Luciana Laganà, Department of Psychology, California State University Northridge, 18111 Nordhoff Street 8255, Building Sierra Tower, Room 314, 91330, Northridge, CA, USA, Tel: 818 677 2827; Fax: 818 677 2829; E-mail:
Citation: Laganà L, Prilutsky RR. A Pilot Psychometric Study on the Validation of the Older Women’s Non-Medical Stress Scale (OWN-MSS) on an Ethnically Diverse Sample. J Geriatrics Palliative Care 2016;4(1): 7.
Copyright © 2016 Laganà L, Prilutsky R R. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reviewed & Approved by: Dr. Wang Wenru, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Journal of Geriatrics and Palliative Care | ISSN: 2373-1133 | Volume: 4, Issue: 1
Submission: 05 November 2015 | Accepted: 19 January, 2016 | Published: 23 January 2016
Abstract
Introduction: Older women often experience various types of stressors, including the death of a spouse and associated financial stress (often with a lack of social support), emotional stress due to factors such as caregiving and being single, and the challenges of the aging process. These circumstances could produce or aggravate anxious symptomatology that can in turn compound the negative effects of aging. A brief scale of perceived stress that is not confounded with health status and covers multiple culturally relevant potential stressors is needed for quick use in busy medical settings.
Aim: To assess the reliability and the validity of an original stress scale designed to measure perceptions of stress beyond health status in a non-clinical convenience sample of community-dwelling older women.
Method: In this cross-sectional pilot investigation, via conducting item-total correlations and correlational tests of validity, we studied the psychometric properties of our measure using data from volunteer older subjects (mainly low-income and from non-Caucasian backgrounds). he domains covered by the nine items of the tool were selected based on a literature review of common stressors experienced byolder adults, especially by older women. Data were collected face-to-face using a demographic list, a well-established depression measure, a brief posttraumatic stress disorder (PTSD) screener, and our 9-item stress tool. Primary outcomes: reliability and validity of the scale of older women’s non-medical stress. Secondary outcomes: demographic characteristics of the sample and correlations between stress items.
Results: Based on our sample of older women (N=40, mean age 71 years), good internal consistency between the items of the stress scale was found (Cronbach’s α=.66). The findings of the data analyses also revealed that our psychometric tool has good convergent validity with the PTSD screener (r=.53). Moreover, in contrast with most other stress tools, it has strong discriminant validity (r=.11) with a well-validated depression scale.
Conclusion: Our results suggest that this new measure is psychometrically strong. Future research directions encompass using larger samples, ideally including older men with the modification of the scale’s name, as well as validating this tool against more measures. Clinical implications of our findings are briefly discussed.
Keywords
Older adults; Stress; Assessment; Psychometrics; Allostatic load; Depression; PTSD
Introduction
The aim of this community-based pilot study was to test whether an original non-medical stress tool is reliable and valid for use with ethnically diverse older women. The way in which stress is handled in older age is an intriguing and relatively unexplored topic amongmultiethnic older adults, which should be studied further via using measures developed specifically for them. Stressors beyond health status are numerous, and reactions to them are highly personal, as briefly highlighted here. Research published in 2015 [
1] suggests that older women, as compared to older men, report higher levels of stress, making them a research population that should receive more attention when studying perceived stress.
Stress related to having health problems is not typically targeted separately from stress that is not of a medical nature (which is often a health risk factor); this is a methodological challenge discussed herein. We have defined non-medical stress as perceived stressexperienced in response to challenging circumstances that do not involve experiencing medical problems. Geriatric research by the first author [
2] on ethnically diverse older women has linked worse general health to higher”non-medical” stress, measured by using the stress tool tested herein. Interestingly, while perceived stress significantly predicted worse general health but not role limitations, PTSD symptomatology predicted limitations in role fulfillment but not worse health. These findings suggest that PTSD symptomatology and perceived non-medical stress could impact physical health dimensions differentially in older age. More research is needed on this topic. Thus, the initial validation of our non-medical stress scale and its widespread distribution represents a significant contribution to thefield of ethnogeriatric psychometrics. Moreover, the present research complements the aforementioned work done by the first author by including an examination of the relationship between non-medical stress and depressive symptomatology. Given that non-medical stress appears to significantly predict physical health, it is important to study whether it is also significantly related to depressive symptoms.
