly in Chicago. J Am Geriatr Soc 63: 1931-1937.
- Dong X, Zhang M, Simon MA (2014) The expectation and perceived receipt of filial piety among Chinese older adults in the Greater Chicago area. J Aging Health 26: 1225-1247.
- Li Y, Chi I, Krochalk PC, Xu L (2011) Widowhood, family support, and self‐rated health among older adults in China. Int J Soc Welf 20 Supplement s1: S72-S85.
- Fulmer T, Paveza G, VandeWeerd C, Fairchild S, Guadagno L, et al. (2005) Dyadic vulnerability and risk profiling for elder neglect. Gerontologist 45: 525-534.
- Gu D, Dupre ME, Warner DF, Zeng Y (2009) Changing health status and health expectancies among older adults in China: gender differences from 1992 to 2002. Soc Sci Med 68: 2170-2179.
- Liang Y, Song A, Du S, Guralnik JM, Qiu C (2014) Trends in disability in activities of daily living among Chinese older adults, 1997-2006: the China Health and Nutrition Survey. J Gerontol A Biol Sci Med Sci 70: 739-745.
- Welmer AK, Liang Y, Angleman S, Santoni G, Yan Z, et al. (2014) Vascular risk factor burden, atherosclerosis, and functional dependence in old age: a population-based study. Int J Behav Med 21: 597-604.
- Dong X, Chang ES, Simon M (2014) Physical function assessment in a community-dwelling population of US Chinese older adults. J Gerontol A Biol Sci Med Sci 69 (Suppl 2): S31-S38.
- Yang M, Jiang J, Li H1, Wu H, Dong B (2015) Association between waist circumference and self‐reported disability among Chinese adults aged 90 years and older. Geriatr Gerontol Int 15: 1249-1257.
- Yang M, Ding X, Luo L, Hao Q, Dong B (2014) Disability associated with obesity, dynapenia and dynapenic-obesity in Chinese older adults. J Am Med Dir Assoc 15: 150.
- Xu T, Zhang ZX, Han SM, Xiao XH, Gong XM, et al. (2009) Relationship between perinatal characteristics and later activities of daily living in Chinese elderly people. Chin Med J 122: 1015-1019.
- Chou KL, Leung JC (2008) Disability trends in Hong Kong community-dwelling Chinese older adults: 1996, 2000, and 2004. J Aging Health 20: 385-404.
- Beydoun MA, Popkin BM (2005) The impact of socio-economic factors on functional status decline among community-dwelling older adults in China. Soc Sci Med 60: 2045-2057.
- Zhang M, Zhu Z, Chen P (1998) Community investigation of the activities of daily living (ADL) and medical conditions of the elderly in Shanghai. Zhonghua Yi Xue Za Zhi 78: 124-127.
- Chen P, Yu ES, Zhang M, Liu WT, Hill R, et al. (1995) ADL dependence and medical conditions in Chinese older persons: a population‐based survey in Shanghai, China. J Am Geriatr Soc 43: 378-383.
- Feng L, Ng TP, He Y, Li C, Kua EH, et al. (2011) Physical health and cognitive function independently contributed to functional disability among Chinese older adults: data from two Asian metropolises. J Aging Res 2011: 960848.
- Ofstedal MB, Zimmer Z, Hermalin AI, Chan A, Chuang YL, et al. (2007) Short-term trends in functional limitation and disability among older Asians: a comparison of five Asian settings. J Cross Cult Gerontol 22: 243-261.
- Zeng P, Wu S, Han Y, Liu J, Zhang Y, et al. (2015) Differences in body composition and physical functions associated with sarcopenia in Chinese elderly: reference values and prevalence. Arch Gerontol Geriatr 60: 118-123.
- Yang Y, Wen M (2015) Psychological resilience and the onset of activity of daily living disability among older adults in China: A Nationwide longitudinal analysis. J Gerontol B Psychol Sci Soc Sci 70: 470-480.
- Zimmer Z, Martin LG, Chang MC (2002) Changes in functional limitation and survival among older Taiwanese, 1993, 1996, and 1999. Popul Stud 56: 265-276.
- Woo J, Ho SC, Yu LM, Lau J, Yuen YK (1998) Impact of chronic diseases on functional limitations in elderly Chinese aged 70 years and over: a cross-sectional and longitudinal survey. J Gerontol A Biol Sci Med Sci 53: M102-M106.
- Zimmer Z, Fang X, Tang Z (2013) Fifteen-year disability trends among older persons in the Beijing Municipality of China. J Aging Health 26: 207-230.
