Journal of Geriatrics and Palliative Care
Download PDF
Case Report
*Address for Correspondence: Hamid R Okhravi, Glennan Center for Geriatrics and Gerontology, Department of Internal Medicine, Eastern Virginia Medical School, Norfolk, VA, USA, E-mail: okhravhr@evms.edu
Citation: Okhravi HR, Walia M, Palmer RM. Skin Angiosarcoma Masquerading as Hematoma in an Elderly Woman. J Geriatrics Palliative Care 2014;2(1):2.
Copyright © 2014 Okhravi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Geriatrics and Palliative Care | ISSN 2373-1133 | Volume: 2, Issue: 1
Submission: 04 November 2013 | Accepted: 27 February 2014 | Published: 03 March 2014
Skin Angiosarcoma Masquerading as Hematoma in an Elderly Woman
Hamid R Okhravi*, Meenal Walia and Robert M Palmer
- Glennan Center for Geriatrics and Gerontology, Department of Internal Medicine, Eastern Virginia Medical School, Norfolk, VA
*Address for Correspondence: Hamid R Okhravi, Glennan Center for Geriatrics and Gerontology, Department of Internal Medicine, Eastern Virginia Medical School, Norfolk, VA, USA, E-mail: okhravhr@evms.edu
Citation: Okhravi HR, Walia M, Palmer RM. Skin Angiosarcoma Masquerading as Hematoma in an Elderly Woman. J Geriatrics Palliative Care 2014;2(1):2.
Copyright © 2014 Okhravi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Geriatrics and Palliative Care | ISSN 2373-1133 | Volume: 2, Issue: 1
Submission: 04 November 2013 | Accepted: 27 February 2014 | Published: 03 March 2014
Case Presentation
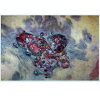
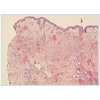
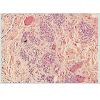
A 78 year old Caucasian, bed-bound, nursing home female,presented with non-tender, violaceous, indurated plaques of the skin of her anterior left thigh. Patient’s past medical history was significant for coronary artery disease, atrial fibrillation, diabetes mellitus type II, and stroke with left hemiplegia. On physical examination of her thigh, a 5X8 cm diffuse dusky red, woody hard, hematoma-like plaque was noted without inguinal lymphadenopathy or leg edema (Figure 1). Laboratory studies (comprehensive metabolic panel, complete blood count, and, coagulation factors) were unremarkable. Initial assumption was the lesions were hematomas, possibly secondary to trauma and heat packs were applied for patient comfort. Over the next two weeks, despite conservative management, the lesion on the anterior thigh extended to the lateral and posterior thigh. In addition, dark serous drainage appeared from 3-4 open areas (Figure 2). A vascular pathology rather than hematoma was suspected. Dermatology consultant performed a skin biopsy and initial results suggested a Kaposi sarcoma, but were not conclusive. HIV/AIDS studies were negative. A deeper second biopsy was conducted and favored the diagnosis of angiosarcoma. The diagnosis was further supported by a third biopsy showing the morphology of the spindle cells and negative HHV-8 staining, consistent with angiosarcoma (Figure 3 and Figure 4). Skin lesions continued to spread locally with emergence of more satellite lesions (Figure 5). Available treatment options including surgical, chemotherapeutic, and radiation interventions were discussed with the resident and daughter (medical power of attorney). Given the presence of multiple underlying co-morbidities, poor baseline functional status, and widespread local disease, resident elected not to pursue any further aggressive diagnostic or therapeutic options. At a meeting requested by the resident to review goals of care, she elected comfort care with hospice services. Due to the increased frequency of dressing changes from wound drainage, she expressed mild pain to hip which was treated effectively with Tramadol, prior to dressing changes. One month later, with daughter at bedside, the resident died comfortably.Discussion
Angiosarcomas are rare malignant tumors of endothelial originthat carry a poor prognosis and high tendency for local and metastatic spread [1]. The most common sites, in decreasing order, are the skin, breast, deep soft tissues, visceral organs and bone [2]. Cutaneous angiosarcoma is a great mimicker with many clinical presentations that include hematoma-like lesions, violaceous nodules and plaques. It is confined to the face and scalp region in more than 50% of cases [3]. It is an uncommon, malignant neoplasm that contains rapidly proliferating, extensively infiltrating anaplastic cells from blood vessels. Angiosarcomas in general have a similar distribution between sexes, can develop at any age, but are more common in older patients; with the cutaneous form most common in elderly white men [4-6]. Most angiosarcomas arise spontaneously, but there are a few reports of malignant transformation within pre-existing benign vascular lesions [7]. Radiotherapy is an independent risk factor, specifically in breast lesions [8]. Various chemicals such as vinyl chloride and thorium dioxide are associated with hepatic angiosarcomas [9,10]. Lymphedema is one of the well-known risk factors for the development of cutaneous angiosarcomas [11].Our patient had no known risk factors for angiosarcoma.Angiosarcomas have high rates of local recurrence and metastases in part because they are unrecognized or misdiagnosed [10], leading to a poor prognosis and a high mortality rate. Differential diagnoses of angiosarcoma include hemangioblastoma, Kaposi’s sarcoma, and metastatic cancer of unknown origin [12]. Histological features of angiosarcoma can vary among cases. The hallmark of angiosarcoma is malignant endothelial cells that are round, polygonal or fusiform and can have an epithelioid appearance. Angiosarcomas usually express endothelial markers such as von Willebrand factor, CD34, CD31, and vascular endothelial growth factor [10]. Immunohistochemistry is important in confirming the diagnosis of skin lesions.