It should be noted that an important aspect of stress is its subjective perception: a classic cognitive-phenomenological conceptualization emphasizes that a person must perceive a demand or stressor and experience some degree of tension to respond with stress [
3]. With respect to the present psychometric study, recognition of events as personally stressful is what our toolassesses. Perceived stress accounts for variations among responses provided by people who, although experiencing the same potentially stressful events, could be affected by these events differently [
4]. Thus, assessing perceived stress could be even more informative than simply assessing occurrence of potentially distressing life events, as perceived stress provides information on the impact of stressors on mental as well as physical health [
5].
To the authors’ knowledge, no stress measure is currently published that was created exclusively to quantify the perceived impact of multiple potential stressors that are likely to be faced by older women from diverse racial/ethnic backgrounds. A few measures assess specific stressors, such as the pressure of engaging in caregiving (e.g., the “Caregiver Strain Index” [
6]), without assessing the perceived stress induced by other pivotal pressures. Stress scalescreated specifically for older adults, such as the Stress Scale for Elderly Patients with Coronary Artery Disease [
7], are designed to be utilized in health care settings on specific medical patient populations. Nongeriatric instruments that quantify more general domains of stress include the “Dimensions of Stress Scale” [
8], which focuses primarily on perceptions of stressor salience and control over stressors; thewidely used “Perceived Stress Scale” [
9], which investigates thoughts and feelings regarding stressful circumstances; and the “Stress Emotions Questionnaire” [
10], which assesses how individuals appraise stressful environmental transactions such as challenges and threats. The Life Experience Survey (LES) [
11] is another tool used to quantify the impact of stressful events. It is a 57-item self-report measure, a very long assessment tool for use in older age, and it assesses frequency and impact of commonly occurring events such as marriage, births, deaths, and job changes exclusively within the past year.
Problematically, existing stress tools are confounded with health status, as they typically contain items assessing stress caused by physical health problems. Most importantly, they are not designed to assess stress levels in older age by tailoring the selection of thestressors to older adults while keeping the scale reasonably short for use with this population. One of the notable exceptions is the Elders Life Stress Inventory (ELSI), designed by Aldwin to measure nonmedical life stress levels among older adults [
12]. This instrument is well-researched and has good psychometric properties [
13]. However, as opposed to our stress tool, it is very lengthy with 30 items, is not specific to older women, and is not designed to tease out the effects of several culturally important factors such as geographical distance from family and friends, which is common in areas such as Los Angeles County where this pilot study was conducted. Furthermore, unlike our stress tool, the queries of the ELSI assume that major caregiving responsibility is exclusively for aging parents. However, as highlighted in 2015 by Abramson, older adults often engage in caregiving for a variety of family members and/or friends; this is especially the case within non-Caucasian cultures [
14,15]. Consequently, the use of our stress tool, once its psychometric properties are tested, will allow researchers and clinicians to assess many understudied issues important to the lives of ethnically diverse older women.
A particularly significant factor that is missing in other measures of stress is the recognition that, although apparently distressing, not all potentially stressful events and circumstances are experienced as stressful, given that perceived stress is, by definition, a very personal experience. To recognize the subjective nature of stress, backed by the findings of the geriatric literature briefly reviewed next, we have chosen Erikson’s construct of generativity applied to stress in older age as the theoretical foundation for this stress measure [
16]. Erikson’s theorization highlights a developmental shift that occurs in middle to older age toward increased generativity that, according to Aldwin, should be mirrored in older adults’ stress processes [
12].