- Sun F, Park NS, Klemmack DL, Roff LL, Li Z (2009) Predictors of physical functioning trajectories among Chinese oldest old adults: rural and urban differences. Int J Aging Hum Dev 69: 181-199.
- Kaneda T, Zimmer Z, Fang X, Tang Z (2009) Gender differences in functional health and mortality among the Chinese elderly: Testing an exposure versus vulnerability hypothesis. Res Aging 31: 361-388.
- Auyeung TW, Lee SW, Leung J, Kwok T, Woo J (2014) Age‐associated decline of muscle mass, grip strength and gait speed: a 4‐year longitudinal study of 3018 community‐dwelling older Chinese. Geriatr Gerontol Int 14 Suppl 1: S76-S84.
- Wang TF, Chen IJ, Li IC (2012) Associations between chewing and swallowing problems and physical and psychosocial health status of long-term care residents in Taiwan: a pilot study. Geriatr Nurs 33: 184-193.
- Wong CH, Wong SF, Pang WS, Azizah MY, Dass MJ (2003) Habitual walking and its correlation to better physical function: implications for prevention of physical disability in older persons. J Gerontol A Biol Sci Med Sci 58: M555-M560.
- Thumboo J, Chew LH, Lewin-Koh SC (2002) Socioeconomic and psychosocial factors influence pain or physical function in Asian patients with knee or hip osteoarthritis. Ann Rheum Dis 61: 1017-1020.
- Meng P, Hu YX, Fan L, Zhang Y, Zhang MX, et al. (2014) Sarcopenia and sarcopenic obesity among men aged 80 years and older in Beijing: prevalence and its association with functional performance. Geriatr Gerontol Int 14 Suppl 1: 29-35.
- Zimmer Z, Martin LG, Nagin DS, Jones BL (2012) Modeling disability trajectories and mortality of the oldest-old in China. Demography 49: 291-314.
- Woo J, Ho SC, Yu AL (2000) The influence of income on morbidity, mortality and dependency in elderly Hong Kong Chinese. Arch Gerontol Geriatr 30: 55-61.
- Woo J, Leung J, Chan R, Chau PH (2013) Influence of income and self-rated socio-economic position on lifestyle, and physical and psychological function in older Chinese adults aged 65 years and over. Public Health 127: 878-881.
- Ho SC, Woo J, Yuen YK, Sham A, Chan SG (1997) Predictors of mobility decline: the Hong Kong old-old study. J Gerontol A Biol Sci Med Sci 52: M356-M362.
- Zimmer Z, Martin LG, Jones BL, Nagin DS (2014) Examining late-life functional limitation trajectories and their associations with underlying onset, recovery, and mortality. J Gerontol B Psychol Sci Soc Sci 69: 275-286.
- Zimmer Z, Liu X, Hermalin A, Chuang YL (1998) Educational attainment and transitions in functional status among older Taiwanese. Demography 35: 361-375.
- Chau S, Lai DW (2011) The size of an ethno-cultural community as a social determinant of health for Chinese seniors. J Immigr Minor Health 13: 1090-1098.
- Jiang J, Tang Z, Futatsuka M, Zhang K (2004) Exploring the influence of depressive symptoms on physical disability: a cohort study of elderly in Beijing, China. Qual Life Res 13: 1337-1346.
- Wang R, Chen L, Fan L, Gao D, Liang Z, et al. (2015) Incidence and effects of polypharmacy on clinical outcome among patients aged 80+: a five-year follow-up study. PloS One 10: e0142123.
- Yang M, Jiang J, Hao Q, Luo L, Dong B (2015) Dynapenic obesity and lower extremity function in elderly adults. J Am Med Dir Assoc 16: 31-36.
- Woo J, Leung J, Sham A, Kwok T (2009) Defining sarcopenia in terms of risk of physical limitations: a 5‐year follow‐up study of 3,153 Chinese men and women. J Am Geriatr Soc 57: 2224-2231.
- Cao L, Chen S, Zou C, Ding X, Gao L, et al. (2014) A pilot study of the SARC-F scale on screening sarcopenia and physical disability in the Chinese older people. J Nutr Health Aging 18: 277-283.
- Chau PH, Woo J, Lee CH, Cheung WL, Chen J, et al. (2011) Older people with diabetes have higher risk of depression, cognitive and functional impairments: implications for diabetes services. J Nutr Health Aging 15: 751-755.
- Woo J, Leung J, Kwok T (2007) BMI, body composition, and physical functioning in older adults. Obesity (Silver Spring) 15: 1886-1894.
- Liu CY, Wang SJ, Teng EL, Fuh JL, Lin CC, et al. (1997) Depressive disorders among older residents in a Chinese rural community. Psychol Med 27: 943-949.