The prognosis of cutaneous angiosarcoma was considered extremely poor in the past, with an overall 5-year survival rate less than 20% [13]. In recent years, several prognostic factors have been analyzed. Poor prognostic factors include old age, metastatic disease at presentation, poor patient performance status at baseline, presence of other soft-tissue sarcomas, large tumors (>5cm), and high tumor grade [1,14]. The site of the sarcoma is also important. Angiosarcoma of the viscera (liver, heart) and retroperitoneal disease have poorer outcomes [1]. Diagnosis relies on biopsy to confirm histology and MRI to delineate extent of primary lesion and endothelial markers. Treatment modalities are limited. For local disease, radical surgery with complete resection is the primary modality, complemented by adjuvant radiotherapy and, in some cases, adjunct chemotherapy. For metastatic disease, cytotoxic chemotherapy is the primary treatment modality [10].
In summary, cutaneous angiosarcoma of the elderly is a great mimicker with widely variable clinical presentations. This condition needs to be differentiated from several other common pathologies. The diagnosis may be challenging as illustrated in our case where several skin biopsies were required to ascertain the diagnosis of angiosarcoma of the skin. Given the poor prognosis of angiosarcoma in frail older patients, treatment options for extensive disease should include palliative care rather than aggressive interventions.
References
- Abraham JA, Hornicek FJ, Kaufman AM, Harmon DC, Springfield DS, et al. (2007) Treatment and outcome of 82 patients with angiosarcoma. Ann Surg Oncol 14: 1953-1967.
- Albores-Saavedra J, Schwartz AM, Henson DE, Kostun L, Hart A, et al. (2011) Cutaneous angiosarcoma. Analysis of 434 cases from the Surveillance, Epidemiology, and End Results Program, 1973-2007. Ann Diagnostic Pathology 15: 93-97.
- Holden CA, Spittle MF, Jones EW (1987) Angiosarcoma of the face and scalp, prognosis and treatment. Cancer 59: 1046-1057.
- Fury MG, Antonescu CR, Van Zee KJ, Brennan MF, Maki RG (2005) A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Cancer 11: 241-247.
- Rouhani P, Fletcher CD, Devesa SS, Toro JR (2008) Cutaneous soft tissue sarcoma incidence patterns in the U.S.: an analysis of 12,114 cases. Cancer 113: 616-627.
- Mark RJ, Poen JC, Tran LM, Fu YS, Juillard GF (1996) Angiosarcoma. A report of 67 patients and a review of the literature. Cancer 77: 2400-2406.
- Rossi S, Fletcher CD (2002) Angiosarcoma arising in hemangioma/vascular malformation: report of four cases and review of the literature. Am J Surg Pathol 26: 1319-1329.
- Huang J, Mackillop WJ (2001) Increased risk of soft tissue sarcoma after radiotherapy in women with breast carcinoma. Cancer 92: 172-180.
- Ron E (2003) Cancer risks from medical radiation. Health Phys 85: 47-59.
- Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ (2010) Angiosarcoma. Lancet Oncol 11: 983-991.
- Stewart FW, Treves N (1948) Lymphangiosarcoma in postmastectomy lymphedema; a report of six cases in elephantiasis chirurgica. Cancer 1: 64-81.
- Lahat G, Dhuka AR, Hallevi H, Xiao L, Zou C, et al. (2010) Angiosarcoma: clinical and molecular insights. Ann Surg 251: 1098-1106.
- Kempson RL, Fletcher CDM, Evans HL, Henrickson MR, Sibley RS. Tumors of the soft tissues. Atlas of tumor pathology. Third series. Fascicle 30. Washington, DC: Armed Forces Institute of Pathology; 2001.
- Fayette J, Martin E, Piperno-Neumann S, Le Cesne A, Robert C, et al. (2007) Angiosarcomas, a heterogeneous group of sarcomas with specific behavior depending on primary site: a retrospective study of 161 cases. Ann Oncol 18: 2030-2036.