When does a potentially stimulating social situation become a stressor in older age? Aldwin conceptualized that, as they grow older, many people do not focus solely on egocentric stressors (i.e., circumstances that harm or threaten the self such as financial problems), but also on external values like providing caregiving to those in need and interacting with friends and family [
12]. These ircumstances, although potentially stressful when perceived as too demanding (e.g., providing strenuous caregiving) or aversive (e.g., being geographical isolated or having unsupportive friends), can offer older adults an avenue to later-life social contribution [
17] and are likely to be especially valued by ethnic minority older adults, in line with their often-collectivistic cultural values. To offer an example: apotentially stressful event, such as having to provide caregiving to one or more family members in older age, could be viewed by an older woman as a rewarding task affirming her contribution to her family, instead of being experienced as subjectively stressful. However, especially when linked to a cumbersome view of caregiving or to disadvantageous demographic factors like poor financial means, the same task could be perceived as a chronic strain producing significant stress. In this regard, culture-based justifications for caregiving have been found to predict psychosocial health among African-American caregivers [
18] and are likely to affect whether caregiving is perceived as stressful or rewarding in older age.
Our stress scale contains nine items whose answers are added up to calculate a total stress score. This implies that the effects of perceived stress are additive, in line with the concept of stress proliferation [
19,20]. The death of a husband who provided steady financial support could induce significant emotional stress related to bereavement as well as financial stress and is an example of stress proliferation. Losing husband-related social ties could introduce novel unbearable financial stress as well as social stress, thereby proliferating into other areas of life and causing secondary hardship that could be psychologically disruptive. Thus, when researching the stress process in older age, it is important to take into account the effects of multiple potentially stressful situations, as well as the structural forms of older adults’ families and their economic and social circumstances [
21], as done in our brief stress tool.
Another potential stressor typically ignored in geriatric research is the process of growing older. This topic has been studied with regard to its potential to hinder the ability to attain resources needed to meet desired goals, which in turn has been associated with perceived stress [
22]; however, research is still lacking on the perceived impactof growing older on older women’s perceived stress levels. To our knowledge, there are no studies conducted on ethnically diverse older women concerning this potential stressor. Additionally, aversive social support is a potential cause of stress in older age. In this regard, Kim and Nesselroade studied the relationships between social support, self-concept, as well as perceived physical and psychological well-being among older adults [
23]. Their findings demonstrated that negative social support both directly and indirectly impacts physical health as a result of a more negative self-concept, making the assessment of perceived stress due to aversive friendships a topic worthy of being included in our stress scale.
To summarize, developing the measure tested herein involved taking into account non-medical potential stressors that are commonly experienced in older age, such as: providing caregiving, living far away from loved ones, having financial difficulties, being single, having financial and emotional stress following the death of a spouse, experiencing a challenging aging process, and perceiving one’s network of friends as too limited or stressful. Our stress tool assesses avariety of dimensions of stress that are often individually and distinctly investigated in some of the available stress measures. In fact, a major setback in many studies throughout the field of geriatric stress is the use of several questionnaires to assess different stress domains. Such methods are costly, time-inefficient, and could fatigue older adults. Fatigue is an important factor to consider in studies on older subjects, as it can hinder their recruitment for research participation. Having developed this brief stress scale represents an attempt to minimize these concerns. Moreover, physical health is a confounder in most of the existing instruments of this kind, with only one of them being designed specifically for the assessment of non-medical stress in older adults, and none for older women in particular. Thus, testing the psychometric properties of this brief tool and making it available tothe public could be useful to geriatric researchers and practitioners in future research and clinical endeavors.
Methods
This research was approved by the Institutional Review Board of California State University Northridge (CSUN). We used a sample of convenience; non-institutionalized older women were recruited at locations such as churches, shops, libraries, and parks in Los Angeles County.
Setting and Population
Older women residing in the community were invited to participate. Forty women consented. Inclusion criteria were that subjects be at least 50 years of age, which, according to the American Association of Retired Persons [
24], is acceptable as being considered f older status. To minimize the chances of recruiting subjects with severe cognitive impairment that could have affected response accuracy, criteria for exclusion from study participation included any of the following: (a) residing in an institutional setting or (b) being unable or unwilling to provide informed consent for any reason.