- Auyeung TW, Kwok T, Lee J, Leung PC, Leung J, et al. (2008) Functional decline in cognitive impairment--the relationship between physical and cognitive function. Neuroepidemiology 31: 167-173.
- Huang CY, Hwang AC, Liu LK, Lee WJ, Chen LY, et al. (2016) Association of dynapenia, sarcopenia, and cognitive impairment among community-dwelling older Taiwanese. Rejuvenation Res 19: 71-78.
- Li Y, Zou Y, Wang S, Li J, Jing X, et al. (2015) A pilot study of the FRAIL scale on predicting outcomes in Chinese elderly people with type 2 diabetes. J Am Med Dir Assoc 16: 714.
- Woo J, Leung J, Lau E (2009) Prevalence and correlates of musculoskeletal pain in Chinese elderly and the impact on 4-year physical function and quality of life. Public Health 123: 549-556.
- Chien MY, Chen HC (2015) Poor sleep quality is independently associated with physical disability in older adults. J Clin Sleep Med 11: 225-232.
- Wu G, Zhao F, Zhou X, Wei L (2002) Improvement of isokinetic knee extensor strength and reduction of postural sway in the elderly from long-term Tai Chi exercise. Arch Phys Med Rehabil 83: 1364-1369.
- Wong AM, Lin YC, Chou SW, Tang FT, Wong PY (2001) Coordination exercise and postural stability in elderly people: effect of Tai Chi Chuan. Arch Phys Med Rehabil 82: 608-612.
- Chu LW, Chiu AY, Chi I (2006) Impact of falls on the balance, gait, and activities of daily living functioning in community-dwelling Chinese older adults. J Gerontol A Biol Sci Med Sci 61: 399-404.
- Lan TY, Wu SC, Chang WC, Chen CY (2009) Home environmental problems and physical function in Taiwanese older adults. Arch Gerontol Geriatr 49: 335-338.
- Lai DW, Tsang KT, Chappell N, Lai DC, Chau SB (2007) Relationships between culture and health status: a multi-site study of the older Chinese in Canada. Can J Aging 26: 171-183.
- Li N, Pang L, Chen G, Song X, Zhang J, et al. (2011) Risk factors for depression in older adults in Beijing. Can J Psychiatry 56: 466-473.
- Chen YY, Wong GH, Lum TY, Lou VW, Ho AH, et al. (2016) Neighborhood support network, perceived proximity to community facilities and depressive symptoms among low socioeconomic status Chinese elders. Aging Ment Health 20: 423-431.
- Ouyang Z, Chong AM, Ng TK, Liu S (2015) Leisure, functional disability and depression among older Chinese living in residential care homes. Aging Ment Health 19: 723-730.
- Lai DW (2005) Prevalence and correlates of depressive symptoms in older Taiwanese immigrants in Canada. J Chin Med Assoc 68: 118-125.
- Chi I, Yip PS, Chiu HF, Chou KL, Chan KS, et al. (2005) Prevalence of depression and its correlates in Hong Kong's Chinese older adults. Am J Geriatr Psychiatry 13: 409-416.
- Woo J, Ho SC, Lau J, Yuen YK, Chiu H, et al. (1994) The prevalence of depressive symptoms and predisposing factors in an elderly Chinese population. Acta Psychiatr Scand 89: 8-13.
- Lai DW (2004) Depression among elderly Chinese-Canadian immigrants from Mainland China. Chin Med J (Engl) 117: 677-683.
- Auyeung TW, Lee JS, Kwok T, Woo J (2011) Physical frailty predicts future cognitive decline-a four-year prospective study in 2737 cognitively normal older adults. J Nutr Health Aging 15: 690-694.
- Wu YH, Liu LK, Chen WT, Lee WJ, Peng LN, et al. (2015) Cognitive function in individuals with physical frailty but without dementia or cognitive complaints: results from the I-Lan longitudinal aging study. J Am Med Dir Assoc 16: 899.
- Woo J, Ho SC, Lau S, Lau J, Yuen YK (1994) Prevalence of cognitive impairment and associated factors among elderly Hong Kong Chinese aged 70 years and over. Neuroepidemiology 13: 50-58.
- Chu CL, Liang CK, Chow PC, Lin YT, Tang KY, et al. (2011) Fear of falling (FF): Psychosocial and physical factors among institutionalized older Chinese men in Taiwan. Arch Gerontol Geriatr 53: e232-e236.
- Chen YM, Hwang SJ, Chen LK, Chen DY, Lan CF (2008) Risk factors for falls among elderly men in a veterans home. J Chin Med Assoc 71: 180-185.