Research assistants/interviewers were trained extensively by the first author to enhance their assessment and interpersonal skills for this study. They were tasked with recruiting older women from their respective communities. Once recruited, respondents were asked to suggest other older women of similar background to participate inthe study. In order to promote the comfort of participants, research assistants were instructed to be accommodating when arranging locations and times for the interviews to be held.
Procedure
Once each older woman qualified to be included in the study, individual assessment sessions took place at a convenient time and place for each participant. The assessment battery covered demographics (i.e., age, ethnicity, marital status, and income), perceived stress, as well as PTSD and depressive symptomatology. Allsubjects were given ample time to answer the assessment questions and were asked to provide informed consent, which gave the older women the right to withdraw from the study at any time.
Assessment tools
A Brief Demographics List was used to assess demographic information. This succinct unpublished list, developed by the first author, contains 4 items inquiring into age, race and ethnicity, income, and marital status.
The SelfCARE(D) [
25] was used to correlate depressive symptomatology with perceived stress. This 12-item scale has each item scored as a 0 or 1, with scores ranging from 0 to 12. The SelfCARE (D) is specifically intended for use with non-institutionalized older adults [
26] and has demonstrated to be a reliable and valid scale [
25-27]. Thus, it was ideal for use in the present study.
The Brief Posttraumatic Stress Screening Scale (BPSSS) [
28] was used to relate PTSD symptomatology to perceived stress. This is the first author’s abbreviated version of the well-established 20-item Distressing Event Questionnaire (DEQ) [
29], a strong measure created to assess PTSD symptomatology. The BPSSS quantifies posttraumatic stress reactions that occurred within the past month in response to an unspecified, most distressing experience. Subjects are asked to refer to this experience when answering Likert-type scaleitems. Scores range from 0, i.e., absent or did not occur, to 4, i.e., present to an extreme or severe degree. This brief PTSD screener contains five items and, in line with the DSM-IV-TR [
30], utilizes a) two items to measure criterion B: re-experiencing, b) two items to assess criterion C: avoidance/numbing, and c) one item to assesscriterion D: increased arousal.
The Older Women’s Non-Medical Stress Scale (OWN-MSS), our perceived stress tool, is a 9-item measure assessing how emotionally stressful it is to: provide caregiving to family/friends, be single orwidowed, experience financial difficulties in general, grow older/the aging process, have a stressful network of friends, experience the death of a spouse and financial stress related to it, as well as not have enough friends to rely on or not enough family members close in proximity.Items are rated using a Likert scale quantifying how emotionally stressful the particular stressor is perceived to be. Scores range from 0 - not at all to 5 - extremely, with the option of choosing n/a if the stressor is not applicable. As previously mentioned, the particular domains covered by the nine items were deliberately selected, as they were based on a literature review of common stressors experienced by older adults, and by older women in particular. This scale has been used successfully in an aforementioned study on older women’s physical health as it relates to psychopathology such as stress and PTSD [
2].
Hypotheses
The stress scale was expected to be a reliable instrument with moderate internal consistency (in view of the variety of stressors assessed). As to validity, we expected to demonstrate good discriminant validity between our stress scale and a depression measure. Further, it was hypothesized that a moderate correlationwould be found between scores on the stress scale and on the first author’s PTSD symptomatology screener, due to their partial conceptual overlap.
Results
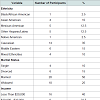
All statistical analyses were conducted utilizing SPSS for Windows version 20. Subject characteristics were computed (
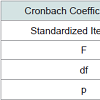
Table 1). As shown in
Table 2, an internal consistency reliability analysis was performed; the analysis of variance (ANOVA) demonstrated overall statistical significance. This finding indicates strong internal consistency, especially in view of the small number of items contained in the stress scale and the variety of potential stressors covered.
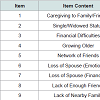
The item-total statistics in
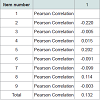
Table 3 show the alpha values if each item was deleted. Moderate correlations between stress items were found, as expected:
Table 4 illustrates the correlations between items within an inter-item correlational matrix.
As can be seen in
Table 5, the stress measure has strong discriminant validity when compared to a well-validated depression measure, as no significant relationship existed between the SelfCARE(D) and our stress tool. Additionally, convergent validitywas found to be good regarding the stress scale and the PTSD symptomatology screener: there are converging properties between these two measures, supporting the hypothesis that the stress tool does tap PTSD symptomatology to a certain degree.
Figure 1 contains our perceived stress scale.
Discussion
The initial test of the reliability and validity of our non-medical stress scale was successful. Findings supported the proposed hypotheses and demonstrated that this tool has solid psychometric properties, especially considering its small size and the large variety of potential stressors included. Researchers could investigate whetherthis scale is reliable and valid when used with older men. If studies support this, scholars will be able to test gender differences relative to older adults’ stressors through utilizing this measure. The items of our stress tool correlate relatively well with one another, with a statistically significant internal consistency. Considering that such items assess different domains, it was expected that there would be amoderate correlation among them. These findings justify conducting a psychometric study on a larger scale on this topic.
Concerning validity testing against a depression measure, results were very promising. Innovatively, our stress scale was shown to be free from confounding factors when compared to a well-researched depression scale. For the interested reader, other stress scales havebeen reported in the literature to be associated with depression, for instance the Severity of HIV-Related Life Problems Scale [
31]. Our research sample was very ethnically diverse and primarily lowincome, and yet levels of distress were not related to depression. This result suggests that, although burdened by many challenging circumstances, older women do not necessarily develop depression associated with them, as resilience is high within this population. Research is needed to verify this.
As expected, the relationship between older women’s stress and PTSD symptomatology was significant, although not large. This result corroborates prior empirical findings on this topic, such as research conducted using the Elders’ Life Stress Inventory [
12] andthe Harvard Trauma Questionnaire (HTQ) [
32]. The strength of this relationship was moderate in our sample, as several subjects, even though they faced many distressing life circumstances, did not report PTSD symptomatology. This result matches the findings of other investigators such as van der Kolk, McFarlane, and Weisaeth who found that, of the individuals who do experience a traumatic stressor such as the loss of a spouse, only one third of them develops PTSD [
33]. In line with this report, we did not expect the degree of association between the stress tool and the PTSD measure to be verystrong, potentially indicating that there are other factors involved in inducing PTSD in older women.
Individual differences including resilience and vulnerability may play a strong role in our finding relative to the stress-PTSD link. In fact, research shows that individual differences influence the development of PTSD even when the same degrees of stress areexperienced, as factors outside of genetic predisposition may affect the development of PTSD and impact resilience to trauma, including social support, trauma severity, and previous history of trauma (i.e., child abuse) [
33].
This study has several limitations that are typical of pilot research of this kind. They include recruiting subjects only in Los Angeles County (which limits the generalizability of the findings), not using random sampling techniques (therefore, selection bias may exist), nothaving assessed additional demographics such as educational levels, and not being able to examine racial differences due to the limited number of participants per racial group. It should also be noted that a) acute stressful events do not necessarily result in immediate troublesome anxiety states and b) do not always raise anxietyeventually; this is a limitation of many stress scales. In addition, perhaps some of our respondents experienced medical stress, but this was not assessed because it was beyond the focus of the present psychometric study. Moreover, a small convenience sample was used; as larger samples would allow better generalizations, future investigations should be designed for this purpose. Also, only older women were recruited; researchers should examine the psychometricproperties of this tool on samples of older men as well. If testing is successful, then the name of the scale should be modified to reflect its use with both older men and women. Among other limitations is the study’s reliance upon self-reports. Additionally, our research is thus subject to the drawbacks of this methodology, such as the fact that variance may exist in the expression of emotional distress and depressive symptomatology. This is a pitfall common to most studies in this research area. As in the vast majority of existing literature within this realm of research, we employed a cross-sectional design, which did not allow for determination of causation effects among variables. This is the most common approach to the study of aging because, in comparison to other designs, it allows data to be gathered more easily and minimizes fatigue among older research participants, as well as the related chance of a high attrition rate. Considering allof these factors, such a design was deemed most appropriate for the achievement of this study’s aims. Finally, in order to keep the scale as brief as possible, we have not covered complex and population-specific potential stressors such as ageism, racial/ethnic discrimination, or heterosexism, which can be carefully assessed separately.