- Woo J, Leung J, Wong S, Kwok T, Lee J, et al. (2009) Development of a simple scoring tool in the primary care setting for prediction of recurrent falls in men and women aged 65 years and over living in the community. J Clin Nurs 18: 1038-1048.
- Zhang W, Shen S, Wang W, Zhou C, Xu L, et al. (2014) Poor lower extremity function was associated with pre-diabetes and diabetes in older Chinese people. PloS One 9: e115883.
- Woo J, Ho SC, Sham A, Yuen YK, Chan SG (1995) Influence of age, disease and disability on anthropometric indices in elderly Chinese aged 70 years and above. Gerontology 41: 173-180.
- Woo J, Ho SC, Yu AL (1999) Walking speed and stride length predicts 36 months dependency, mortality, and institutionalization in Chinese aged 70 and older. J Am Geriatr Soc 47: 1257-1260.
- Zhang W, Ding H, Su P, Duan G, Chen R, et al. (2016) Does disability predict attempted suicide in the elderly? A community-based study of elderly residents in Shanghai, China. Aging Ment Health 20: 81-87.
- Chan HL, Liu CY, Chau YL, Chang CM (2011) Prevalence and association of suicide ideation among Taiwanese elderly--a population-based cross-sectional study. Chang Gung Med J 34: 197-204.
- Yip PS, Chi I, Chiu H, Chi Wai K, Conwell Y, et al. (2003) A prevalence study of suicide ideation among older adults in Hong Kong SAR. Int J Geriatr Psychiatry 18: 1056-1062.
- Zou C, Zhou Y, Dong B, Hao Q, Chen S, et al. (2015) Predictors of 49-month mortality in Chinese nonagenarians and centenarians in PLAD study. Aging Clin Exp Res 27: 821-827.
- Feng Q, Hoenig HM, Gu D, Yi Z, Purser JL (2010) Impact of new disability subtypes on 3-year mortality in Chinese older adults. J Am Geriatr Soc 58: 1952-1958.
- Zimmer Z, Martin LG, Lin HS (2005) Determinants of old-age mortality in Taiwan. Soc Sci Med 60: 457-470.
- Kim G, Chiriboga DA, Jang Y, Lee S, Huang CH, et al. (2010) Health status of older Asian Americans in California. J Am Geriatr Soc 58: 2003-2008.
- Dong X, Li Y, Simon MA (2014) Social engagement among US Chinese older adults--findings from the PINE study. J Gerontol A Biol Sci Med Sci 69 Suppl 2: S82-S89.
- Nguyen D (2011) Acculturation and perceived mental health need among older Asian immigrants. J Behav Health Serv Res 38: 526-533.
- Min JW, Rhee S, Lee SE, Rhee J, Tran T (2014) Comparative analysis on determinants of self-rated health among non-Hispanic White, Hispanic, and Asian American older adults. J Immigr Minor Health 16: 365-372.
- Mui AC, Kang SY (2006) Acculturation stress and depression among Asian immigrant elders. Soc Work 51: 243-255.
- Feng Q, Zhen Z, Gu D, Wu B, Duncan PW, et al. (2013) Trends in ADL and IADL disability in community-dwelling older adults in Shanghai, China, 1998-2008. J Gerontol B Psychol Sci Soc Sci 68: 476-485.
- Nagi SZ (1976) An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc 54: 439-467.
- Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA (1996) Successful aging: predictors and associated activities. Am J Epidemiol 144: 135-141.
- Liu X, Liang J, Muramatsu N, Sugisawa H (1995) Transitions in functional status and active life expectancy among older people in Japan. J Gerontol B Psychol Sci Soc Sci 50: S383-S394.
- Seeman TE, Berkman LF, Charpentier PA, Blazer DG, Albert MS, et al. (1995) Behavioral and psychosocial predictors of physical performance: MacArthur studies of successful aging. J Gerontol A Biol Sci Med Sci 50: M177-M183.
- Kiel DP, O'Sullivan P, Teno JM, Mor V (1991) Health care utilization and functional status in the aged following a fall. Med Care 29: 221-228.
- Rogers MW, Mille ML (2003) Lateral stability and falls in older people. Exerc Sport Sci Rev 31: 182-187.
- Taş U, Verhagen AP, Bierma-Zeinstra SM, Hofman A, Odding E, et al. (2007) Incidence and risk factors of disability in the elderly: the Rotterdam study. Prev Med 44: 272-278.
- LaCroix AZ, Guralnik JM, Berkman LF, Wallace RB, Satterfield S (1993) Maintaining mobility in late life. II. Smoking, alcohol consumption, physical activity, and body mass index. Am J Epidemiol 137: 858-869.