Clinical and research directions include the need to study larger samples regarding whether reactions to stressful events in older age differ as a function of gender, geriatric age sub-groups, and race/ ethnicity (as these questions were beyond the scope of this pilot study). Moreover, interested scholars should test the feasibility of using this scale as a screener in busy clinical practices and should establish clinical cut-off scores to identify older patients living with overwhelming stress. Future studies on larger samples should include ore rigorous analyses such as factor analysis. Moreover, to test this scale’s differential capability to quantify non-medical stress and to further validate it, its scores should be compared to scores on a well-established geriatric stress scale such as the Elderly Life Stress Inventory [
12]. Also, researchers should clarify the difference between psychological stress due to non-medical causes and stress due to medical physical condition(s). When we asked older subjects to selfreport stress of a non-medical nature, it was found that their stress levels were not related to psychological problems such as depressive symptomatology. To assume that stressors of a medical and nonmedical nature should be assessed simultaneously is a confounding that should be carefully minimized, because once the total stress score is computed, medical and non-medical factors impacting stress responses can no longer be separated.
Conclusion
In summary, although factors such as potential selection biases limit the generalizability of our findings, the results of this pilot study are promising regarding the reliability and validity of our nonmedical stress tool. This is especially true due to the discovery that this scale is not confounded with depressive symptomatology, unlike many of the available stress tools. The next step includes attempting to duplicate these findings on larger samples, comparing scores on this measure to those on a gold standard stress measure, identifying clinical cut-off scores for our scale, and testing this measure on older men. In particular, a strong effort should be made to recruit racial/ ethnic minorities in numbers large enough to be able to implement racial/ethnic comparisons. To our knowledge, this was the first study to test the psychometric properties of a short scale of non-medical stress created specifically for ethnically diverse older women.
Acknowledgements
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under award number SC3GM094075, Luciana Laganà, Principal Investigator. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We also wish to acknowledge Prof. Scott Plunkett and the students enrolled in the first author’s gerontology classes and research laboratory for their contribution to this study.
References
- Osmanovic-Thunstrom A, Mossello E, Akerstedt T, Fratiglioni L, Wang HX (2015) Do levels of perceived stress increase with increasing age after age 65? A population-based study. Age Ageing 44: 828-834.
- Laganà L, Reger SL (2009) A pilot study on perceived stress and PTSD symptomatology in relation to four dimensions of older women's physical health. Aging Ment Health 13: 885-893.
- Hennon CB, Brubaker TH (1994) Divorce and health care in later life. In: Schwartz LL, (Ed). Mid-life divorce counseling. Family psychology and counseling series, American Counseling Association, Alexandria, VA, pp. 39-63.
- Landrine H, Klonoff EA, Corral I, Fernandez S, Roesch S (2006) Conceptualizing and measuring ethnic discrimination in health research. J Behav Med 29: 79-94.
- Vines AI, Ta M, Esserman D, Baird DD (2009) A comparison of the occurrence and perceived stress of major life events in black and white women. Women Health 49: 368-380.
- Robinson BC (1983) Validation of a caregiver strain index. J Gerontol 38: 344-348.
- Choi YO, Kim JS (2014) Development of a stress scale for elderly patients with coronary artery disease. J Korean Acad Nurs 44: 630-638.
- Vitaliano PP, Russo J, Weber L, Celum C (1993) The dimensions of stress scale: psychometric properties. J Appl Soc Psychol 23: 1847-1878.
- Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24: 385-396.
- Folkman S, Lazarus RS (1986) Stress-processes and depressive symptomatology. J Abnorm Psychol 95: 107-113.
- Sarason IG, Johnson JH, Siegel JM (1978) Assessing the impact of life changes: development of the Life Experiences Survey. J Consult Clin Psychol 46: 932-946.
- Aldwin CM (1990) The Elders Life Stress Inventory: Egocentric and nonegocentric stress. In: Stephens MA, Crowther JH, Hobfoll SE, Tennenbaum DL (Eds). Stress and coping in later-life families, Taylor & Francis, Florence, KY, pp. 49-69.
- Aldwin CM (1991) The Elders Life Stress Inventory (ELSI): Research and clinical applications. In: Keller PA (Ed). Innovations in clinical practice: A source book, Professional Resource Press, Sarasota, FL, 10: 355-364.
- Abramson TA (2015) Older adults: The "Panini Sandwich" generation. Clin Gerontol 38: 251-267.
- Ahn S, Hochhalter AK, Moudouni DK, Smith ML, Ory MG (2012) Self-reported physical and mental health of older adults: the roles of caregiving and resources. Maturitas 71: 62-69.
- Erikson EH (1953) Childhood and society. Norton Press, New York.
- James A, James WL, Smith HL (1984) Reciprocity as a coping strategy of the elderly: a rural Irish perspective. Gerontologist 24: 483-489.
- Dilworth-Anderson P, Goodwin PY, Williams SW (2004) Can culture help explain the physical health effects of caregiving over time among African American caregivers? J Gerontol B Psychol Sci Soc Sci 59: S138-S145.
- Pearlin LI (1999) Stress and mental health: A conceptual overview. In: Horwitz AV, Scheid TL, (Eds). A handbook for the study of mental health: Social contexts, theories, and systems: Cambridge University Press, New York, pp. 161-175.
- Pearlin LI, Pioli MF, McLaughlin AE (2001) Caregiving by adult children: Involvement, role disruption, and health. In: Binstock RH, George LK (Eds). Handbook of aging and the social sciences, (5th edn). Academic Press, San Diego, CA, pp. 238-254.
- Pearlin LI, Skaff MM (1998) Perspectives on the family and stress in late life. The Plenum series in adult developing and aging. In: Lomranz J (Ed). Handbook of aging and mental health: An integrative approach, Plenum Press, New York. pp. 323-340.
- Brandtstädter J, Rothermund K (2002) The life-course dynamics of goal pursuit and goal adjustment: a two-process framework. Dev Rev 22: 117-150.
- Kim JE, Nesselroade JR (2003) Relationships among social support, self-concept, and wellbeing of older adults: a study of process using dynamic factor models. Int J Behav Dev 27: 49-65.
- AARP (2015) American Association of Retired Persons.
- Bird AS, MacDonald AJ, Mann AH, Philpot MP (1987) Preliminary experience with the SelfCARE (D): a self-rating depression questionnaire for use in elderly, non-institutionalized subjects. Int J Geriatr Psychiatry 2: 31-38.
- Abas M, Hotopf M, Prince M (2002) Depression and mortality in a high-risk population: 11-year follow-up of the Medical Research Council Elderly Hypertension Trail. Br J Psychiatry 181: 123-128.
- Banerjee S, Shamash K, MacDonald AJ, Mann AH (1998) The use of the SelfCARE(D) as a screening tool for depression in the clients of local authority home care services--a preliminary study. Int J Geriatr Psychiatry 13: 695-699.
- Laganà L, Schuitevoerder S (2009) Abbreviated posttraumatic stress screen for ethnically diverse older women. Educ Gerontol 35: 732-751.
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, et al. (2000) Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire.Psychol Assess 12: 210-224.
- American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, Fifth Edition, APA, Washington.
- Heckman TG, Kochman A, Sikkema KJ, Kalichman SC (1999) Depressive symptomatology, daily stressors, and ways of coping among middle-age and older adults living with HIV disease. J Ment Health Aging 5: 311-322.
- Hagengimana A, Hinton D, Bird B, Pollack M, Pitman RK (2003) Somatic panic-attack equivalents in a community sample of Rwandan widows who survived the 1994 genocide. Psychiatry Res 117: 1-9.
- van der Kolk BA, McFarlane AC, Weisaeth L (1996) Traumatic Stress: The effects of overwhelming experience on mind, body and society, Guilford Press, New York, London. 42: 17-41.