- Dong X, Simon M, Fulmer T, Mendes de Leon CF, Rajan B, et al. (2010) Physical function decline and the risk of elder self-neglect in a community-dwelling population. Gerontologist 50: 316-326.
- Zhang M, Simon MA, Dong X (2014) The prevalence of perceived stress among US Chinese older adults. 1: 40-56.
- Simon MA, Chang ES, Zang M, Ruan J, Dong X (2014) The prevalence of loneliness among US Chinese older adults. J Aging Health 26: 1172-1188.
- Dong X, Chen R, Wong E, Simon MA (2014) Suicidal ideation in an older US Chinese population. J Aging Health 26: 1189-1208.
- Dong X, Chen R, Simon MA (2014) Anxiety among community-dwelling US Chinese older adults. J Gerontol A Biol Sci Med Sci 69(Suppl 2): S61-S67.
- Dong X, Chen R, Li C, Simon MA (2014) Understanding depressive symptoms among community-dwelling Chinese older adults in the greater Chicago area. J Aging Health 26: 1155-1171.
- Guralnik JM, Ferrucci L (2003) Assessing the building blocks of function: utilizing measures of functional limitation. Am J Prev Med 25(3 Suppl 2): 112-121.
- Cress ME, Buchner DM, Questad KA, Esselman PC, deLateur BJ, et al. (1996) Continuous-scale physical functional performance in healthy older adults: a validation study. Arch Phys Med Rehabil 77: 1243-1250.
- Kuriansky JB, Gurland BJ, Fleiss JL, Cowan D (1976) The assessment of self-care capacity in geriatric psychiatric patients by objective and subjective methods. J Clin Psychol 32: 95-102.
- Dong X, Chen R, Simon MA (2014) The prevalence of medical conditions among US Chinese community-dwelling older adults. J Gerontol A Biol Sci Med Sci 69(Suppl 2): S15-S22.
- Rudberg MA, Furner SE, Dunn JE, Cassel CK (1993) The relationship of visual and hearing impairments to disability: an analysis using the longitudinal study of aging. J Gerontol 48: M261-M265.
- Conwell Y, Duberstein PR, Caine ED (2002) Risk factors for suicide in later life. Biol Psychiatry 52: 193-204.
- Awata S, Seki T, Koizumi Y, Sato S, Hozawa A, et al. (2005) Factors associated with suicidal ideation in an elderly urban Japanese population: a community‐based, cross‐sectional study. Psychiatry Clin Neurosci 59: 327-336.
- Mancini AD, Bonanno GA (2006) Marital closeness, functional disability, and adjustment in late life. Psychol Aging 21: 600-610.
- Koenig HG, George LK (1998) Depression and physical disability outcomes in depressed medically ill hospitalized older adults. Am J Geriatr Psychiatry 6: 230-247.
- Jang M, Lee E, Woo K (1998) Income, language, and citizenship status: factors affecting the health care access and utilization of Chinese Americans. Health Soc Work 23: 136-145.
- 155. Bean FD, Stevens G (2003) America's newcomers and the dynamics of diversity. Russell Sage Foundation.
- Kagawa-Singer M, Hikoyeda N, Tanjasiri S (1997) Aging, chronic conditions, and physical disabilities in Asian and Pacific Islander Americans. In: Minorities, aging, and health. pp. 149-180.
- Comijs HC, Smit JH, Pot AM, Bouter LM, Jonker C (2008) Risk indicators of elder mistreatment in the community. J Elder Abuse Neglect 9: 67-76.
- Dong X, Simon MA (2010) Is impairment in physical function associated with increased risk of elder mistreatment? Findings from a community-dwelling Chinese population. Public Health Rep 125: 743-753.
- Dong X, Chang ES, Bergren S (2014) The burden of grandparenting among Chinese older adults in the Greater Chicago area-The PINE study. AIMS Med Sci 1: 125-140.
- Alhajj T, Wang L, Wheeler K, Zhao W, Sun Y, et al. (2010) Prevalence of disability among adolescents and adults in rural China. Disabil Health J 3: 282-288.
- Woo J, Ho SC, Yuen YK, Yu LM, Lau J (1996) An estimation of the functional disability burden in elderly Chinese age 70 years and over. Disabil Rehabil 18: 609-612.
- Woo J, Zhang XH, Ho S, Sham A, Tang Z, et al. (2008) Influence of different health‐care systems on health of older adults: a comparison of Hong Kong, Beijing urban and rural cohorts aged 70 years and older. Australas J Ageing 27: 83-88.